Fig. 11.1
MRA examination reconstructed with the MIP technique of the abdominal aorta and renal arteries on the coronal (a) and axial (b) planes. The right renal artery has an early bifurcation (arrow)
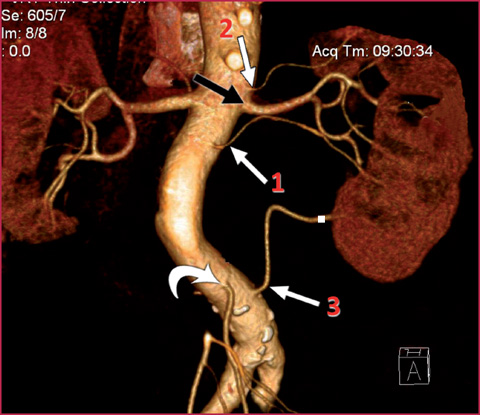
Fig. 11.2
3D Volume Rendering (VR) reconstruction of the abdominal aorta and renal vessels. On the left, it is easy to recognize four renal arteries: the main renal artery (black arrow), an accessory branch (1) and two polar branches, one for the upper pole (2) and the other for the lower pole (3). The branch to the lower pole originates near the aortic junction, distal to the origin of the inferior mesenteric artery (curved arrow)
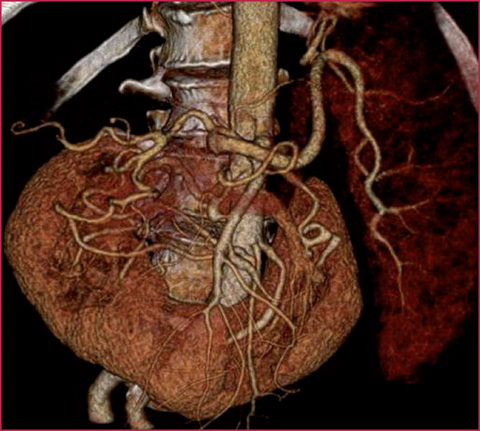
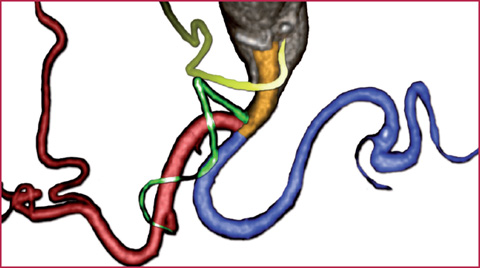
Fig. 11.3
3D VR reconstruction of the abdominal aorta and renal vessels. Presence of horse-shoe kidney and numerous arteries that supply the renal parenchyma
Accessory renal arteries are the most common cause of compression of the ureteropelvic junction and they may be accidentally damaged in every abdominal surgical procedure, especially when the laparoscopic technique is used. Detection of these branches is therefore mandatory, especially in pre-surgical evaluation (Fig. 11.4).
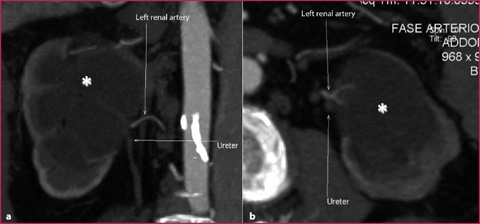
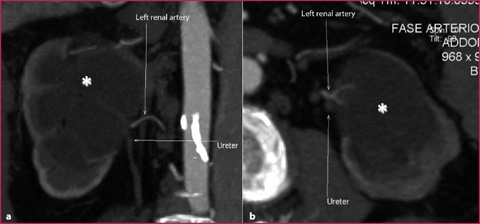
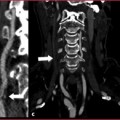
Fig. 11.4
CT-angiography reconstructed with the MIP technique on the coronal (a) and axial (b) planes. Hydronephrosis of the left kidney (asterisks) due to renovascular conflict between the ureter and accessory renal artery
Celiac Axis
The celiac axis is the first collateral branch of the abdominal aorta and arises from the ventral surface of the aorta immediately after the diaphragm (Fig. 11.5, Table 11.1).
Table 11.1
Celiac trunk branches
Celiac trunk (yellow) |
Left gastric artery (dark green) |
Common hepatic artery (red) |
Phrenic artery (light green) |
Splenic artery (blue) |
Usually the celiac axis divides into three terminal vessels: the left gastric artery, the common hepatic artery, and the splenic artery (Figs. 11.6–11.7, Table 11.2).
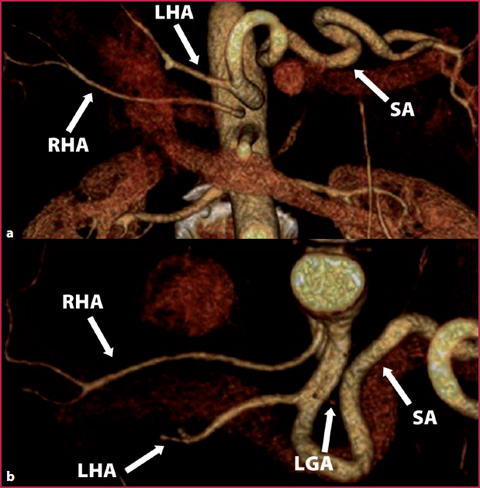
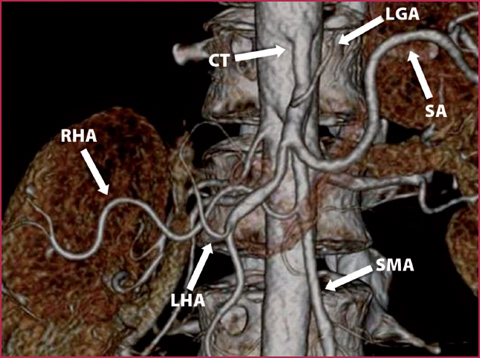
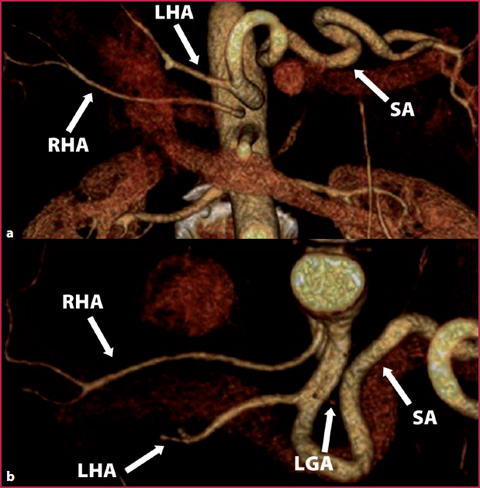
Fig. 11.6
CT angiography of the abdominal aorta and splanchnic vessels with 3D VR reconstruction. a Coronal plane. b Axial plane. The reconstruction shows the origin of left hepatic artery (LHA) from the celiac trunk, and the splenic artery (SA) and left gastric artery (LGA) originate normally. The right hepatic artery (RHA) originates independently from the abdominal aorta
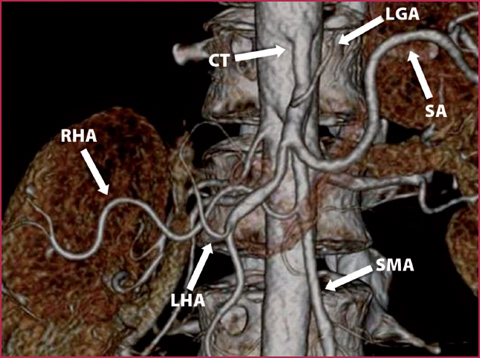
Fig. 11.7
CT angiography with 3D VR reconstruction on the coronal plane. The examination shows the origin of the left hepatic artery (LHA) from the celiac trunk (CT), and the splenic artery (SA) and left gastric artery (LGA) originate normally. The right hepatic artery (RHA) originates independently from the superior mesenteric artery (SMA)
Table 11.2
Normal anatomy and anatomic variants of the celiac trunk
Type I Complete celiac trunk | • Celiac trunk with normal trifurcation • Early origin of the left gastric artery with subsequent bifurcation in the common hepatic and splenic arteries • Origin of four branches from the celiac trunk: -Absence of the common hepatic artery with direct origin of the left and right hepatic arteries -Phrenic artery -Pancreatic-dorsal artery |
Type II Incomplete celiac trunk with the origin of remaining vessels directly from the abdominal aorta | • Gastro-splenic trunk • Hepato-gastric trunk • Tronco epatogastrico • Agenesis of the celiac trunk with independent origin of vessels from the abdominal aorta |
Type III Incomplete celiac trunk with the common origin of one or more branches from the superior mesenteric artery | • Celiac-mesenteric trunk • Hepato-mesenteric trunk • Spleno-mesenteric trunk • Spleno-hepato-mesenteric trunk |
The splenic artery lies behind the dorsal face of the pancreas and is usually divided into four segments: the suprapancreatic segment, immediately after the origin; the pancreatic segment, which lies on the dorsal face of the pancreas; the prepancreatic segment, located on the anterior face of the pancreas; and the prehilar segment, between the pancreas and the spleen.
The common hepatic artery branches off to the gastroduodenal artery, the right gastric artery and the supraduodenal artery, and therefore becomes a proper hepatic artery. The gastroduodenal artery divides into two branches: the superior pancreaticoduodenal artery and the right gastroeplipoic artery. The first case, the inferior pancreaticoduodenal artery, represents the pancreaticoduodenal arcade that creates a communication between the celiac axis and the superior mesenteric artery (Figs. 11.8–11.10).
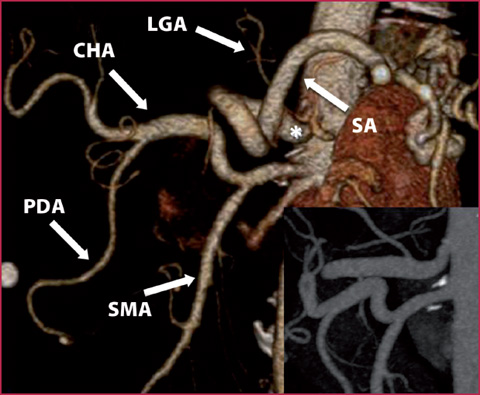
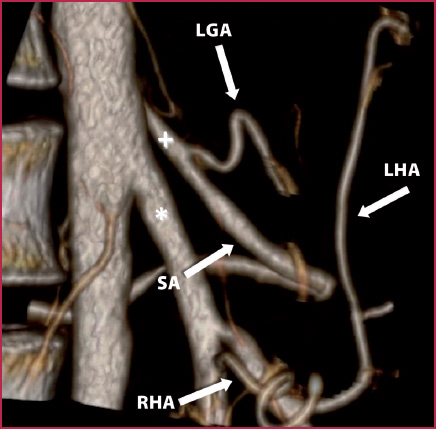
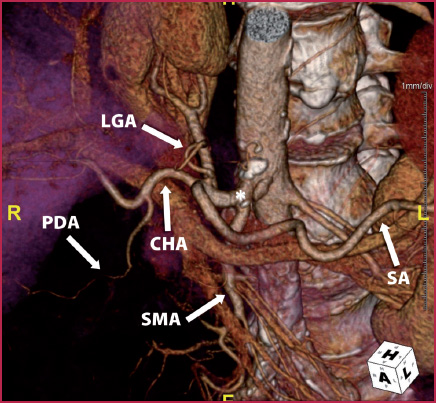
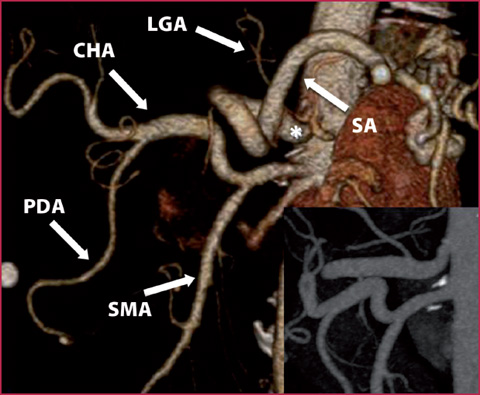
Fig. 11.8
The 3D VR reconstruction shows the common origin of the splenic artery (SA) and left gastric artery (LGA) from the gastro-splenic trunk (asterisk). The common hepatic artery (CHA) originates independently from the superior mesenteric artery (SMA); PDA, pancreatic-duodenal artery. The box at the bottom right represents a particular detail obtained with MIP reconstruction on the sagittal plane
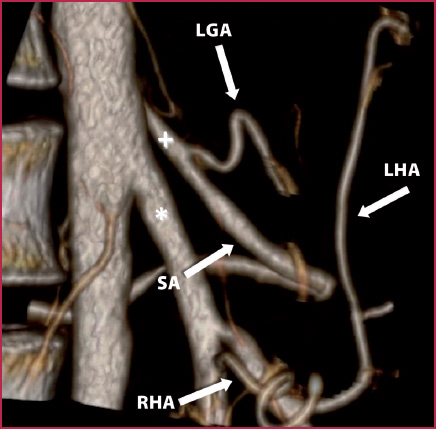
Fig. 11.9
3D reconstruction shows the common origin of the splenic artery (SA) and left gastric artery (LGA) from the gastro-splenic trunk (plus). The right (RHA) and left (LHA) hepatic arteries originate independently from the superior mesenteric artery (asterisk)
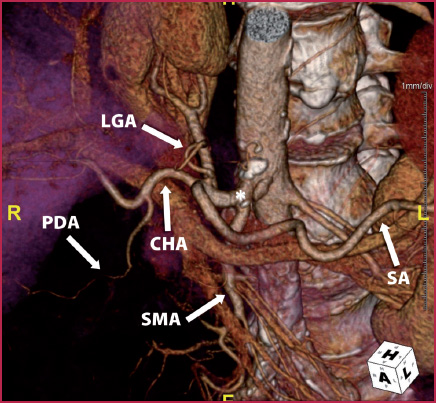
Fig. 11.10
3D VR reconstruction shows the common origin of the superior mesenteric artery (SMA) from the celiac trunk (asterisk); this anatomic variant is also called the celiac-mesenteric trunk. Downstream are the origins of the left gastric artery (LGA), splenic artery (SA) and common hepatic artery (CHA); PDA, pancreaticduodenal artery
Usually the hepatic artery per se divides into the right and left hepatic arteries. In any case, there are numerous anatomical variations; the most common are the replaced right hepatic artery, which arises from the superior mesenteric artery, and the replaced left hepatic artery, which arises from the left gastric artery. Less frequent variations include variations of number such as the accessory hepatic arteries both for the right or left hepatic segments.
Superior Mesenteric Artery
The superior mesenteric artery arises from the abdominal aorta caudally to the origin of the celiac axis, in the space between the twelfth thoracic vertebra and the second lumbar vertebra. Sometimes the superior mesenteric artery arises from the celiac axis and this variation is called the celiomesenteric trunk.
Collateral branches of the superior mesenteric artery are: the inferior pancreaticoduodenal artery, the ileocolic artery, the middle colic artery, the right colic artery and the jejunal and ileal branches (Fig. 11.11, Table 11.3).
Table 11.3
Superior mesenteric artery and its collateral branches
Superior mesenteric artery (red) |
Pancreatic-duodenal artery (green) |
Middle colic artery (purple) |
Right colic artery (light blue) |
Ileocolic artery (dark blue) |
Jejunal and ileal branches (yellow) |
The inferior pancreaticoduodenal artery is the first collateral branch of the superior mesenteric artery, originating from the left face of the vessels, with the superior pancreaticoduodenal artery representing the pancreaticoduodenal arcade.
The ileocolic artery supplies the terminal ileum, appendix, cecum and proximal part of the ascending colon. The ileal artery and colic artery arise from the ileocolic artery and create the ileocolic arcade.
The right colic artery may originate from the superior mesenteric artery, middle colic artery or ileocolic artery, and it is responsible for vascularization of the ascending colon and hepatic flexure. The middle colic artery is the second vessel that originates from right side of the superior mesenteric artery and it is responsible for vascularization of the transverse colon.
The left branch of the middle colic artery connects with the left colic artery, which originates from the inferior mesenteric artery, constituting the second most important collateral connection of the mesenteric arteries after the arc of Riolan (Fig. 11.12). Sometimes an accessory middle colic artery may be present that is called the middle mesenteric artery.


Fig. 11.12
CT angiography with 3D VR reconstruction showing the arc of Riolan that connects the superior and inferior mesenteric arteries
Inferior Mesenteric Artery
The inferior mesenteric artery arises from the anterior face of the abdominal aorta at the level of the third lumbar vertebra and branches off to the left colic artery, sigmoid arteries and the superior hemorrhoidal artery.
Branches of the left colic artery and sigmoid arteries form the marginal artery of Drummond, which also connects the ileocolic artery, right colic artery, middle colic artery, left colic artery, and superior sigmoid artery.
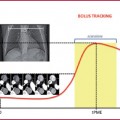
11.2 11.2 CTA Technique
Patient Preparation
Peripheral venous access (18-20G) in an antecubital vein;
Remove metal objects or clothing that could create artifacts;
Give to patients 500-800 mL of water to create negative contrast in the stomach and small bowel;
Patient in a supine position with arms behind head (to eliminate artifacts due to the skeletal segment of the upper arms). Otherwise the arms may be positioned on chest.
Image Acquisition
Acquisition parameters are shown in Table 11.4.
To obtain a good quality CTA image of the mesenteric vessels and renal arteries, thefollowing are mandatory:




Acquisition of topogram;
Place the region of interest (Rol);
Monitoring of intravascular attenuation with the bolus tracking technique and beginning of scan after a threshold of 150HU;
Acquisition of venous phase after 60-70 s after contrast medium administration (to study pathologies of the venous system).
High-iodine concentration contrast medium (>350 mg/mL), possibly pre-heated and administrated at a rapid injection rate (> 4 mL/s) (Table 11.5);
Short scan duration;
Thin layer reconstruction with minimum recon increment.
Table 11.4
Scanning parameters
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree