PI-RADS Assessment
Based on the current uses and capabilities of mpMRI and MRI-targeted procedures, PI-RADS v2 defines clinically significant cancer on pathology as those tumors that have a Gleason score ≥ 7 (including 3+4 with a prominent, but not predominant, Gleason pattern 4 component) and volume > 0.5 cm3 or extraprostatic extension (EPE).
PI-RADS v2 has the following 5 assessment categories:
PI-RADS 1 Very low (clinically significant cancer is highly unlikely to be present)
PI-RADS 2 – Low (clinically significant cancer is unlikely to be present)
PI-RADS 3 – Intermediate (the presence of clinically significant cancer is equivocal)
PI-RADS 4 – High (clinically significant cancer is likely to be present)
PI-RADS 5 – Very high (clinically significant cancer is highly likely to be present)
The 5-point scale to score the imaging findings is based on the likelihood (probability) that a combination of mpMRI features on T2-weighted imaging (T2WI), diffusion weighted imaging (DWI), and dynamic contrast-enhanced (DCE) imaging represent the presence of a clinically significant cancer for an identified lesion in the prostate gland. To arrive at one of these 5 PI-RADS v2 assessment categories for each suspicious finding in the prostate, T2WI and DWI are each assessed using a 5-point scale, and DCE-MRI is classified as either positive or negative. Then, using the appropriate PI-RADS v2 table for either the peripheral zone (PZ) or the transition zone (TZ), these three parameters (for T2WI, DWI, and sometimes DCE-MRI) are integrated, and each lesion is assigned a PI-RADS v2 assessment category (PI-RADS 1–5) that indicates the likelihood that it is a clinically significant cancer.
It is important to note that there is a range of both malignant and benign histologies in the prostate gland, and at present there may be some overlap in their mpMRI characteristics. A PI-RADS v2 assessment category of PI-RADS 1 does not exclude the possibility of clinically significant cancer. Rather, it simply indicates that it is highly unlikely. Similarly, assessment category PI-RADS 5 does not provide proof that a lesion is a clinically significant cancer but rather indicates that it is highly likely. Currently, ranges of percent probabilities have not been assigned to each PI-RADS v2 assessment category. As PI-RADS v2 is tested and refined, this may become possible in the future.
Assignment to a specific PI-RADS v2 assessment category is based solely on mpMRI findings. It does not take into account other factors, such as serum prostate-specific antigen (PSA), digital rectal examination, patient history, or choice of treatment. However, these factors, along with local preferences, experience, and clinical history may determine recommendations regarding patient management, including biopsy.
6.3 Diffusion-Weighted Imaging Scoring
A score of 1 to 5 is assigned on DWI by comparing the signal intensity in a lesion to the average signal of normal prostate tissue in the histologic zone in which it is located. Nonetheless, the findings on DWI should always be correlated with findings on T2WI, T1WI, and DCE-MRI. ▶ Table 6.1 provides the criteria for assigning a score from 1 through 5 based on findings from DWI. Note that these criteria take into consideration: (1) lesion shape and margins; (2) signal intensity; (3) size; and (4) observations from both the high b-value images and the apparent diffusion coefficient (ADC) map. See ▶ Fig. 6.1 and ▶ Fig. 6.2 for examples.
DWI | T2WI | DCE | PI-RADS assessment category |
1 | Anya | Any | 1 |
2 | Any | Any | 2 |
3 | Any | – | 3 |
+ | 4 | ||
4 | Any | Any | 4 |
5 | Any | Any | 5 |
a “Any” means that any score from 1 to 5 on the 5-point scale can be assigned; “+” or “-” means positive or negative for contrast enhancement. Abbreviations: DCE, dynamic contrast-enhanced MRI; DWI, diffusion-weighted imaging; T2WI, T2-weighted imaging; PI-RADS, Prostate Imaging-Reporting and Data System v2. Source: Adapted from American College of Radiology (ACR) Prostate Imaging–Reporting and Data System, version 2. Available at www.acr.org. | |||

Fig. 6.1 PI-RADS assessment for peripheral zone on diffusion-weighted imaging (DWI). ADC, apparent diffusion coefficient; PI-RADS, Prostate Imaging–Reporting and Data System v2. (Adapted from the American College of Radiology [ACR] Prostate Imaging–Reporting and Data System, version 2. Available at www.acr.org.)
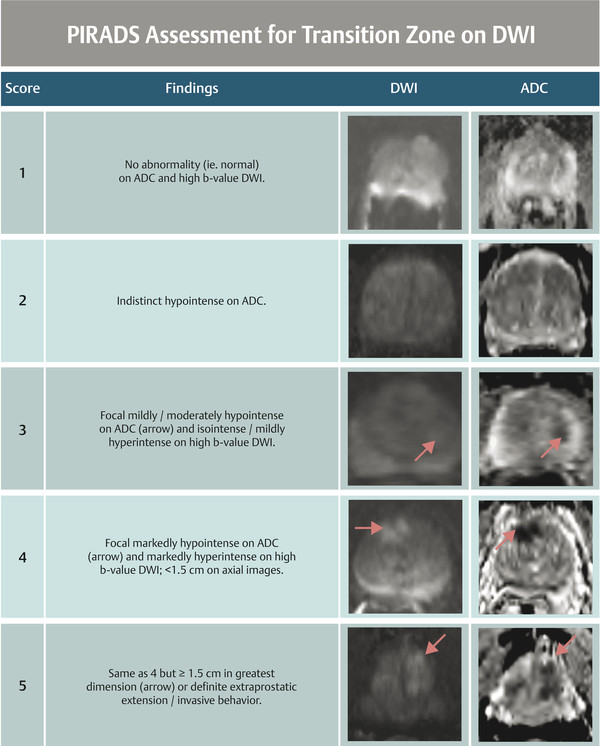
Fig. 6.2 PI-RADS assessment for transition zone on diffusion-weighted imaging (DWI). ADC, apparent diffusion coefficient; PI-RADS, Prostate Imaging–Reporting and Data System v2. (Adapted from the American College of Radiology [ACR] Prostate Imaging–Reporting and Data System, version 2. Available at www.acr.org.)
In the peripheral zone (PZ), assignment of a PI-RADS v2 assessment category for a lesion is based predominantly on the DWI score ( ▶ Table 6.1; ▶ Fig. 6.3).

Fig. 6.3 Flowchart for deriving final PI-RADS assessment category for peripheral zone lesion ADC, apparent diffusion coefficient; DWI. diffusion-weighted imaging; PI-RADS, Prostate Imaging–Reporting and Data System v2. (Adapted from American College of Radiology [ACR] Prostate Imaging–Reporting and Data System, version 2, 2015. Available at www.acr.org.)
For example, if the DWI score is 4 and the T2WI score is 2, then the PI-RADS assessment category should be 4. The only exception to this direct relationship of the DWI score and PI-RADS assessment category in the PZ is a positive (+) DCE score, which upgrades a DWI score of 3 to the final PI-RADS assessment category of 4 – high (clinically significant cancer is likely to be present). See section 6.5 DCE-MRI scoring for definitions of positive and negative scores for DCE-MRI.
Certain benign conditions display a focal hypointense ADC signal. Familiarity with these conditions and their typical MR appearance is essential for making the appropriate PI-RADS assessment. For example, although fibrosis, calculi, and hemorrhage are hypointense on both T2WI and ADC due to insufficient signal, they will also be markedly hypointense on all DWI images, essentially excluding clinically significant disease. Benign prostatic hypertrophy presents a greater challenge. Encapsulated, circumscribed, and round nodules in the TZ (transition zone) or PZ generally represent benign prostatic hyperplasia (BPH) or extruded BPH, respectively, regardless of their ADC/DWI signal. However, not uncommonly, BPH nodules may lack some or all of their benign morphological features and demonstrate marked ADC hypointensity, making assessment difficult. This remains a recognized limitation of mpMRI diagnosis and usually requires great expertise and experience on the part of the reader.
6.4 T2-Weighted Image Scoring
Scoring of T2WI also utilizes a 5-point scale, although the definitions of each score slightly differ between the PZ and TZ, as shown in ▶ Fig. 6.4 and ▶ Fig. 6.5.

Fig. 6.4 PI-RADS assessment for peripheral zone on T2-weighted imaging (T2WI). PI-RADS, Prostate Imaging-Reporting and Data System v2. (Adapted from American College of Radiology [ACR] Prostate Imaging–Reporting and Data System, version 2, 2015. Available at www.acr.org.)

Fig. 6.5 PI-RADS assessment for transition zone on T2-weighted imaging (T2WI). BPH, benign prostatic hyperplasia; PI-RADS, Prostate Imaging-Reporting and Data System v2. (Adapted from American College of Radiology [ACR] Prostate Imaging–Reporting and Data System, version 2, 2015. Available at www.acr.org.)
On T2WI, clinically significant cancers in the PZ usually appear as round or ill-defined hypointense focal lesions. It is important to note that many benign conditions may mimic this appearance, including prostatitis, hemorrhage, glandular atrophy, benign hyperplasia, biopsy-related scars, and post-hormonal therapy or post-ablation changes. Careful inspection of additional sequences may provide clues to the correct diagnosis.
TZ cancers are even more problematic. When benign prostatic hyperplasia (BPH) is present, the TZ is composed of variable amounts of glandular (T2-hyperintense) and stromal (T2-hypointense) tissue resulting in heterogeneous signal intensity. Identifying T2 hypointense cancer amongst the regions of benign stromal hyperplasia is challenging. Typical T2W features of TZ tumors that may prove useful include ill-defined moderate hypointensity (“erased charcoal” or “smudgy fingerprint” appearance), spiculated margins, lenticular shape, absence of a complete hypointense capsule, and invasion of the urethral sphincter and anterior fibromuscular stroma. The more features present, the higher the likelihood of a clinically significant TZ cancer.
Just as DWI is the dominant sequence for assigning an assessment category to a PZ lesion, T2WI is the primary determining sequence for a lesion in the TZ ( ▶ Table 6.2; ▶ Fig. 6.6): For example, if the T2WI score for a TZ lesion is 4 and the DWI score is 2, then the PI-RADS assessment category should be 4. Comparable to in the PZ, the only exception to this direct relationship between the T2WI score and the final PI-RADS assessment category occurs with the T2WI score of 3, in which case the DWI score serves as a tiebreaker (namely, a DWI score of 5 leads to an upgrade of a TZ lesion with a T2WI score of 3 to a PI-RADS assessment category of 4).
T2WI | DWI | DCE | PI-RADS assessment category |
1 | Anya | + or − | 1 |
2 | Any | + or − | 2 |
3 | ≤4 | + or − | 3 |
5 | + or − | 4 | |
4 | Any | + or − | 4 |
5 | Any | + or − | 5 |
a “Any” means that any score from 1 to 5 on the 5-point scale can be assigned; “+” or “-” means positive or negative for contrast enhancement. Abbreviations: DCE, dynamic contrast-enhanced MRI; DWI, diffusion-weighted imaging; T2WI, T2-weighted imaging; PI-RADS, Prostate Imaging-Reporting and Data System v2. Source: Adapted from American College of Radiology (ACR) Prostate Imaging–Reporting and Data System, version 2. Available at www.acr.org. | |||

Fig. 6.6 Flowchart for deriving final PI-RADS assessment category for transition zone lesion. BPH, benign prostatic hyperplasia; DWI, diffusion-weighted imaging; PI-RADS, Prostate Imaging-Reporting and Data System; T2WI, T2-weighted imaging. (Adapted from American College of Radiology [ACR] Prostate Imaging–Reporting and Data System, version 2, 2015. Available at www.acr.org.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree