DOTATATE
DOTATOC
Age
60.2 ± 9.1 years
45.3−75.2 years
Activity per cycle (GBq)
6.5 ± 1.1
7.3 ± 0.7
5.0−9.5
5.5−8.5
Table 2
Risk factors present in the patient group
Risk factor | No. of patients |
|---|---|
Hypertension | 9 |
Diabetes | 2 |
Age more than 65 years | 4 |
2.2 Radiopharmaceuticals
The radiopharmaceuticals were prepared in our own radio pharmacy. 177Lu-labeling of DOTA-peptides was done according to the general procedure: A solution of 500 μg 2,5-dihydroxybenzoic acid and 50 μg of the corresponding DOTA peptide in 50 μL 0.4 M sodium acetate buffer (pH 5.5) was added to a solution of 1 GBq in 30 μL 0.05 M HCl. The mixture was heated to 90°C for 30 min and then diluted with 0.9% saline solution followed by sterile filtration. Quality control settings were the following: RP-18-HPLC, solvent A: water; solvent B: acetonitrile (both with 0.1% TFA); gradient: 0–2 min 100% A, 20 min 100% B; flow rate: 1.2 mL/min; column: LiChrospher 100RP 18EC-5 μm 250 × 4 mm. The radiochemical purity was greater than 99.5%.
2.3 Infusion and Renal Protection
For kidney protection, every patient was co-infused with 1,500 mL of a renoprotective amino acid mixture of 5% lysine HCL and 10% l-arginine HCL in 250 mL NaCl at pH 7.4 and osmolarity of 400 mosmol/l. This infusion was started 30 min prior to administration of the therapeutic dose and continued for 4 h. The radiopharmaceutical was co-administered over 10–15 min by using a second infusion pump system. This co-infusion of amino acids reduces renal exposure and allows for higher mean absorbed doses to reach tumors (Jamar et al. 2003).
The activity to administer was chosen based on the general status of the patient (e.g., Karnofsky scale), kidney function, hematologic reserve, tumor mass and SSTR expression, previous treatments, and also experience reported by other groups (Kwekkeboom et al. 2005).
2.4 Monitoring of Renal Function
In all patients undergoing PRRNT, follow-up of renal function was carried out after each cycle after a period of 6–12 months with serum creatinine and BUN. GFR was determined using 110–185 MBq 99mTc-DTPA before and every 3–4 months after therapy, and the tubular extraction rate (TER) determined using 99mTc-MAG3 was also documented.
2.5 Dosimetry
Dosimetric calculations were performed according to the MIRD scheme from 2D planar whole image sets (Bolch et al. 2009). The time-dependent activity was determined based on conjugated planar whole-body scans acquired 0.5, 3, 20–24, 44–48, and 68–72 h post injection. For estimation of mean absorbed doses, we used a well-established dosimetry protocol, as was used in a previous study (Wehrmann et al. 2007).
2.6 Comparison and Statistics
The dosimetric parameters determined for kidneys in addition to the mean absorbed dose were uptake, half life, residence time, and tumor-to-kidney ratio. Pre- and post-therapy serum creatinine, GFR, and TER were also compared. The effect of age, diabetes, hypertension, and total administered activity on renal function was determined. For evaluation of statistically significant differences, nonparametric signed-rank tests for paired samples were used. All statistical tests were performed using ORIGINPRO 8.1G; p-values ≤ 0.05 were considered to be significant.
3 Results
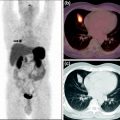
The dosimetric parameters for kidneys were determined in 22 patients for both DOTATATE and DOTATOC (Fig. 1). Renal uptake, residence time, and mean absorbed dose per unit administered activity showed higher values for DOTATATE in 19 of 22 patients (86%, p < 0.05). These results were statistically significant. Only half-life was found to be similar for both peptides, where 12 patients (55%) showed longer half-life for DOTATATE (p > 0.05).
Fig. 1
Comparison of renal dosimetry parameters for DOTATATE and DOTATOC
Tumor-to-kidney ratio was higher for DOTATOC in 23 of 43 (53%) lesions measured; however, this difference was not statistically significant (p > 0.05).
There were no statistically significant changes in GFR (Fig. 2a), TER (Fig. 2b), or serum creatinine (Fig. 2c) pre and post-therapy with either DOTATATE or DOTATOC (p > 0.1). Five of the 22 patients had mild elevation in serum creatinine, of whom 3 had history of hypertension, 1 had diabetes mellitus, and 1 was aged >65 years. In none of these five patients did any significant fall in serum creatinine occur post-therapy. Thus, no significant changes in renal function were observed in any of the patients irrespective of the amount of administered radioactivity and peptide used for PRRNT.
Fig. 2




Comparison of pre- and post-therapy renal parameters in patients treated with DOTATOC and DOTATATE: a GFR, b TER, and C serum creatinine
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree