Chapter 9 Radiation treatment planning
immobilization, localization and verification techniques
Introduction
• the size and shape of the PTVs
• the limiting (tolerance) dose to the critical structures (OAR)
• the positional reproducibility of the linear accelerator and couch support system
• limitation dictated by the patient’s position within the immobilization device
• selection of optimum beam parameters (e.g. field size collimator rotation).
Patient immobilization
Patient head shells
The majority of patients receiving radiotherapy to the head and neck region are immobilized using a custom made shell that accurately fits to provide effective and reproducible positioning of the head at all stages of planning and treatment. Typically, the process used to fabricate a clear plastic shell, Figure 9.1A requires a plaster cast of the patient’s head to be first produced. The transparency of the plastic enables the accuracy of fit to be checked with minor adjustments being made to ensure the shell must be a good fit, achieving the optimal position for treatment, while maintaining patient comfort.
Typically, the following steps are required to produce a full head shell:
1. the patient should assume the position to be adopted in the treatment room; this usually involves a headrest that supports the neck and inclines the head at the required angle for treatment. Separate impressions are taken of the front and back halves of the head
2. an impression of the back half of the patient’s head is made using, for example, plaster of Paris bandage or dental alginate, which covers an area up to a coronal plane at the level of the ears
3. before taking a similar impression of the front half of the head a few precautions are necessary to ensure patient comfort. The patient should breathe normally through the nose and ‘separating cream’ should be used on the skin to enable easy removal of the plaster cast. In some circumstances, a tissue-equivalent mouth insert will be required to depress and fix the tongue
4. the plaster bandage should be shaped carefully round the bony protuberances of the head in order to facilitate good fitting of the shell and to provide effective immobilization. The two plaster impressions front and back must fit uniquely together once they are removed from the patient. Further layers of plaster bandage are applied to the two halves to provide rigidity and, once hardened, are removed from the patient
5. the two halves are fixed together with further plaster bandage over the joints and the impression is filled with a thin mix of plaster and allowed to set overnight
6. the final solid cast is trimmed and sawn in half along a suitable coronal plane. The cast is now ready for vacuum forming
7. the flat surface of each half cast is placed on the vacuum forming machine. A large plastic sheet is heated and stretched into a bubble before the casts are raised and the vacuum applied to form a tight skin around the surface of the molds
8. the excess plastic is trimmed from each shell to provide a flange that enables the two halves to be held together with plastic press-studs. Side supports are molded and attached to the shell to enable it to be fixed to the treatment head support.
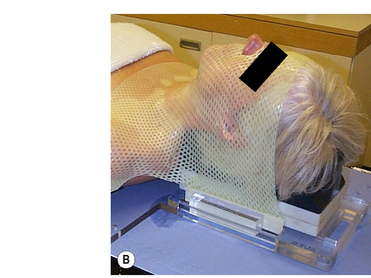
Thermoplastic shells
Commercial systems are now widely available that do not require vacuum forming techniques; these perforated thermoplastic materials may be softened in a hot-water bath or warm oven and shaped directly onto the patient, Figure 9.1B. This system utilizes a U-frame in which the attached thermoplastic, when heated and softened, stretches from the tip of the nose to the baseplate, where the U-frame is indexed and locked down. While this system is very easy to use and provides a snug fit for excellent fixation, it also can, in some cases, exhibit shrinkage, leading to patient discomfort due to the stretching of the thermoplastic required with this type of system. Stretching resulting from prolonged use during the course of treatment can lead to inaccuracies in set-up and, although here is a cost benefit from repeated use, sterilization requirements can limit this.
Stereotactic frames
Stereotactic frames were originally designed for stereotactic intracranial surgery, biopsy and electrode placement but have since been extensively adopted for radiosurgery head immobilization, Figure 9.1C. The high level of precision required for radiosurgery, such as Gamma Knife® and X-knife® systems, necessitates a means of relating three-dimensional patient image coordinates to 3D locations in frame coordinates to submillimeter accuracy. The most common system in use is the Leksell Stereotactic System® Frame which is rigidly attached to the patient’s head using four small screws placed with local anesthetic. The frame is shown in figure 9.1C. The frame provides the basis for target coordinate determination and is used to immobilize and position the patient’s head within the radiosurgery collimator helmet. The centre coordinates of the target volume are positioned at the intersection of the beams (from 200 cobalt sources for the Gamma Knife®) so that ‘target-centering’ is always achieved within this geometrically rigid system. Relocatable versions of the stereotactic frame are also available that are closer in design to the ‘head-arc fixation’ method.