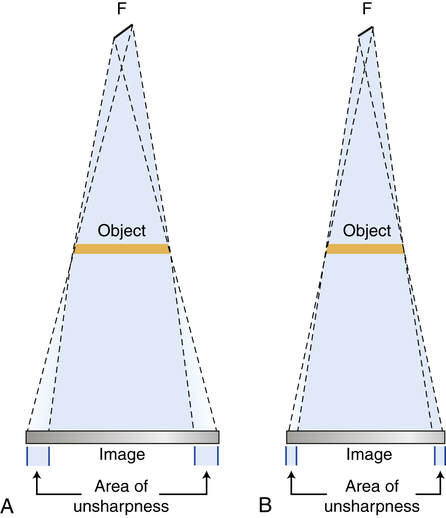
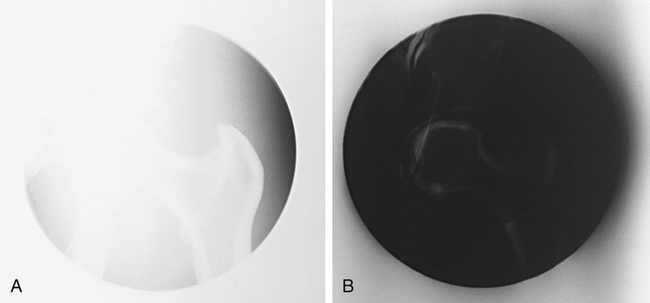
• Explain the relationship between milliamperage and exposure time with radiation production and image receptor exposure. • Calculate changes in milliamperage and exposure time to change or maintain exposure to the image receptor. • Compare the effect of changes in milliamperage and exposure time on film-screen and digital images. • Recognize how to correct exposure factors for a density error. • Explain how kVp affects radiation production and image receptor exposure. • Calculate changes in kVp to change or maintain exposure to the image receptor. • Recognize the factors that affect recorded detail and distortion. • Calculate changes in mAs for changes in source-to-image receptor distance. • Calculate the magnification factor and determine image and object size. • Describe the use of grids and beam restriction, and their effect on image receptor exposure and image quality. • Calculate changes in mAs when adding or removing a grid. • Recognize patient factors that may affect image receptor exposure. • Identify the exposure factors that can affect patient radiation exposure. • Differentiate between the types of exposure technique charts. • State exposure technique modifications for the following considerations: body habitus, pediatric patients, projections and positions, soft tissue, casts and splints, and pathologic conditions. mAs/distance compensation formula object-to-image receptor distance (OID) source-to-image receptor distance (SID) source-to-object distance (SOD) fixed kVp–variable mAs technique chart In Chapter 6, variables that affect both the quantity and quality of the x-ray beam are presented. Milliamperage and time affect the quantity of radiation produced and kilovoltage affects both the quantity and quality. Chapter 9 emphasizes that a good-quality radiographic image accurately represents the anatomic area of interest. The characteristics evaluated for image quality are density or brightness, contrast, recorded detail or spatial resolution, distortion, and noise. This chapter focuses on radiographic exposure techniques and the use of accessory devices, and their effect on the radiation reaching the image receptor (IR) and the image produced. Radiographers have the responsibility of selecting the combination of exposure factors to produce a quality image. Knowledge of how these factors affect the image individually and in combination assists the radiographer to produce a radiographic image with the amount of information desired for diagnostic interpretation. Once the anatomic part is adequately penetrated, as the quantity of x-rays is increased, the exposure to the IR proportionally increases (Figure 10-1). Conversely, when the quantity of x-rays is decreased, the exposure to the IR decreases. Therefore exposure to the IR can be increased or decreased by adjusting the amount of radiation (mAs). A patient’s age, condition, and the presence of a pathologic condition also affect the amount of mAs required for the procedure. Additionally, for a given mAs, IRs respond differently. For film-screen IRs, the mAs controls the density produced in the image. There is a direct relationship between the amount of mAs and the amount of density produced when using film-screen IRs. For example, when the mAs is increased, density is increased; when the mAs is decreased, density is decreased (Figure 10-2). When a film image is too light (insufficient density), a greater increase in mAs may be needed to correct the density, or the mAs may need to be decreased to correct a film image that has excessive density. This relationship between radiation exposure intensity and density is discussed in more detail in Chapter 9. The film characteristic, speed, and chemical processing determine the amount of optical density produced on the image for a given mAs. In general, for repeat radiographs necessitated by density errors, the mAs is adjusted by a factor of 2; therefore a minimum change involves doubling or halving the mAs. This typically brings the optical densities back within the straight-line portion of the film’s sensitometric curve to best visualize the anatomic area of interest. As mentioned previously, it may take more than doubling the mAs to correct for a density error. If the radiograph necessitates an adjustment greater than a factor of 2, the radiographer should multiply or divide the mAs by 4 (Figure 10-3). However, the kVp has a greater effect on the image when using film-screen IRs. Increasing the kVp increases IR exposure and the density produced on a film image, and decreasing the kVp decreases IR exposure and the density produced on a film image (Figure 10-4). For film-screen IRs, kVp has a direct relationship with density; however, the effect of the kVp on density is not equal throughout the range of kVp (low, middle, and high). A greater change in the kVp is needed when operating at a high kVp (greater than 90) compared with operating at a low kVp (less than 70) (Figure 10-5). Altering the penetrating power of the x-ray beam affects its absorption and transmission through the anatomic tissue being radiographed. Higher kVp increases the penetrating power of the x-ray beam and results in less absorption and more transmission in the anatomic tissues, which results in less variation in the x-ray intensities exiting the patient (remnant). As a result, images with lower contrast are produced (Figure 10-6). When a low kVp is used, the x-ray beam penetration is decreased, resulting in more absorption and less transmission, which results in greater variation in the x-ray intensities exiting the patient (remnant). This produces a high-contrast radiographic image (Figure 10-7).
Radiographic Exposure Technique
Introduction
Primary Factors
Milliamperage and Exposure Time

As the quantity of x-rays is increased (mAs), the exposure to the image receptor proportionally increases.

Changes in mAs have a direct effect on density. A, Original image. B, Decreased in density when the mAs is decreased by half. C, Increase in density when the mAs is doubled. (From Fauber TL: Radiographic imaging and exposure, ed 3, St Louis, 2009, Mosby.)
A, A greater increase in mAs, four times the original mAs, is needed. B, A greater decrease in mAs, one-fourth the original mAs, is needed. (From Fauber TL: Radiographic imaging and exposure, ed 3, St Louis, 2009, Mosby.)
Kilovoltage
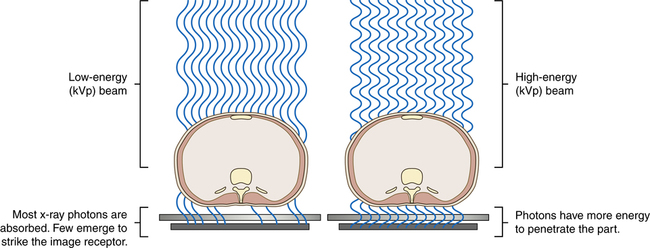
Increasing the kVp increases the penetrating power of the radiation and increases the exposure to the image receptor.
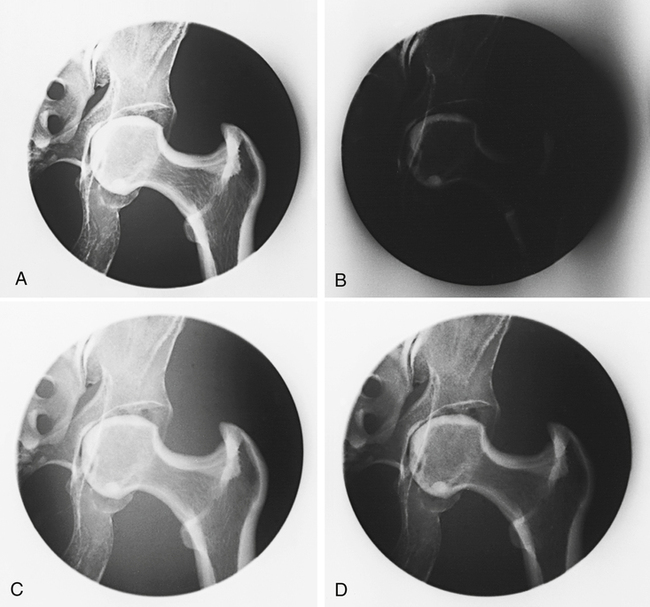
Produced at 50 kVp (A) and produced at 90 kVp with the mAs adjusted to maintain radiographic density (C). A 10-kVp increase at 50 kVp (B) produces a greater change in density than a 10-kVp increase at 90 kVp (D). (From Fauber TL: Radiographic imaging and exposure, ed 3, St Louis, 2009, Mosby.)
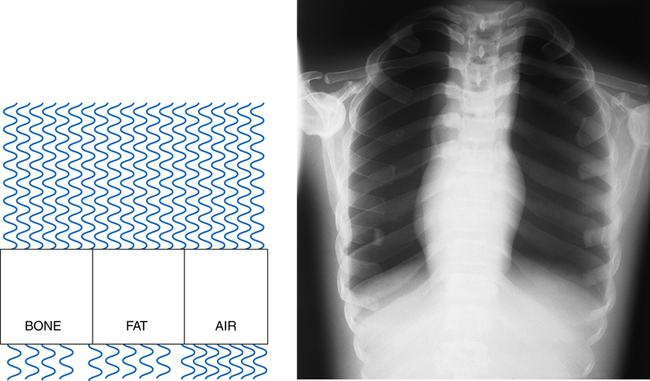
Higher kVp increases the penetrating power of the x-ray beam and results in less absorption and more transmission in the anatomic tissues, which results in less variation in the x-ray intensities exiting the patient. As a result, images with lower contrast are produced. (From Fauber TL: Radiographic imaging and exposure, ed 3, St Louis, 2009, Mosby.)
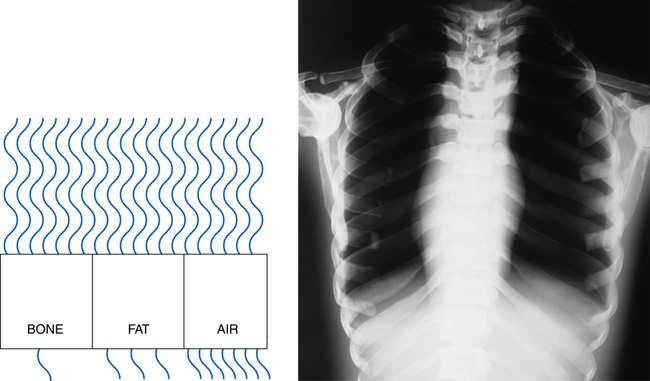
Lower kVp decreases the x-ray beam penetration, resulting in more absorption and less transmission, which results in greater variation in the x-ray intensities exiting the patient. As a result, images with higher contrast are produced. (From Fauber TL: Radiographic imaging and exposure, ed 3, St Louis, 2009, Mosby.)
Radiographic Exposure Technique