Fig. 9.1
An axial CT with bone window (a) and sagittal (b) and coronal (c) MPR with bone windows show a retained foreign body (a scep) into the right frontal squamous, confirmed by 3D reconstruction (d)
The major determinant of injury is the behavior of the penetrating object within the tissue which in turn depends on deformation, yaw (rotation about the long axis), and fragmentation of the projectile. The velocity of the penetrating object has been emphasized in previous studies and differentiates wounds into “low velocity” and “high velocity.” However, velocity is not an independent primary determinant of wounding potential [10].
The three most common types of low velocity penetrating head injuries are industrial accidents, suicide attempts, and results of criminal assault. Immediate radiological examination is mandatory because the small entrance wound does not correspond with the size of foreign body and associated intracranial injury. X-ray skull is useful to delineate the depth and direction of penetration.
In the civilian population, most gunshot wounds are the result of a semi-jacketed missile, which has an exposed, easily deformed, soft metal, or hollow-point tip. When deformation occurs, the diameter of the projectile may increase to two to three times its original size. The permanent cavity arises from the cutting action of the projectile and is comparable in size to the final diameter of the bullet. The increase in contact area also results in rapid deceleration of the missile and the release of energy into the surrounding tissues, producing a larger temporary cavity as well. Radial forces and subsequent pressure waves from the transfer of kinetic energy contribute to further tissue damage by the formation of this temporary cavity parallel to the bullet tract. The brain is extremely susceptible to the formation of both permanent and temporary cavitation [11]. The impact velocity of a missile and the incident angle influence whether the missile will penetrate the calvarium and the severity of fracture [11]. If the incident angle is small, a tangential wound may occur; that is, the missile penetrates the superficial soft tissues but does not enter the calvarium. In these wounds, the missile imparts a relatively small amount of its kinetic energy to the tissue, and the vast majority of the energy is retained by the projectile so that flight beyond the target is maintained. However, intracranial damage can occur owing to energy waves transmitted through the skull to the brain [12]. Skull fractures result when the tensile force caused by the missile exceeds the elastic properties of the skull.
Bone and bullet fragments deep within the brain parenchyma are potential sources of infection: insufficient heat is generated when firing a gun to sterilize a bullet. The necrotic tissue also provides an excellent culture medium for the growth of microorganisms, and the injured area is often lined by foreign material (hair, skin, and cloth) brought into the wound by the bullet [11]. For these reasons—secondary infection, brain edema, and hematomas can result in a fatal clinical course and death with medicolegal consequences [8]—one of the goals of the neurosurgeon is to remove all accessible bone, bullet fragments, and devitalized brain tissue [12].
In the emergency setting, when penetrating cranial injury is suspected, MDCT is considered the primary diagnostic examination [13, 14]. While MDCT easily detects metallic objects, wooden foreign bodies may be problematic in radiologic diagnosis [13]. Intracranial wood may show varying degrees of attenuation on CT scans. Dry wood, which often displays low attenuation, resembling air bubbles, should not be dismissed as air or an artifact. In subacute and chronic stages, a wooden foreign body absorbs water and approaches tissue density [13]. Although both CT and MRI imaging may be available for the detection of nonmetallic foreign bodies, such as wood and plastic, CT at various window widths should be considered the primary diagnostic technique, because MRI imaging may not differentiate dry wood from air or bone fragments [15].
In the emergency acute fashion, the CT patterns to reach on CT scan in emergency situation are:
the presence of retained foreign bodies for example gunshot, with its hole access or exit, if not retained
penumoencephalus
the correlated fractures and bone fragments migration
the parenchyma alterations correlated such as lacerocontusion, hemorrhagic intraparenchimal, or extraparenchimal collections (Epidural or Subdural hematoma, intraparenchimal satellite hematoma)
post-traumatic Subarachnoid Hemorrhage (SAH).
cerebral oedema
diffuse brain damage,
brainstem injury,
CNS infection, or ventricular injury.
Obviously, the more of these elements that are present, the worse the patient outcomes are. [16] (Figs. 9.2a–h, 9.3a–i).
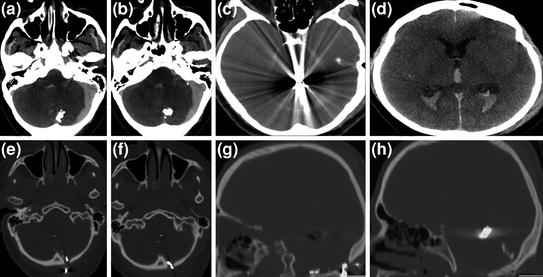
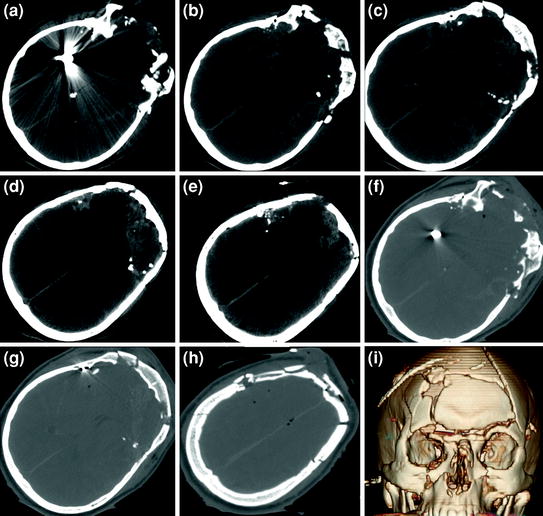
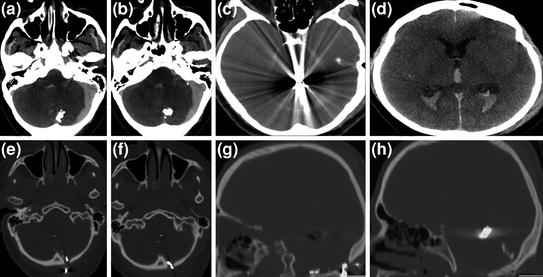
Fig. 9.2
The axial CT scan shows (a–d) multiple retained bullets in the posterior fossa with left subdural cerebellum haematoma and tetraventricular haematoma. The axial (e–f) and sagittal MPR (g–h) show the inlet hole at the occitial squamous and the retained bullets in the posterior fossa
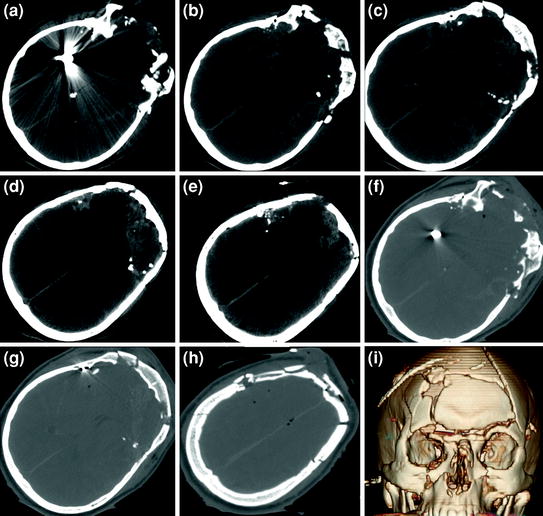
Fig. 9.3
The axial CT scan shows (a–e) retained bullets in the right temporal lobe with multiple fragments in the left frontal and temporal lobe. A traumatic diffuse SAH and a multiple hemorraghic left frontal contusions are present with small frontal penumoencefalus. The axial CT scan with bone window (f–h) shows the inlet hole a temporal squamous with retained bullet and multiple skull-bone fractures confirmed by 3D reconstruction (i)
During the follow-up, an infection element such as abscess, empyema, CSF injury, must be reached.
Brain swelling and CSF leak, orbit-cranial trajectory and intraventricular lodgement are associated with increased incidence of such complications.
Patients with retained intracranial missile fragments should be on regular follow-up so that such complications are recognized and treated as they occur [17, 18].
A good practice suggests that every patient with an open wound be inspected carefully—a claim that should be self-evident. If there is any risk of existing penetrating or depressed skull trauma, CT imaging should be performed, even in patients with a Glasgow Coma Scale sum score of 14 or 15 [19, 20].
Previous studies have demonstrated that in up to 14 % of patients with a Glasgow Coma Scale of 14, CT scans showed intracranial lesions. Additional CT angiography should be performed in penetrating injuries with hematomas or suspected vascular lesions [21].
It is recommended not to perform an MRI study if a retained foreign body is present, because of uncertain foreign body nature.
All the devices used during neurointerventional procedures such as cerebral aneurism embolization, vessel stenting, AVM embolization are compatible with MRI and it can be performed without any problem and without waiting time after the procedure. The presence of these devices is easy to reach and to identify and they produce an X-ray and MRI artifacts.
As endovascular procedure complication, a retained coils migration or a retained microcatheter fragment or small metallic splinter into SAH space are described and generally they are not correlated with any type of cerebral injury or infection [22] (Fig. 9.4a, b).
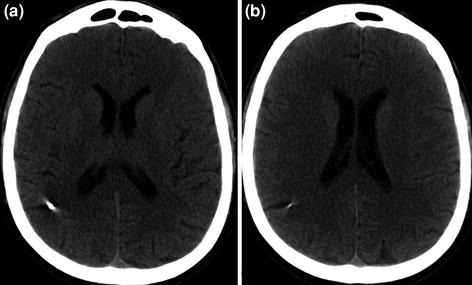
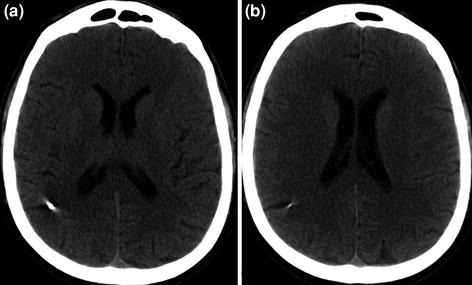
Fig. 9.4
a–b The axial CT scan shows a small retained metallic fragment in the right frontal subaracnoid space without any parenchima alteration, injected during a cerebral aneurysm embolization
In case of a retained microcatheter fragment is incorporated into the arterial wall of intracranial vessel while other portions may remain mobile and cause late peripheral arterial symptoms it should be surgically removed [23].
9.3 Retained Intraspinal Foreign Bodies
Penetrating injuries to the spine, although less common than blunt trauma from motor vehicle accidents, are important causes of injury to the spinal cord [24, 25]. They are essentially of two varieties—gunshot or stab wounds. Gunshot injuries to the spine are more commonly described and are associated with a higher incidence of neurological damage. On the contrary, the prognosis is better in stab wounds where surgery plays a greater role [26].
Approximately one-third of penetrating gunshot wounds causing spinal cord injuries are likely to involve a retained bullet fragment within the spinal canal [27




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree