Conventional radiography, including routine views (specific for various body parts), special views, and stress views
Digital radiography, including digital subtraction arthrography (DSa) and angiography (DSA).
Fluoroscopy, alone or combined with videotaping
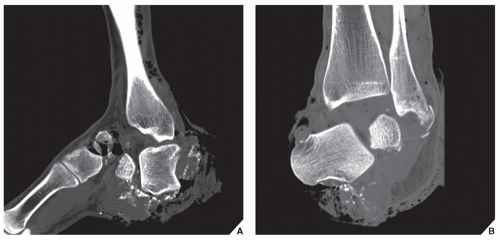
Computed tomography (CT)
Arthrography, tenography, and bursography
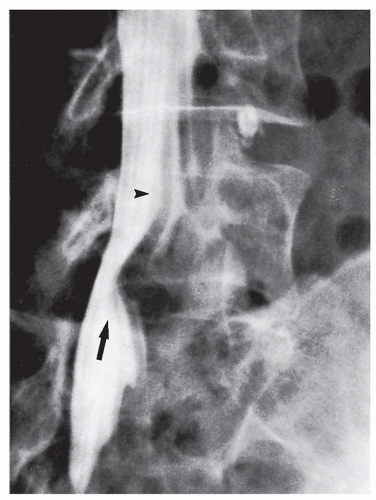
Myelography and diskography
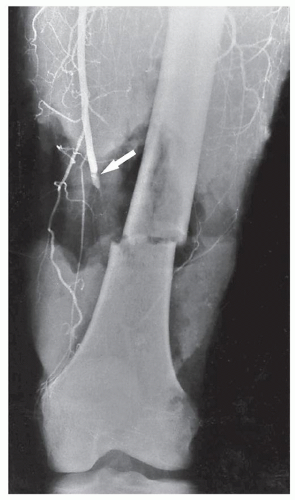
Angiography (arteriography and venography)
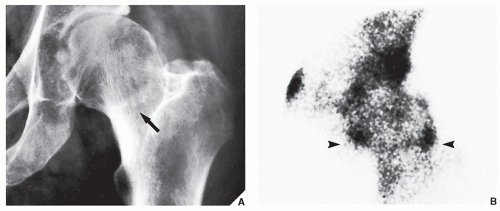
Scintigraphy (radionuclide bone scan)
Ultrasonography (US)
Magnetic resonance imaging (MRI)
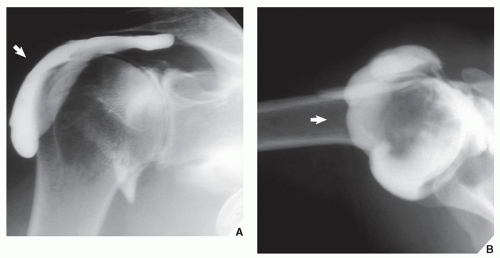
tibialis anterior and posterior, and flexor digitorum longus. Bursography of the subacromial-subdeltoid bursae complex occasionally demonstrated a partial or full-thickness tear of the rotator cuff.
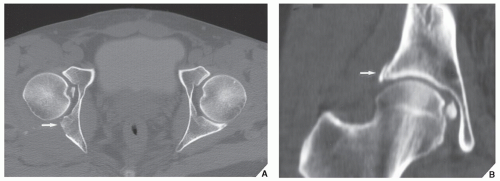
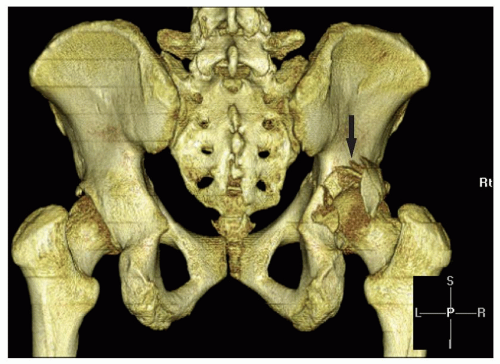 FIGURE 4.9 Fracture of the acetabulum. 3D CT reconstructed image shows distinctive features of a fracture of the posterior wall of the right acetabulum (arrow). |
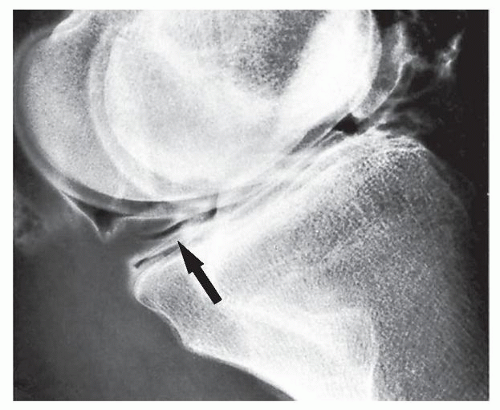 FIGURE 4.11 Tear of the medial meniscus. In this patient, double-contrast arthrography of the knee shows a horizontal cleavage tear in the posterior horn of the medial meniscus (arrow). |
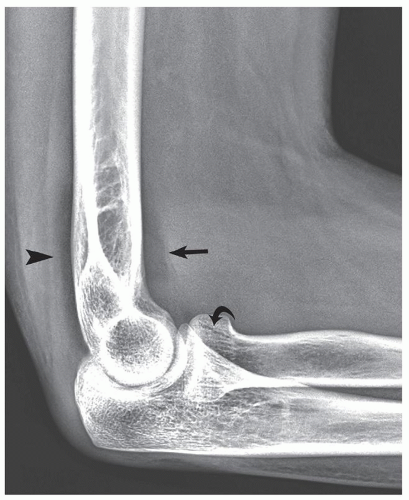
arthroscopies are avoided. MRI is probably the only imaging modality that can demonstrate so-called bone contusions (see Fig. 2.39). These abnormalities consist of posttraumatic marrow change resulting from a combination of hemorrhage, edema, and microtrabecular injury. Meniscal injuries, such as bucket-handle tears, tears of the free edge, and peripheral detachments, can be accurately diagnosed. Other subtle abnormalities of various structures and posttraumatic joint effusion can also be well visualized (Figs. 4.16 and 4.17). Similarly, the medial and lateral collateral ligaments, anterior and posterior cruciate ligaments, and tendons around the knee joint can be well demonstrated (see Figs. 9.14 and 9.15) and abnormalities of these structures can be diagnosed with high accuracy. In the shoulder, impingement syndrome and complete and incomplete rotator cuff tears may be effectively diagnosed most of the time (Fig. 4.18). Traumatic lesions of the tendons (such as biceps tendon rupture), traumatic joint effusions, and hematomas are easily diagnosed with MRI. Likewise, this modality is effective to diagnose a tear of the cartilaginous labrum. The
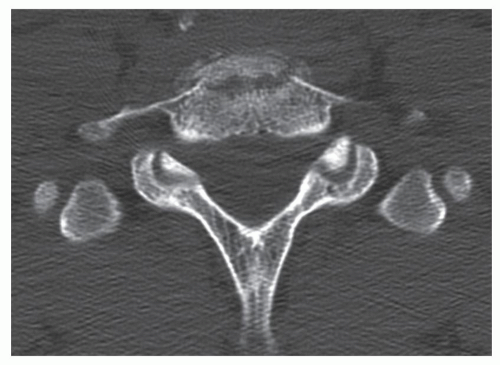
changes of osteonecrosis at various sites, particularly in its early stage, may be detected by MRI when other modalities, such as conventional radiography and even radionuclide bone scan, may be normal. MRI of the ankle and foot has been used among others in diagnosing tendon ruptures and posttraumatic osteonecrosis of the talus. In the wrist and hand, MRI has been successfully used in the early diagnosis of posttraumatic osteonecrosis of the scaphoid and Kienböck disease. MRI is strongly advocated as the technique of choice in the evaluation of abnormalities of the triangular fibrocartilage complex, although arthrography, particularly in conjunction with digital imaging and CT, is also a very effective modality. The greatest use of MRI is for evaluating trauma of the spine, the spinal cord, the thecal sac, and nerve roots, as well as for evaluating disk herniation (see Fig. 11.105). MRI is also useful in the evaluation of spinal ligament injuries. The demonstration of the relationship of vertebral fragments to the spinal cord with direct sagittal imaging is extremely helpful, particularly to evaluate injuries in the cervical and thoracic areas.
 FIGURE 4.16 Chondral defects. Axial proton density-weighted fat-saturated MRI of the knee demonstrates subtle defects in the articular cartilage of the right patella (arrows). |
Diagnosing and evaluating the type of fracture or dislocation
Monitoring the results of treatment and looking for possible complications
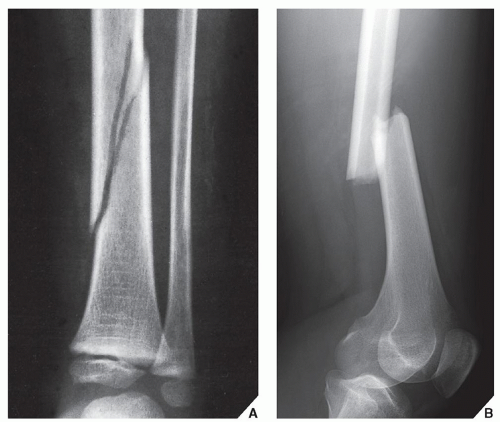
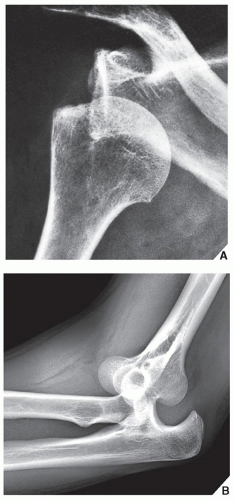
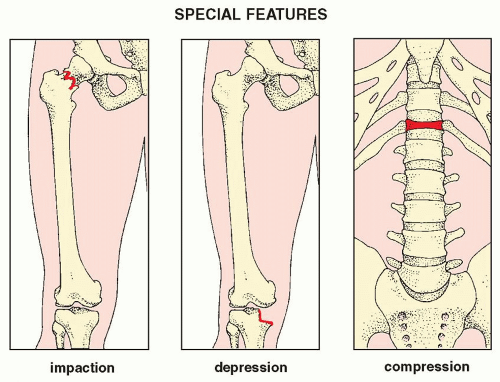
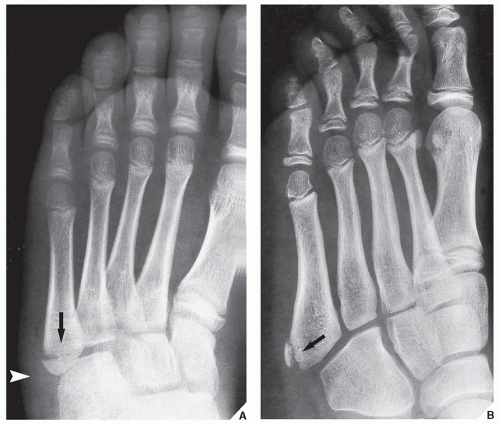
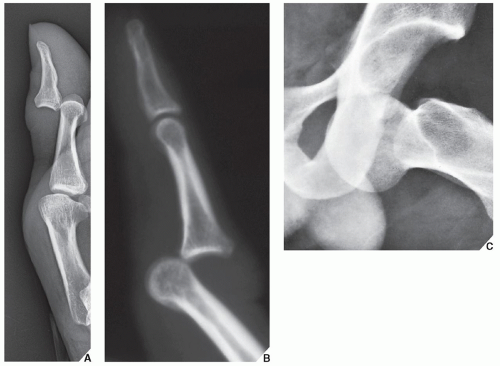
to the longitudinal axis of the bone (Fig. 4.27); (e) the presence of special features such as impaction, depression, or compression (Fig. 4.28); (f) the presence of associated abnormalities such as a fracture with concomitant dislocation or diastasis (Fig. 4.29); and (g) special types of fractures that may occur as the result of abnormal stress or secondary to pathologic processes in the bone (Fig. 4.30). The distinction between an open (or compound) fracture, one in which the fractured bone communicates with the outside environment through an open wound (Fig. 4.31), and a closed (or simple) fracture, one that does not produce an open wound in the skin, should preferably be made by clinical rather than radiographic examination.
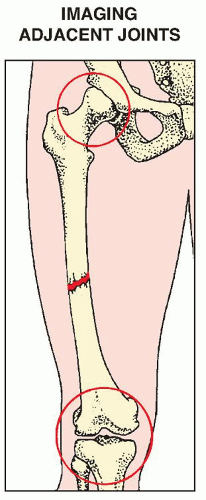 FIGURE 4.23 Adjacent joints. The radiograph of a suspected fracture of the femoral shaft should include the hip and knee articulations. |
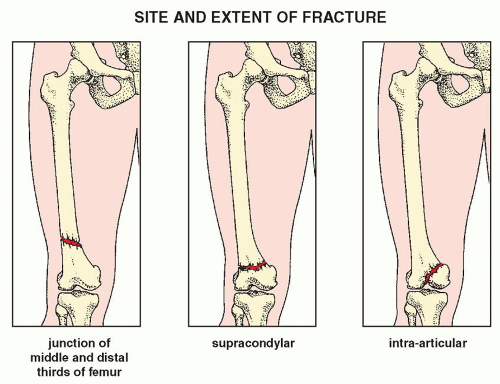 FIGURE 4.24 Site and extent. Factors in the radiographic evaluation of a fracture: the anatomic site and extent. |
 FIGURE 4.26 Alignment. Factors in the radiographic evaluation of a fracture: the alignment of the fragments. |
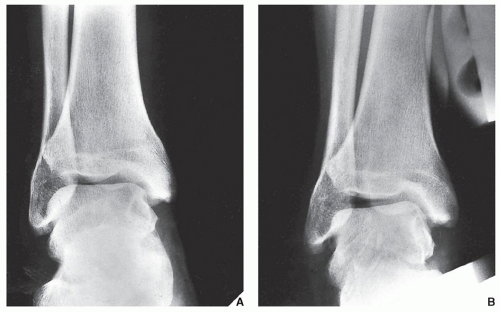
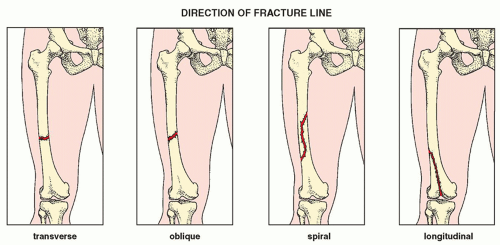 FIGURE 4.27 Direction. Factors in the radiographic evaluation of a fracture: the direction of the fracture line. |
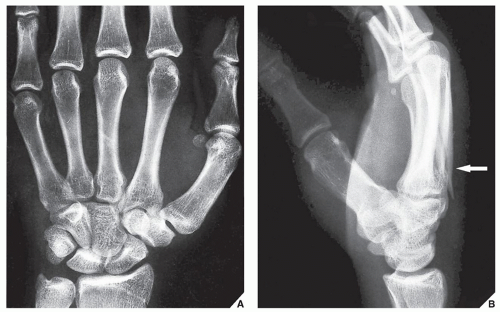
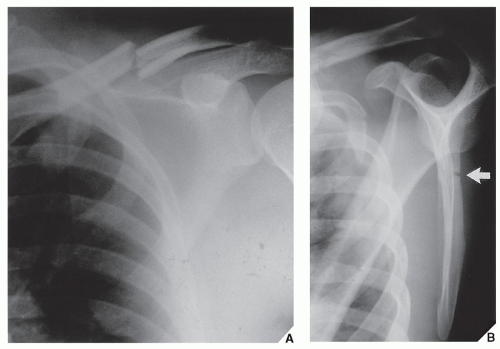
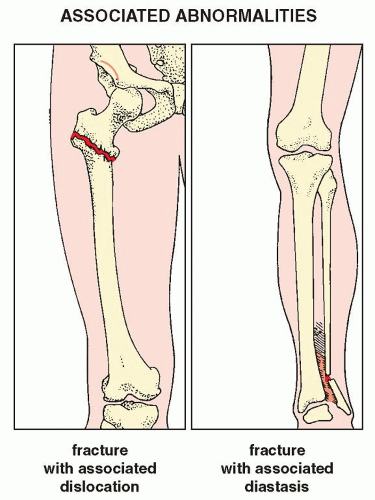 FIGURE 4.29 Associated abnormalities. Factors in the radiographic evaluation of a fracture: associated abnormalities. |
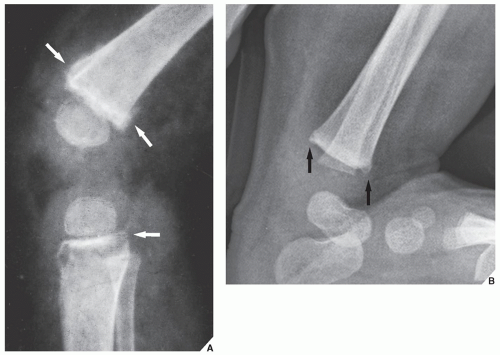
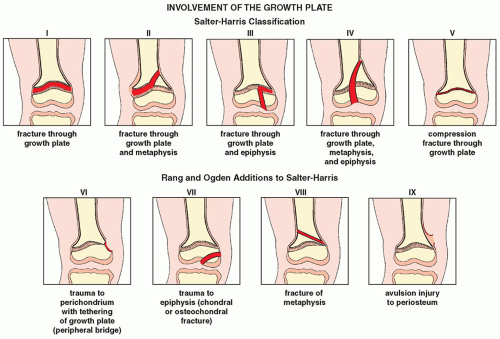 FIGURE 4.32 Classification of the growth plate injuries. The Salter-Harris classification of injuries involving the growth plate (physis) together with Rang and Ogden additions. |
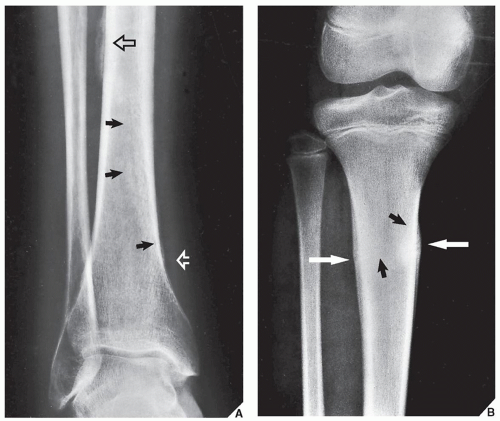
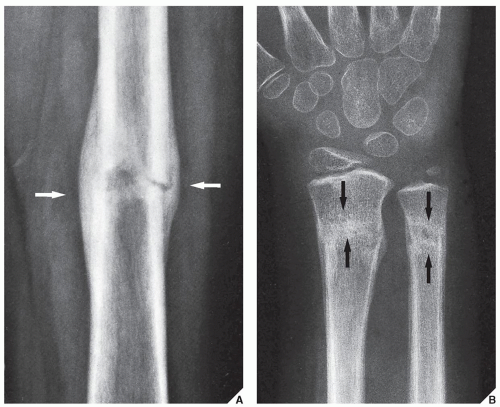
and compact bone. For the radiologist evaluating follow-up radiographs, the primary indication of bone repair is radiographic evidence of periosteal (external) and endosteal (internal) callus formation (Fig. 4.45). This process, however, may not be radiographically apparent in the early stage of healing. Periosteal response may not be visible on radiographs at sites where there is an anatomic lack of periosteum, for example, in the intracapsular portion of the femoral neck. Likewise, radiographs may not demonstrate endosteal callus formation because the callus contains only fibrous tissue and cartilage, which are radiolucent. At this early stage of healing, a fracture may be clinically united, that is, shows no evidence of motion under stress, yet radiographically, the radiolucent band between the fragments may persist (Fig. 4.46A). As the primary temporarily radiolucent callus is gradually converted by the process of endochondral ossification to more mature lamellar bone, it is seen on the film as a dense bridge (Fig. 4.46B). This constitutes radiographic union.
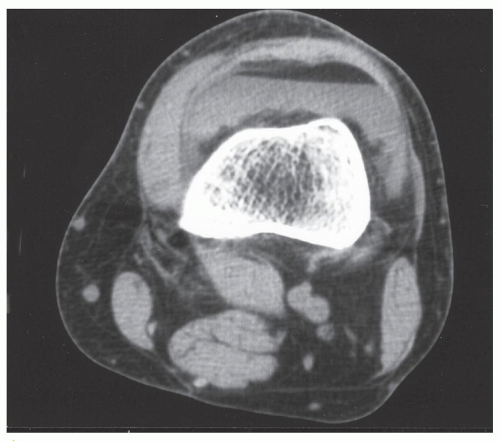 FIGURE 4.39 FBI sign on CT. Axial CT section through the knee joint shows an FBI sign in a patient with tibial plateau fracture (not seen on this image). |
TABLE 4.1 Factors Influencing Fracture Healing | ||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
TABLE 4.2 Fracture Healing | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
 FIGURE 4.48 Nonunion. A fracture of the proximal fibula failed to unite. Note the gap between the fragments, the complete lack of callus formation, and the rounding of the fragment edges. |
TABLE 4.3 Causes of Nonunion | ||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree