Chapter 4 Radiation protection
Introduction
The biological effects of ionizing radiation are described in detail in Chapter 17 of this book, and are summarized in the following section. As there are known risks of radiation exposure, levels of acceptable risk have been specified by international expert groups, principally the International Commission on Radiological Protection (ICRP). Based upon these acceptable risks, dose levels have been recommended and in most cases adopted into national legislative requirements.
Biological effects of radiation
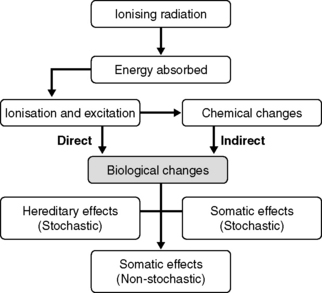
The block diagram (Figure 4.1) details the various biological effects that radiation may cause resulting from the absorption of energy associated with the radiation. As will be seen later, different areas of the body have different degrees of radiation sensitivity, which is mirrored in the fact that there are different dose limits for specific areas of the human body.
Stochastic hereditary effects
These effects are expressed not in the exposed individual but in the exposed individual’s subsequent offspring or future generations. Effects such as one eye a different colour from the other or, more grossly, one limb shorter or missing, are examples. Genetic defects appear in the population due to many causes, radiation being just one of them, with about one in 200 live births having a genetic defect expressed. As such, the possibility of radiation being the cause of any defect can only be shown statistically, the probability being dose dependent, rising with dose. The current risk estimated by ICRP 60 [1] of severe hereditary effects from radiation is one in 75 000 for a radiation dose of 1 mSv (see below), that is about 375 mSv would double the natural occurrence of genetic defects. That is from one in 200 to two in 200.
Stochastic somatic effects
These effects are expressed in the exposed individual in the form of cancer induction. Again, cancer has a number of causes, radiation being only one. About one in four of the population is likely to have a cancer in their lifetime. The probability of this being caused by radiation increases with dose. The current risk estimated by ICRP 60 [1] of a cancer from radiation is one in 13 000 for a radiation dose of 1 mSv (see below). The extra cancer risk from very low doses is extremely small and, in practice, undetectable in the population. However, the extra cancer risk at higher doses may be detectable using statistical methods. Even after high dose exposure, it is rarely possible to be certain that radiation was directly responsible for a cancer arising in an individual. There are a number of scientific uncertainties in making these estimates of cancer risk at low doses. In 2000, the highly respected United Nations Scientific Committee on the Effects of Atomic Radiation (UNSCEAR) [2] suggested that uncertainties in cancer risk estimates may be about twofold higher or lower for acute doses where cancer risk can be directly assessed and a further factor of two (higher or lower) for the projection of these risks to very low doses and low dose rates.
Non-stochastic somatic effects
These effects, sometimes known as deterministic, are expressed in the exposed individual in the form of acute effects of radiation such as radiation burns, hair loss, sterility, vomiting and diarrhoea. These effects will only occur once the level of dose received exceeds the threshold dose for that effect, with the severity of the effect increasing with dose beyond the threshold. Dependent on the area irradiated and the level of dose received, such effects will be displayed by patients undergoing radiotherapy exposures. A picture showing some of these effects is given in (Figure evolve 4.2![]() ). Details of dose thresholds that need to be exceeded for different effects are given in Table 4.1.
). Details of dose thresholds that need to be exceeded for different effects are given in Table 4.1.
Table 4.1 Dose thresholds for biological effects
| Threshold dose (Gy) | Area irradiated | Effect |
|---|---|---|
| >0.15 | Testes | Temporary sterility |
| >0.5 | Eye | Cataracts |
| >2.0 | Skin | Burns |
| >2.5 | Gonads | Permanent sterility |
| >20 | CNS | Death in hours |
Dose descriptors
The Gray is a measure of absorbed dose or energy in Joules per kilogram as described in Chapter 2. Two other quantities are relevant when discussing radiation protection matters, these are equivalent dose and effective dose which have the units of Sieverts to indicate a change in dose descriptor.
Equivalent dose
Radiation with a high LET (such as protons and alpha particles) is more likely than radiation with a low LET (such as x-rays or beta particles) to damage the small structures in tissue such as DNA molecules. This is because the energy from high LET radiation is absorbed in a small volume surrounding the trail of dense ionization produced by this radiation. The radiation weighting factor is directly related to the LET of the radiation. The radiation weighting factors are used to correct for differences in the biological damage to tissue caused by chronic exposure to different radiations (Table 4.2).
Table 4.2 Weighting factors for different types of radiation
| Radiation type and energy range | Radiation weighting factor (WR) |
|---|---|
| Photons – all energies | 1 |
| Electrons – all energies | 1 |
| Protons – energy >2 MeV | 5 |
| Alpha particles | 20 |
After ICRP60 [1]
Effective dose
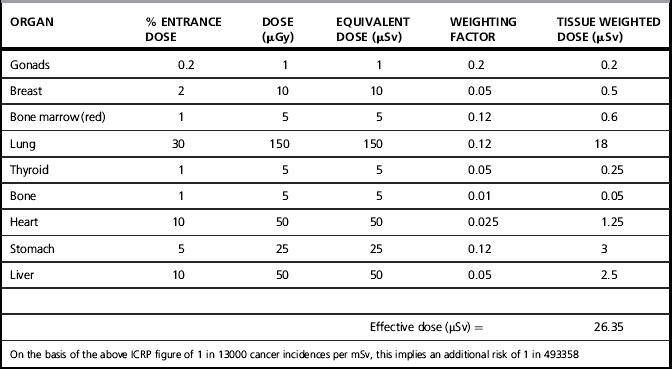
Equivalent dose accounts for the varying biological effects of different types of radiation on a particular tissue type or organ, T. However, it should come as no surprise to find out that the same radiation exposure to different parts of the body can have very different results. If the entire body were irradiated with a uniform beam of a single type of radiation, some parts of the body would react more dramatically than others. To take this effect into account, the ICRP have developed a list of tissue weighting factors, denoted WT, for a number of organs and tissues that most significantly contribute to an overall effective biological damage to the body. It should be noted that areas of the body with a high cell turnover are more radiosensitive than areas with a slower cell turnover and thus have a larger weighting factor. Table 4.3 presents values of the tissue-weighting factor WT based upon standard man which is a 70 kg male. Figures would be different for females, for instance, as they have more radiosensitive breast tissue. As such, the effective dose for a particular examination should not be viewed as a precise figure, but merely a figure giving an indication of relative risk.
| Tissue or body part | WT |
|---|---|
| Gonads | 0.20 |
| Bone marrow | 0.12 |
| Colon | 0.12 |
| Lung | 0.12 |
| Stomach | 0.12 |
| Bladder | 0.05 |
| Breast | 0.05 |
| Liver | 0.05 |
| Oesophagus | 0.05 |
| Thyroid | 0.05 |
| Skin | 0.01 |
| Bone surface | 0.01 |
| Remainder (adrenals, brain, upper large intestine, small intestine, kidney, muscle, pancreas, spleen, thymus, and uterus) | 0.05 |
| Total | 1.00 |
From [1]
To arrive at an effective dose for a particular examination, it is necessary to determine the equivalent dose to the different listed tissues or body parts, multiply these doses by the relevant tissue weighting factor and then sum the constituent parts. The units of effective dose are the Sievert and a worked example is given in Table 4.4.
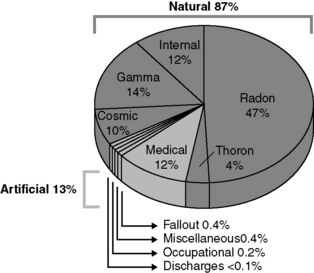
Background radiation
We are all exposed to radiation, regardless of our occupation, from ‘natural’ radiation sources in the environment and from man-made sources. We have no control over the level of exposure to these sources of natural radiation other than by choosing a particular lifestyle. For example, cosmic rays from outer space are attenuated by the Earth’s atmosphere and the more atmosphere there is the more the attenuation. This means that people who live at high altitudes or travel in high flying aircraft will get a greater radiation dose from cosmic rays. Other sources of natural radiation and the proportions that they contribute to the overall dose are shown in Figure 4.3.
Legislative requirements
The Ionising Radiations Regulations 1999 [3]
These revised the Ionising Radiations Regulations 1985 and deal with the protection of workers and members of the public from ionizing radiation from any source. The Approved Code of Practice – ‘Work with ionising radiation’ [4] – supports these. These documents are legally enforceable and breaches of their requirements could lead to prosecution by the regulators, normally the Health and Safety Executive. Good practice guidance is given in the Medical and Dental Guidance Notes [5]. The Ionising Radiations Regulations require three basic requirements to be met; these are:
1. that no practice involving radiation be adopted unless there is a positive net benefit, either to the exposed individuals or to society, i.e. it can be justified
2. all exposures must be As Low As Reasonably Achievable or Practicable. This is often referred to as the ALARA or ALARP principle. The principle requires that any particular source, the number of people being exposed, and the likelihood of incurring exposures where these are not certain to be received, be optimized to a minimum, taking account of social and economic factors. In practice, there may be a number of options where an assessment would show that costs are not grossly disproportionate. The option, or combination of options, which achieves the lowest level of residual risk, should be implemented, provided grossly disproportionate costs are not incurred. In general, the greater the risk, the more that should be spent in reducing it, and the greater the bias on the side of safety. The judgment as to whether measures are grossly disproportionate should reflect societal risk, that is to say, large numbers of people (employees or the public) being killed at one go. This is because society has a greater aversion to an accident killing 10 people than to 10 accidents killing one person each
3. dose equivalents to individuals do not exceed certain dose limits. The exposure of individuals resulting from the combination of all relevant practices should be subject to dose limits, or to some control of risk in the case of potential exposures. These are aimed at ensuring that no individual is exposed to radiation risks that are judged to be unacceptable from these practices in any normal circumstances.
Risk assessments
Prior to any work being undertaken with ionizing radiation, the employer is responsible for carrying out a risk assessment. This is in common with the requirement under the Management of Health and Safety at Work Regulations [6] to carry out risk assessments for other work involving hazards. The purpose of this risk assessment is to identify the measures needed to restrict the exposure of employees and other persons to ionizing radiation. The assessment must be suitable and sufficient enough to demonstrate that all hazards with the potential to cause a radiation accident have been identified and the nature and magnitude of the risks arising from those hazards have been evaluated. Where the risk assessment identifies a radiation risk, the employer must take all reasonable steps to prevent any such accident, limit the consequences of any accident that does occur and provide employees with the information, instruction and training to restrict their exposure. These risk assessments should normally be recorded and reviewed regularly to ensure their continued relevance. The factors that should be considered in performing a radiation risk assessment are given in the Approved Code of Practice [4] and include such things as the nature of the sources and the estimated radiation dose rates to which anyone can be exposed.
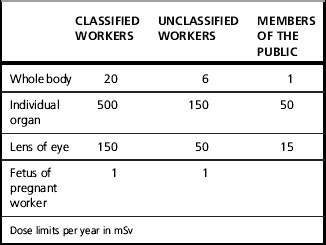
Dose limits
The annual dose limit has remained largely unchanged for the past 40 years and, despite the new dosimetric evidence, the absolute whole body dose limit per year remains at 50 mSv. However, such a level of dose is only allowable in special circumstances as the dose averaged over a 5-year period must not exceed 20 mSv per year for those occupationally exposed and aged over 18 years old. For those employees under 18 years old, the whole body dose limit is 6 mSv per year. Women of reproductive capacity working with ionizing radiation are subjected to a further dose constraint that the equivalent dose to the abdomen shall not exceed 13 mSv in any consecutive calendar quarter. The current dose limits are summarized in Table 4.5. It should be noted that there are currently no dose limits for patients undergoing examination or treatment with radiation, only that their doses must be as low as reasonably practicable and that any dose given must be justified in terms of the risk to the patient from not carrying out the exposure (see IRMER legislation [7] below).
There are two things to note in Table 4.5. First, there are different dose limits for different areas of the body, as different organs within the body have different radiosensitivities and radiation exposures are very often non-uniform. An area of the body with the quickest cell division and, therefore, the most radiosensitive is the fetus. This, in regulatory terms, is considered to be a member of the public from the point of the dose limit to be applied. A dose limit of 1 mSv to the fetus equates to a dose to the abdomen of the mother of about 2 mSv and is the limit that the employer has to apply for the declared term of the pregnancy. As such, the period of time for the dose limit to be exceeded starts when the worker declares herself to be pregnant to her employer. Secondly, there are three groups of people with different dose limits, classified workers, unclassified workers and members of the public. Classified workers are those workers who, by virtue of the work they undertake, are likely to exceed the dose limits for unclassified workers. Before a worker can be classified, they are required to be declared fit to do so by an appointed doctor. This is a registered medical practitioner who has been appointed in writing by the Health and Safety Executive (HSE). Once a worker has been classified, the employer is legally obliged to issue the worker with an individual radiation dosimeter and keep a cumulative dose record for 50 years of the last entry in it. This must be undertaken by an HSE approved dosimetry and record keeping service. An annual report is sent to a body known as the Central Index for Dose Information (CIDI) of the doses received by all classified persons, with the intention of being able to undertake epidemiological studies in subsequent years and to provide a central record of doses received by a classified worker which, if the worker changes employers, is passed onto their new employer. The reports of any investigation into a real or suspected overexposure of a member of staff or a patient must also be kept for 50 years. The Health and Safety Executive has defined an exposure significantly more than intended as being the reporting criteria to be used in determining if a patient has been overexposed due to equipment failure. This information is given in Appendix 2 of the Guidance Note PM77 [8] – ‘Equipment used in connection with medical exposure’. This specifies that notification to the HSE should be made if the dose given to a patient from beam therapy or brachytherapy exceeds 1.1 times the intended dose for a whole course or 1.2 times the intended dose for any fraction. For unsealed radionuclide therapy, the guideline multiple is 1.2 for any administration.
The whole body effective dose limit for all other persons including anyone below the age of 16 is 1 mSv per year with equivalent dose limits for specific areas in the body as detailed in Table 4.5.