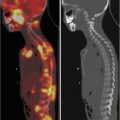
Fig. 8.1
99mTc-MDP scan. (a): Whole-body anterior and posterior views of a 10-year-old male. Left leg correctly positioned shows well-defined tibia and fibula; right leg slightly extra rotated, due to an inflammatory lesion in the proximal tibial metaphysis, shows superimposition of the two bones. (b) Normal multiple static whole-body scan of a 3-year-old male with good overlap of the field of views, limbs correctly positioned. Note the faint shine-through of the costochondral junctions in the chest posterior view
Three-phase technique is strongly recommended, independently from the clinical problem, because increases information throughput at no added irradiation cost. Blood flow images must be aimed to the body segment most suspicious, if no radiological or clinical localization is available, or otherwise targeted on the culprit site. A 1-s framing time for a total of 90 s, 128 × 128 matrix, is adequate. Blood pool images should encompass the whole body and may be acquired also with a relatively fast (5–10 min) whole-body scan [6].
8.3 Sedation
Bone scan images are very sensitive to movement artifact. Normally children above 6 years of age are able to stay still for the time required; velcro straps, sandbags, video, and cooperative parents normally are sufficient for younger children [7]. A careful, friendly explanation of the procedure is of paramount importance in acquiring child and parents’ cooperation. In babies below 15 kg, oral chloralium hydrate, up to 50 mg/kg, at least 20 min. before the scan, may provide light sedation. Nevertheless, every time a pharmacological intervention is necessary, this must be performed according to the institutional guidelines and under the maximum safety schedule [8].
8.4 SPET/TC
The birth of hybrid systems fulfilled the dream of nuclear medicine to be able to precisely allocate RF distribution into an anatomical detailed map. Of course, when dealing with bone diseases, the CT component of the image carries independent, very valuable information, not hampered at all by the lack of contrast media administration. In pediatric age, on the other hand CT scan increases the radiation burden, and the tube setting parameters must be carefully optimized to minimize this increase, taking into account the natural high contrast of bone tissue and reducing the scan field according to the abnormalities of uptake observed in the scintigraphic image [9]. We must at end be aware that CT cannot solve every diagnostic problem and sometimes it is wiser to not perform SPET/CT when the clinical context strongly suggests the need for an MRI (Fig. 8.2).
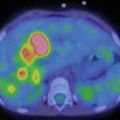
Fig. 8.2
Three-phase bone scan of a 2.5-year-old limping female. A previous spine MRI under sedation was normal. Blood flow phase aimed at the knee (not shown) unremarkable. Whole-body blood pool (a, b) images showed increased blood content at the left sacroiliac joint. Bone phase (c) confirmed the finding. SPET/CT not performed, MRI suggested for possible space-occupying lesion. Osteoarthritis of the left sacroiliac joint confirmed thereafter
8.5 Caveat and Pitfalls
Bone-seeking RF are all actively excreted by the urinary system. Children must be encouraged to drink or breastfeed. Every potentially contaminated dressing (diapers, underwear, etc.) must be removed before the scan and toilet-trained children invited to void. Injection site, especially if an intravenous stable access was used, should be recorded, for avoiding misinterpretation. It is better to not use central venous catheters.
During the skeletal development many growth plates are visible; their location must be known by the interpreting physician for avoiding misinterpretation. Beware also the “shine-through” phenomenon, i.e., the visibility of a focus of uptake on both opposite (e.g., either anterior or posterior) images.
8.6 Clinical Indications
Bone space-occupying lesions are normally detected by X-rays, serendipitously or because of local pain [10]. They are classified according to their calcium content and their impact on the bone integrity. Bone scan easily allows to distinguish between stable lesions and growing ones, according to the intensity of the RF uptake. Osteomas (bone islands), osteopoikylosis, simple bone cysts, non-ossifying fibromas and enchondromas in the majority of cases show faint or unremarkable peripheral uptake, except when they undermine the integrity of the cortex (Fig. 8.3). Aneurismal bone cysts, fibrous dysplasia areas, osteoid osteomas and osteoblastomas are characterized by increased uptake, the latter two very intense. SPET/TC is very useful for studying these lesions and can become a “one stop shop” (Fig. 8.4) for the detection of osteoid osteoma [11], due to the ability of detecting the nidus, efficiently integrating the data obtained with MRI [12]. Dealing with lesions, like fibrous dysplasia or chronic recurrent multifocal osteomyelitis (CRMO) [13], often multiple, bone scans still represent the more efficient whole-body survey available.
Fig. 8.3
A 12-year-old female with pain at the right foot. Plain X-ray film showed osteolytic lesion of likely benign meaning (non-ossifying fibroma). SPET/CT (a MIP image, b fused selected slices, c pure CT slices) showed high uptake on the lateral part of the lesion, suggesting cortical painful erosion. Curettage performed
Fig. 8.4




(a) A 16-year-old male with pain at the right foot. Plain X-ray film reported as unremarkable. SPET/CT (a) SPET sagittal images, (b) fused sagittal images, clearly showed high uptake at the proximal head of the II metatarsal bone. (b) The CT section delineated the presence of a dense lesion with radiolucent core: osteoid osteoma. Radiofrequency ablation performed
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree