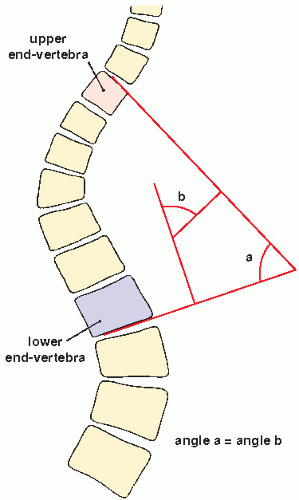
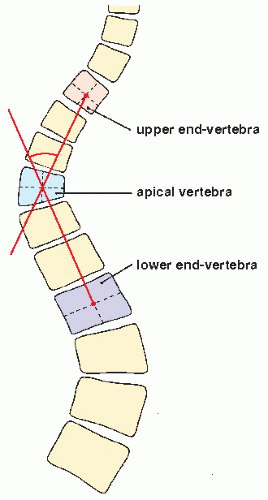
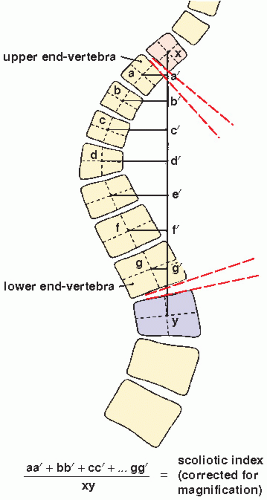
Lippman-Cobb method. The latter method, which has been adopted and standardized by the Scoliosis Research Society, classifies the severity of scoliotic curvature into seven groups (Table 33.2).
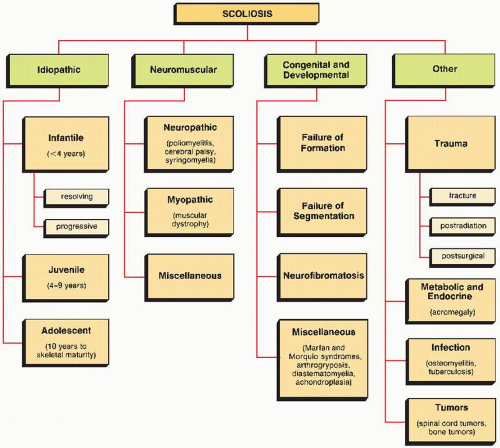
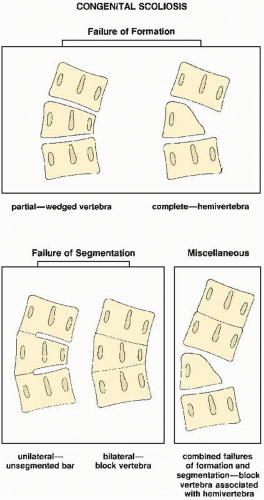 FIGURE 33.4 Classification of congenital scoliosis on the basis of cause. (Modified from MacEwen GD et al., 1968; Winter RB et al., 1968.) |
TABLE 33.1 Standard Radiographic Projections and Radiologic Techniques for Evaluating Scoliosis | ||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||
TABLE 33.2 Lippman-Cobb Classification of Scoliotic Curvature | ||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
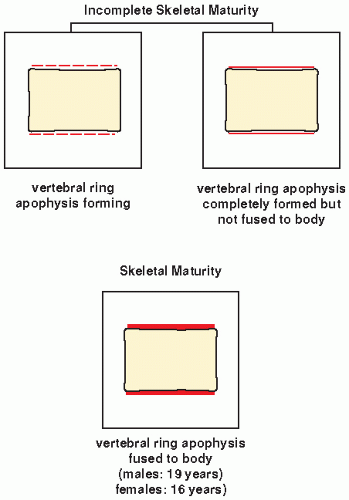 FIGURE 33.13 Skeletal maturity. Determination of skeletal maturity from ossification of the vertebral ring apophysis. |
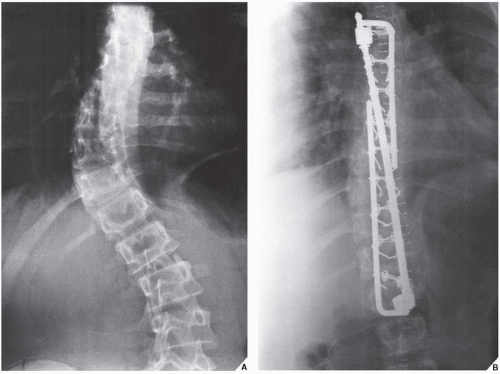
then fixed to the L-rods. Variations in this technique have been used with L-rod instrumentation alone, which involves the use of sublaminar wires fixed to the rods, or a combination of Harrington distractors and wires fixed to them. Cotrel-Dubousset spinal instrumentation using knurled rods has also gained popularity. Fixation is achieved via pediculotransverse double-hook purchase at several levels. The two knurled rods are additionally stabilized by two transverse traction devices. The Dwyer technique, involving anterior fixation of the spine and obliteration of the intervertebral disks, is also used in the surgical treatment of scoliosis but more often in the paralytic types of the deformity.
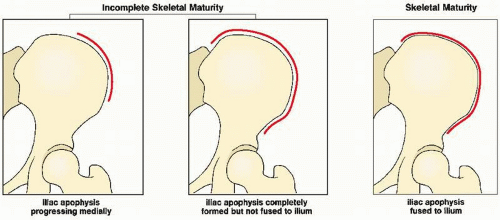 FIGURE 33.15 Skeletal maturity. Determination of skeletal maturity from the status of ossification of the iliac apophysis. |
birth or may appear over time, occur in more than 90% of patients. The latter lesions have a smooth border that has been likened to the coast of California; this distinguishes them from the café-au-lait spots seen in fibrous dysplasia, which have rugged “coast of Maine” borders. These spots increase in size and number as the person grows older. Axillary or inguinal freckles are rare at birth, but appear throughout childhood and adolescence. Plexiform neurofibromatosis is a diffuse involvement of the nerves, associated with elephantoid masses of soft tissue (elephantiasis neuromatosa) and localized or generalized enlargement of a part or all of a limb. Patients with these manifestations are particularly prone to malignant tumors (see Fig. 22.35).
TABLE 33.3 Most Effective Radiographic Projections and Radiologic Techniques for Evaluating Common Anomalies with General Affliction of the Skeleton | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
vertebral bodies; with the introduction of MRI, this modality became more prevalent in investigation of the aforementioned abnormalities.
birth, but these more often appear later in infancy. This condition is also associated with other manifestations, such as deformities of the extremities, blue sclerae, laxity of ligaments, and dental abnormalities.
Type I | This most common type of the disorder is a relatively mild form, with autosomal-dominant inheritance. Bone fragility is mild to moderate and osteoporosis is invariably present. Sclera are distinctly blue and hearing loss or impairment is a common feature. Stature is normal or near normal. Wormian bones are present. The two subtypes are distinguished by the presence of normal teeth (subtype IA) or dentinogenesis imperfecta (subtype IB). |
Type II | This is the fetal or perinatal lethal form of the disorder. This form demonstrates an autosomal-dominant inheritance with new mutation. The very severe nature of generalized osteoporosis, bone fragility, and severe intrauterine growth retardation results in death in the fetal or early perinatal period. Of those infants who survive, 80% to 90% die by 4 weeks of age. All patients in this group have radiologic features typical of OI. In addition, the sclera are blue and the face has a triangle shape caused by soft craniofacial bones and a beaked nose. The calvarium is large relative to the face, and the skull shows a marked lack of mineralization as well as wormian bones. Limbs are short, broad, and angulated. Three subtypes, A, B, and C, are marked by differences in the appearance of the ribs and the long bones. In subtype A, the long bones are broad and crumpled and the ribs are broad, with continuous beading. In subtype B, the long bones also are broad and crumpled, but the ribs show either discontinuous beading or no beading. Subtype C is characterized by thin fractured long bones and ribs that are thin and beaded. |
Type III | This is a severe progressive form and represents a rare autosomal-dominant inheritance with new mutations. Bone fragility and osteopenia are considerable, leading with age to multiple fractures and severe progressive deformity of the long bones and spine. Bone abnormalities are generally less severe than in type II and more severe than in types I or IV. Sclera are normal, although pale blue or gray at birth, but the color changes through infancy and early childhood until it is normal by adolescence or adulthood. The calvarium is large, thin, and poorly ossified; wormian bones are present. |
Type IV | This is also a rare type of OI and is inherited as an autosomal-dominant trait. Characteristically, osteoporosis, bone fragility, and deformity are present, but they are very mild. Sclera are usually normal. The incidence of hearing impairment is low and is even lower than in type I. |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree