Fig. 8.1
Sonographic anatomy of the normal skin (3D reconstruction dorsal forearm, transverse view)
Nail
This is an enthesis organ that makes up a complex with the interphalangeal joint and the distal insertion of the extensor tendon . The nail unit can be divided in the ungual and periungual regions. The ungual region is composed of a hypoechoic nail bed mainly made up of collagen that may turn to slightly hyperechoic in the proximal region where the matrix is located. Above the nail bed, there is a hyperechoic bilaminar structure that is called the nail plate which is composed of hard keratin and has two layers: the dorsal and ventral plates separated by a hypoechoic interplate space. This virtual space turns to hyperechoic on higher frequencies ( ≥ 20 MHz). Underlying the nail bed, there is a hyperechoic line that corresponds to the bony margin of the distal phalanx . The periungual region is mostly composed of skin without fatty lobules and is divided into the lateral and proximal nail folds. However, hypodermal fatty tissue is prominent in the pulp of the fingers or toes ([16–20]; Fig. 8.2) .
Fig. 8.2
Sonographic anatomy of the normal nail. a, b 3D reconstructions (a: gray scale and b: power Doppler; longitudinal views, index finger; color filter) show the parts of the nail unit (a) and the ungual vessels (b), in color)
Hair
Scalp hair can be divided into two parts: the deep part which is the hair follicle located in the dermis, and the superficial (visible) part that makes up the hair tract. The hair follicle appears on ultrasound as an oblique hypoechoic dermal band and the scalp hair tract mostly shows as a trilaminar hyperechoic structure and ≤ 20 % may show a bilaminar hyperechoic pattern. The vellus hair present in the rest of the body appears as a hyperechoic monolaminar structure. The hair follicles can show different depth according to the cycle of the hair, also called the “hair clock hair.” Thus, immature hair follicles (telogen phase) are located in the upper dermis and mature hair follicles (anagen phase) are located in the deep dermis close to the upper hypodermis. In between these phases, there is a catagen phase. Also, the orientation of the hair follicles may present some differences according to ethnic parameters. Hence, hair follicles tend to be more oblique in Caucasians, almost parallel in individuals with African ancestry and more vertical in persons with Asian ancestry. The blood flow of the scalp shows a centripetal pattern and mainly originates from branches of the temporal and occipital arteries. ([21–24]; Figs. 8.3 and 8.4).
Fig. 8.3
Sonographic anatomy of the normal hair follicles (arrows) of the scalp
Fig. 8.4
Sonographic anatomy of a normal trilaminar hair tract of the scalp
Technical Considerations
Ultrasound examinations start with the visual inspection of the lesion and the regulation of the lighting in the examination room in order to assess the presence of single or multiple lesions . A copious amount of gel is applied in the lesional and perilesional region. Comparisons with the contralateral side are also performed. The sonographic test begins with a gray scale sweep that is followed by a color or power Doppler sequence and then the distribution, thickness, type, and speed of the blood vessels is determined by spectral curve analysis. The ultrasound examinations should include at least two sweeps in perpendicular axes (transverse and longitudinal). Frequently, 3D reconstructions are performed in order to clearly demonstrate the pathology to the clinicians. In children ≤ 4 years old, sedation is commonly used in order to avoid movements or crying of the child that can produce artifacts on the screen . Normally, chloral hydrate or melatonin is administered 30 min before the ultrasound examination. The chloral hydrate dosage used is 50 mg/kg and the melatonin dosage varies according to age. Chloral hydrate allows deeper sedation than melatonin; therefore, melatonin is normally not used in periorificial lesions such as around the eyes or mouth because the child can easily wake up. In these last cases, the preferred sedative is chloral hydrate. The child is monitored using the modified Aldrete scoring and only discharged when the score is ≥ 9 points [9, 12, 13, 25–27] .
Pathologies
There are several dermatologic pathologies that can be scanned on ultrasound. However for academic purposes, we have divided the rheumatologic topics into the following parts :
Inflammatory Diseases
Psoriasis: Skin and Nail Involvement
This is an autoimmune disease that affects the skin, nails, enthesis, and joints . The role of ultrasound is to support an early diagnosis and to assess activity and monitoring of the disease [28, 29]. Cutaneous psoriatic plaques appear on ultrasound as thickening and/or undulation of the epidermis with decreased echogenicity and thickening of the upper dermis. Increased blood flow is usually detected in the dermal region of the plaque during active phases. Psoriatic onychopathy presents from early to late phases with thickening (i.e., increased distance between the ventral plate and the bony margin of the distance phalanx) and decreased echogenicity of the nail bed, loss of definition of the ventral plate, hyperechoic deposits in the ventral plate, loss of definition of both plates, wavy and thickened dorsal and ventral plates. Importantly, early changes in psoriatic onychopathy may be subclinical [20] . Commonly, hypervascularity can be detected in the proximal part of the nail bed during the active stages of the disease . Decreased or heterogeneous echogenicity of the tendons (due to enthesopathy), anechoic fluid or hypertrophic synovium in the joints as well as periarticular bony erosions can also be present ([29–35]; Figs. 8.5 and 8.6) .
Fig. 8.5
Cutaneous psoriasis plaque. a Power Doppler and b 3D reconstruction gray scale. Notice the thickening of the epidermis and the hypoechoic band in the upper dermis (*). Increased vascularity (a, in color) is also shown in the dermal part of the plaque (a)
Fig. 8.6
Common sonographic alterations in psoriatic onychopathy
Morphea
This is the cutaneous form of scleroderma, a connective tissue disease, and can show dermal, hypodermal, and fascial involvement . This latter fascial type is also called eosinophilic fasciitis. Morphea can go from inflammatory to atrophic stages and generate multiple plaque-type lesions; affect one or both sides of the body or produce a linear type of involvement which is frequently seen in children and can present as “en coup de sabre” (ECDS), progressive hemifacial atrophy (Parry–Romberg Syndrome, PRS), among other subtypes [34, 36–38]. The phases show different patterns on ultrasound which can be used for assessing the activity of the disease [38]. Usually during the inflammatory phase, there is thickening and decreased echogenicity of the dermis and increased echogenicity of the underlying hypodermis. In the atrophy phase, there is thinning of the dermis and hypodermis, sometimes with absence of fatty lobules, which can generate direct contact between the muscle and the dermis. In between these phases, there is an inactive phase. Frequently, in patients with multiple morphea plaques, there are asynchronic activity between different plaques or parts of the same plaque. This subclinical data could be critical for the early management of these cases [34, 38] .
Increased regional blood flow and hyperechogenicity of the hypodermis have been reported as the most sensitive sonographic signs for assessing activity in morphea. Also, inflammatory signs of the ipsilateral parotid gland (i.e., decreased echogenicity and/or hypervascularity) have been reported in concomitance with Parry–Romberg Syndrome [34, 38]. Upward displacement of the nail plate, increased thickness, and decreased echogenicity of the nail bed due to edema, have also been reported in scleroderma ([20]; Fig. 8.7) .
Fig. 8.7
Morphea. a Active phase (color Doppler; transverse view; right cheek) shows thickening and decreased echogenicity of the dermis (*) with increased echogenicity of the underlying hypodermis (o). A vessel is observed in the dermal part of the lesion (arrow). b Atrophy phase (gray scale; frontal region; transverse view) demonstrates lack of fatty tissue in the hypodermis (*, between markers) in the lesional area
Dermatomyositis
This is an autoimmune disease that affects skeletal muscle, skin, and lungs . On sonography, increased echogenicity of the muscle due to inflammation has been reported. Calcinosis cutis is a common finding in this condition which can be detected on ultrasound as hyperechoic dermal or hypodermal deposits that show a posterior acoustic artifact. These calcinosis deposits may also be seen in the periungual regions at the tip of the fingers. Increased echogenicity of the hypodermis due to panniculitis may also be seen ([20, 34]; Fig. 8.8) .
Fig. 8.8
Dermatomyositis, calcinosis. Ultrasound (gray scale, transverse view, right gluteal region) shows hyperechoic calcified deposits (*, between markers) in the hypodermis with posterior acoustic shadowing artifact
Cutaneous Lupus
This is the cutaneous manifestation of lupus erythematosus which may precede its systemic involvement . According to activity, cutaneous lupus has three phases: acute, subacute, and chronic, also called discoid lupus. On sonography, the acute phase shows as thickening and decreased echogenicity of the dermis with increased echogenicity of the underlying hypodermis and regional hypervascularity (Fig. 8.9) . Occasionally, the dermal involvement may take a fusiform shape. In the discoid or chonic lupus, there is atrophy and hypoechogenicity of the dermis with hypovascularity. Isolated increased echogenicity of the hypodermis in the acute phase can also be observed which is called “lupus panniculitis” or “lupus profundus.” Additionally, thrombosis and vasculitis may complicate the disease. The thrombosis appears as hypoechoic material within the vessels that show lack of blood flow. The disease may also affect the nail matrix and bed and cause inflammatory and/or atrophic changes in the ungual region with dystrophy (i.e., irregularities) of the nail plate [20, 34] .
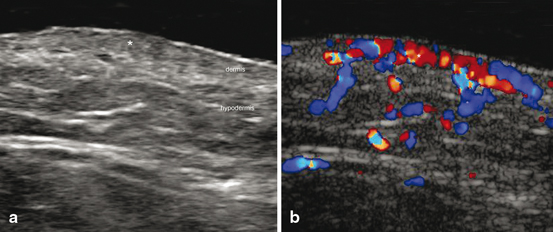
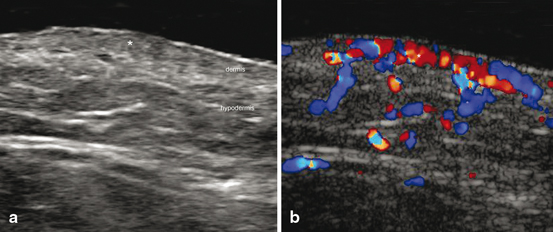
Fig. 8.9
Acute Lupus. a Ultrasound (gray scale, transverse view, right mandible region) demonstrates thickening and decreased echogenicity of the dermis in the lesional area (*). b Color Doppler ultrasound shows increased vascularity in the region (*)
Rheumatoid Arthritis
This is a systemic autoimmune inflammatory disease that affects the joints in concomitance with diverse organs which include the nails . Ultrasound may support the early assessment of anatomic changes within the joints such as synovitis, periarticular bony erosions, narrowing of the joint space, tendinopathy, tear or atrophy of the tendons, among other signs. In the nail unit, rheumatoid arthritis produces thickening and decreased echogenicity of the nail bed with regional hypervascularity during the active phases of the disease. Upward displacement of the ungual plaques can also be detected due to edema ([20]; Fig. 8.10). In contrast with psoriatic onychopathy, these patients do not show prominent involvement of the nail plate [35] .
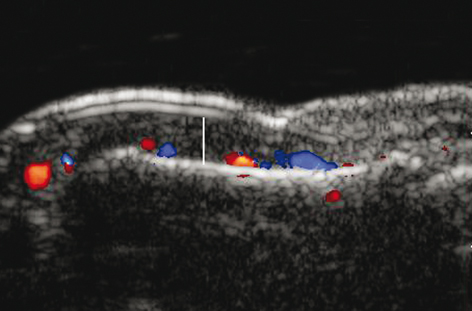
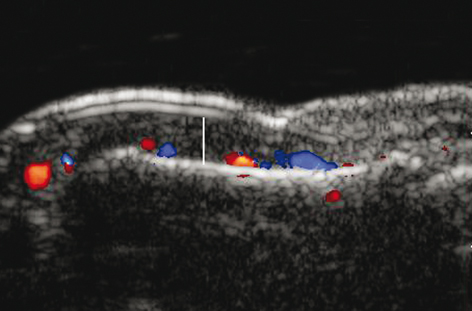
Fig. 8.10
Rheumatoid arthritis. Color Doppler ultrasound of the nail demonstrated upward displacement of the ungual plaques due to thickening of the nail bed (vertical white line)
Immunosuppression Complications
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree