Fig. 11.1
Plain film of the carpus (two projections, a and b) shows a metallic foreign body (arrow) located in the soft tissues
Cheap and easy availability of conventional radiography makes it the first line investigation in any setting. Limitations of radiography include nonvisualization of radiolucent FBs, radiation exposure, and failure of precise localization during removal.
Failure to remove FBs is likely to give rise to acute or late complications, such as allergies, inflammation, or infection, that may be severe.
Knowledge of the exact location of FB relative to skin surfaces, adjacent muscles, tendons, neurovascular bundles, and other vascular structures allows more controlled surgical dissection.
Soft Tissue Foreign Bodies
FBs retained in the soft tissues are a common reason for medical consultation, and usually consist of wooden or metal splinters or glass shards.
Self-inserted soft-tissue FBs, the deliberate and direct destruction or alteration of body tissue without suicidal intent, is a relatively recent focus of scrutiny by the medical community [4]. In the United States, 4 % of the general population and 13–23 % of adolescents report a history of nonsuicidal self-injury [5, 6]. These numbers are potentially underestimated as a result of underreporting due to the socially unacceptable nature of the act and the feelings of guilt experienced by the patient after the self-injury [5, 7].
Most metallic materials are opaque on radiographs. However, some referring physicians do not realize that thorns, splinters, wooden fragments, and pieces of plastic are usually not sufficiently opaque to be visualized [8–12]. On the other hand, glass of all types is radio-opaque [8, 9, 13]. The opacity of glass is not related to its lead content; therefore, all substantially large pieces of glass should be visible on radiographs.
Bullet wounds are far too common in the United States. Bullets (Fig. 11.2) are usually described by their caliber, which is a measurement of their diameter in inches or in millimeters. Although the caliber of a bullet is important, it has only a loose relationship to the weight of the bullet and the size of its charge. These latter parameters help determine the kinetic energy of the bullet, which is an important factor in determining its wounding potential. Bullets are usually composed of lead, and they may be fully or partially covered by an outer metal jacket (full metal jacket) that is usually composed of copper.


Fig. 11.2
Lateral radiograph of the neck shows the presence of a projectile lodged in the soft tissues posteriorly to the spinous process of C3–C4
Bullet injuries are most severe in friable solid organs (e.g., the liver and brain), where damage may be caused by temporary cavitation remote from the actual bullet track. Dense tissues (e.g., bone) and loose tissues (e.g., subcutaneous fat) are more resistant to bullet injury. Bones modify the behavior of bullets markedly, altering their course, slowing them down, and increasing their deformity and fragmentation [14].
Role of Imaging Procedures in the Detection of Soft Tissue Foreign Bodies
FBs can seldom be identified and removed on the basis of clinical examination alone, and usually only when superficially located at the level of the soft tissues. Otherwise, imaging techniques are required to recognize the FB and establish its exact location prior to surgical removal attempt. Conventional radiography is still now the first radiological procedure performed in patients with a clinical suspicion of soft tissue FB. Two projections are required in order to best determine the location of the FB (Fig. 11.3).


Fig. 11.3
Radiographs (two projections) of a 5-year-boy who stepped on a nail show the nail (a and b, arrow) in the soft tissue of his foot
Traditional radiography usually demonstrate radio-opaque FBs (Fig. 11.4); the radiological visualization of FBs depends on their radiopacity. Metal objects with a relatively high atomic weight are easily visible on plain films even if they are millimetric (Fig. 11.5). Almost all objects composed of plastic and most thin aluminum objects, such as pull tabs on cans, are not radio-opaque. Aluminum is of low radiodensity, which makes visualization on radiographs difficult [15]. The atomic numbers of soft tissue and aluminum (7.5 and 13, respectively) are similar [16].

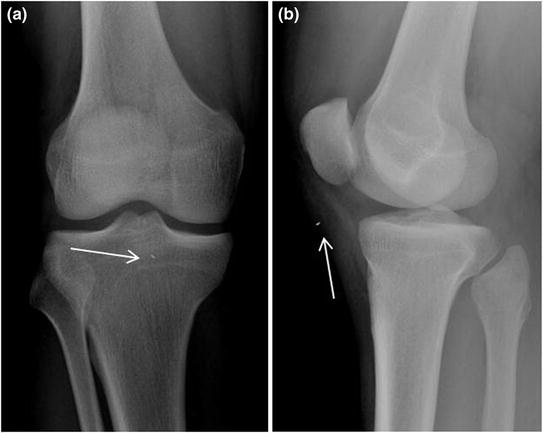

Fig. 11.4
Lateral radiograph of elbow shows the presence of a radio-opaque foreign body (needle, arrow) located in the soft tissues
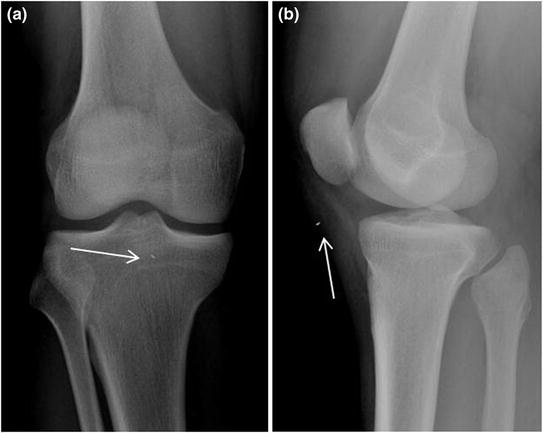
Fig. 11.5
Antero-posterior (a) and lateral (b) radiographs of the knee demonstrate the presence of a millimetric foreign body (arrow) located in the soft tissue region inferiorly to the rotula
Glass is always radio-opaque, and its radio-opacity does not depend on its content of lead or other metals. Glass FB, whether ingested, inserted into a body cavity, or deposited in the soft tissues of an extremity by an injury, should always be detectable on radiographs. This detectability obviously depends on the size of the object. Submillimeter pieces of glass buried deep in the soft tissue of an obese person may not be visible. However, any substantial piece of glass 1–2 mm or larger should generally be detected.
As traditional radiograms are widely available, simple to perform, and inexpensive, X-ray is the reference first diagnostic examination [17] and will identify radio-opaque FBs (glass, metal, stone) in around 80 % of cases, but only displays 15 % of nonradio-opaque FBs (wood, plastic) [18, 19]. Radioscopy offers a more accurate topographic assessment and allows reference points to be marked on the skin to aid subsequent FB removal. However, radioscopy exposes patient and operator alike to relatively high doses of ionizing radiation.
Ultrasonography has now proved irreplaceable, with high sensibility and specificity [17, 20–22]. Ultrasonography is the first choice investigation in the diagnosis of an FB retained in the soft tissues, as it has a sensitivity and specificity of 90 and 96 %, respectively [23, 24]. Due to its high spatial resolution, ultrasound will identify FBs smaller than a millimetre [25], be they wood, glass, metal, or plastic [26]. The limitations of ultrasound are well known; it is an operator-dependent technique and will only display FBs retained in superficial tissues [26].
Ultrasound examination will also establish the integrity of the surrounding ligaments, tendons, joint capsules, and neurovascular structures (with the aid of color Doppler) and accurately depict the relations between the FB and adjacent structures (tendons, nerves, vessels) to ensure the safe removal of the FB, avoiding iatrogenic lesions or complications [26].
Moreover, ultrasound-guided percutaneous removal of FBs is a safe and viable approach to the management of FBs achieving at least 88 % success overall [27].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree