Fig. 2.1
The vertebral column, AP (a) and LL projections (b). (b) Cervical and lumbar lordosis and dorsal and sacral kyphosis
In the foetus, we can observe a single concave curvature of the rachis, towards the front. After 4 months only, cervical lordosis appears, and the child learns to hold his or her head up; lumbar lordosis and sacrum tilt take place when the child starts trying to achieve the upright and walking position, that is, between 10 months and 2 years of age. The mechanic adjustment of the curvature derives from the need of increasing the resistance to higher loads, determined by the human bipedal position and movement. Bioengineering researches show that the physiological curves increase by ten times the column resistance to the vertical compression.
The first two cervical vertebrae, the atlas (C1) and the epistropheus (C2) are morphologically different for their head-support function and for their capacity of allowing the movements of rotation and bending. The atlas has a ring shape and its vertebral body is not completely formed. It consists of an anterior and a posterior arch, connected through a lateral mass. The superior articular facets are connected to the corresponding condyles of the occipital bone, at the cranial base, while the inferior facets articulate with the superior facets of the epistropheus. From the superior part of the epistropheus, the odontoid process develops, also referred to as the dens epistropheus. It forms a synovial joint with the posterior profile of the anterior arch of C1, it is supported by a resistant ligament structure, and it is the fulcrum of rotation for the atlas and the cranium. The occipito-cervical junction is a cardan system, with two perpendicular and fixed axes of rotation and an instantaneous axis obtained by the variable combination of the first two ones. In particular, in order to satisfy the needs of coordination of the ocular-cervical movements, we can distinguish a superior cardan system, in correspondence of the occipito-cervical junction, that enables limited but precise movements of the head and an articular cervical system that enables more ample, but less precise, movements for the flexion-extension and the rotation towards the sides. Such dynamics are connected to the visual function and justify the presence of the system of muscles involved in the movement of the cranio-vertebral junction, overlapping the system of muscles that enable the stabilisation of the cervical part of the rachis. The regular mechanical stress of the cervical spine justifies the frequent arthrosis involvement of this area.
Except for the first two cervical vertebrae, all the other vertebrae consist of a body, positioned in the anterior part, and of a posterior arch, characterised by the right and left pedicle connected to the pars interarticularis. Bone protuberances are located above and below each pars interarticularis, forming the superior and inferior articular processes, connected through a synovial joint to the relevant articular processes of the adjacent vertebral bodies. The intervertebral joints are subject to regular mechanical stress that causes the frequent morphological and structural alteration of the posterior arch, which may be deformed or even interrupted (isthmus), with the consequent possible ventral slip of the vertebral body (spondylolisthesis). The posterior arch consists of two posterior laminae merging in the spinous process that completes the ring, forming the spinal canal. Laterally, the posterior arches originate from the transverse processes that, along with the spinous processes, allow the insertion of several scheletric muscles (Fig. 2.2). In the cervical region, we do not find the synovial joints only but also another joint: the uncus or uncinate process, a lateral bone protuberance developing from the superior surface of the body of each cervical vertebra and articulating with a depression on the inferior profile of the superior vertebral body, forming the Luschka joint, considered the lateral extension of the intervertebral disc.
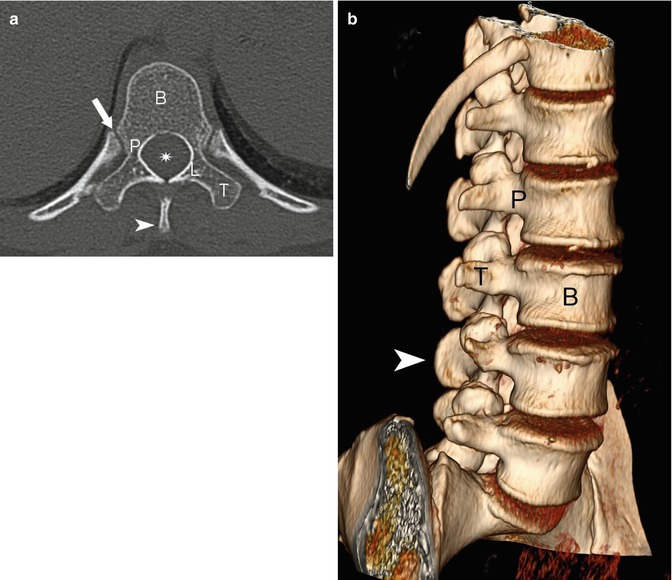
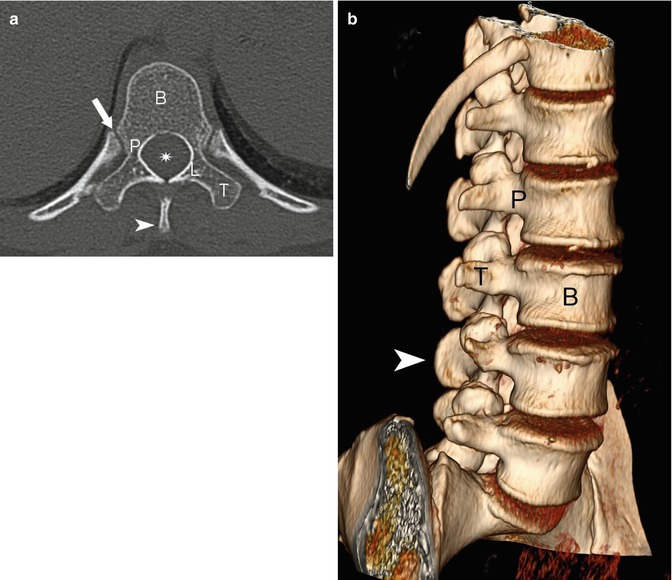
Fig. 2.2
(a) CT axial section of a dorsal vertebra. (b) Tridimensional CT, oblique projection of the lumbar rachis. Vertebral body (B), pedicles (P), laminae (L), transverse apophysis (T), spinous process (arrowhead), and costotransverse joint (arrow). The star shows the spinal canal
The vertebral bodies, going from the cranium to the pelvis, need to support heavier and heavier loads, and their diameters increase accordingly. Not only the diameters but also the shape of the vertebrae changes: the body of the cervical vertebrae is quadrangular, the thoracic vertebrae have an almost triangular body, while the lumbar vertebrae are bean-shaped. The axial CT and MRI scanning perfectly demonstrates the progressive cranio-caudal increase of the transversal section of each vertebral body, due to the need to support the increasing load and therefore the need to increase the resistance of the lumbar spine.
The space between the two vertebral bodies is occupied by the intervertebral disc, whose shape corresponds to the adjoining vertebral bodies.
Also the spinal canal changes its shape: it is triangular in the cervical and lumbar regions and round in the thoracic vertebrae. In the thoracic tract, the spinal canal has a smaller diameter, because the spinal cord is thinner in this region, while the diameter is bigger in the inferior cervical region and in the lumbar one, in correspondence of the so-called cervical and lumbar protuberances. Therefore, the transverse sections of the spinal cord and the spinal canal match. The spinal nerves exit through the neural foramina in each vertebral body. In the cervical spine, such foramina may be morphologically stretched and form a channel surrounded by the pedicles of the adjacent superior and inferior vertebrae: the anterior margin consists of the posterior part of the vertebral body and the uncinate process; the apophyseal masses and the interapophyseal joints form the posterior margin. The ventral and dorsal roots are located in the inferior part of the foramen, on the level of the disc, or underneath. Also in the lumbar region, the superior and inferior margins of the neural foramen are formed by the pedicles; at this level, the posterior profile of the above vertebral body and the posterior margin of the below disc form the anterior margin; the interapophyseal joint and a small part of the yellow ligament form the posterior margin. The lumbar nerve roots are localised in the superior part of the foramen, above the disc.
2.1.2 Intervertebral Discs
For the length and the peculiar shape of the spinal column, the intervertebral discs are essential elements, representing approximately 1/4 of the total length of this part of the skeleton. The height of the lumbar and thoracic discs diminishes from the bottom to the top. The discs are also involved in the formation of the normal curves of the spinal column: in the cervical and lumbar column, they are higher in the front than in the back; in the thoracic tract, they are instead shorter in the front than in the back, but not as much as the vertebral bodies. The intervertebral disc is composed of two parts, structurally well distinguished but strictly connected: the nucleus pulposus, a central gelatinous core composed of water, proteoglycans, and scattered collagen fibres, and an outer annulus fibrosus with collagen content (Fig. 2.3).
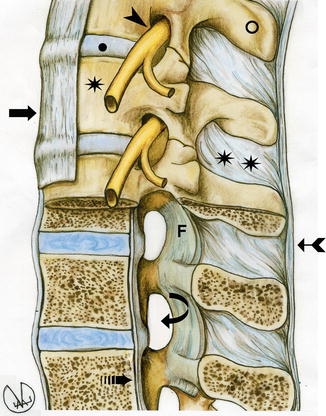
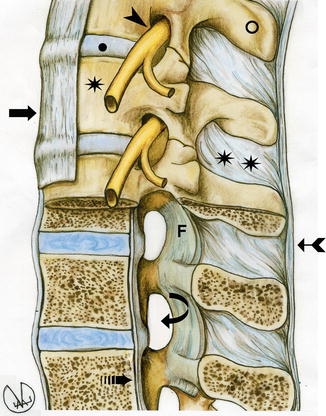
Fig. 2.3
Anatomy of the vertebral column, lateral view. Spinous apophysis (ring), intervertebral disc (circle), intervertebral foramen (curved arrow), interspinous ligament (double star), longitudinal anterior (arrow) and posterior (broken arrow) ligaments, supraspinous ligament (arched arrow), ligamentum flavum (F), nervous roots (arrowhead), and vertebral body (star)
The nucleus pulposus reacts to the load as a water cushion and distributes the pressure in a uniform way, in the transverse surface of the vertebral body, putting the fibrous ring under tension. In rest position, the nucleus is in the centre of the annulus or slightly oriented towards the dorsal region, such as in the thoracic and lumbar regions. When moving, it goes towards the side of the extension.
The discs, up to the second year of age, become avascular and their metabolism is exclusively governed by the phenomena of diffusion; in adult subjects, blood vessels appear in pathological conditions only. The superior and inferior disc facets perforate, without interruptions, the hyaline cartilage of the vertebral body end plates, where the collagen fibres of the annulus fibrosus are anchored. The relevant jointure formed between the vertebral bodies is termed a synchondrosis. The collagen fibres of the fibrous rings run in multiple directions, forming spirals due to the multiple forces. In particular, the vertical ones can minimise the compression and traction stresses; on the contrary, the oblique ones, towards the sides (from 30° to 45°) form a helicoidal system that minimises the stresses of rotation and pullout stresses. The mechanical resistance of the fibrous peripheral area of the disc is, in general, capable of resisting traumatic lesions, and therefore, in the event of a trauma, the vertebral body may fracture without dislocating or breaking the disc.
The intervertebral discs control the amplitude of the movements between vertebral bodies, while the articular processes affect the movement directions, limiting them, like rails. Protrusions of the cartilage of the intervertebral disc through the vertebral plate, and into the adjacent vertebra, may occur, forming discal hernias, because the plates may get weaker with advancing age, the so-called Schmorl’s nodes in Scheuermann’s disease (Fig. 2.4).
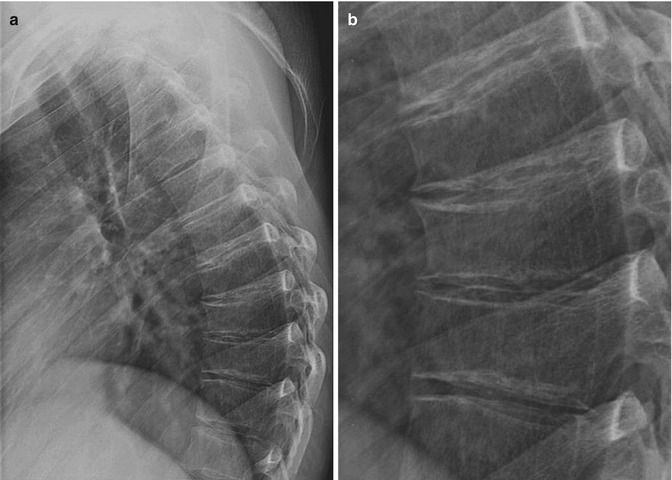

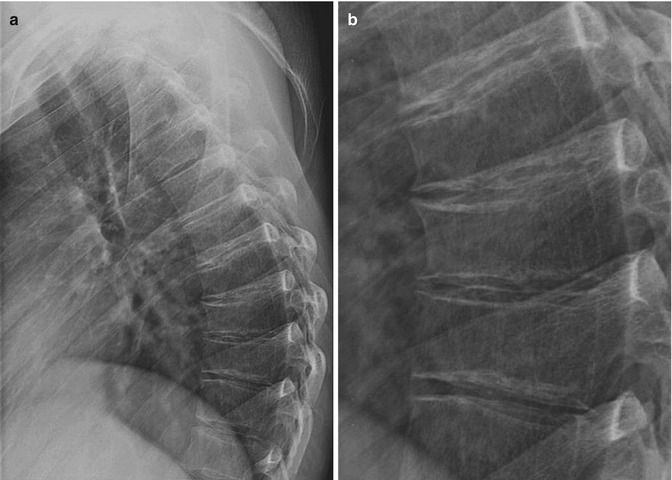

Fig. 2.4
X-ray, latero-lateral projection (a) and detailed view of the middle-inferior dorsal tract (b): anterior wedge-shaped deformation of the vertebral bodies and irregularity of the vertebral plates, more visible on the targeted projection, typical of Scheuermann’s diseases. (c) Sagittal T2-weighted image of the same patient, supporting the radiographic evidence and showing some Schmorl’s little nodules in the vertebral plates
During the day, in upright position, the intervertebral discs reduce their volume, and a minimal amount of fluid is in fact squeezed out by the pressure of the body; also the articular cartilages may flatten after prolonged pressure. In the evening, therefore, the overall stature of the body may be around 3 cm shorter than in the morning. As we get older, the stature variation during the day become less visible; in older people, the vertebral discs are less flexible due to their physiological progressive dehydration, and the stature reduction gets permanent. The alterations of the annulus fibrosus appear relatively earlier, between the 20th and the 40th year of age. When the nucleus pulposus is under pressure, it tends to move and put pressure on the fibrous ring, which is already weak; a protrusion, or hernia, may occur and push the content, generally the nerve roots, inside the spinal canal or the junction foramina. The intervertebral disc is innerved, especially on the anterior side, and this justifies the discal origin of specific back pain.
2.1.3 Ligaments
The vertebrate bodies and the intervertebral discs are connected to several ligament structures. The anterior longitudinal ligament goes from the base of the cranium to the sacrum and adheres to the anterior margin of the vertebral bodies and discs; the posterior longitudinal ligament goes from C2 to the sacrum, well adhering to the vertebral plates and to the posterior margin of the disc but separated from the middle posterior portion of the vertebral body by the interior-anterior epidural venous plexus and the basal vertebral veins. The superior extension of the posterior longitudinal ligament is the tectorial membrane that goes from C2 to the inferior part of the clivus.
In the elastic system of the vertebral disc bodies, tension is maintained through the ligaments, and such system is contrasted by the tension on the vertebral arches, maintained by the yellow ligaments.
The yellow ligaments (ligamenta flava) are flat; they connect the lamina of the vertebral hemiarch in cranio-caudal direction; the name is due to the yellowish colour of the prevailing elastic fibres that may extend considerably, without laceration, and that release the energy accumulated during the traction; such a capacity is reduced with advancing age. The ligamenta flava, which are longer and more robust in the lumbar region and thinner in the cervical region, work under strong tension and tend to stretch the spinal column; they oppose, along with the long dorsal muscles, to the anterior masses of the trunk that would otherwise bend the body forwards. The yellow ligaments have a static function also for their support to the posterior border of the neural foramina: in fact, their anterolateral border reaches the intervertebral joint and adheres to the anterior side of the capsule; in such a way, the vessels and nerves crossing the foramen lean on the smooth surface of the yellow ligament, rather than on the rough surface of the articular capsule.
The spinous processes are connected through the supraspinous and interspinous ligaments (Fig. 2.3).
In the cranio-vertebral junction, we find other ligaments whose function is to stabilise the atlantoaxial articulation and the cranio-cervical joint. The anterior atlantooccipital membrane connects the anterior margin of foramen magnum to the anterior arch of C1; the corresponding posterior atlantooccipital membrane runs from the posterior margin of the foramen magnum to the posterior arch of C1. Another important ligament is the cruciate ligament of atlas, consisting of the transverse ligament, strong horizontal component between lateral masses of C1, passing behind the dens and keeping it together with the anterior arch of C1, and the cranio-caudal component, fibrous band running from the transverse ligament and inserted superiorly (along with the tectorial membrane) in the caudal portion of the clivus. The apical ligament connects the apex of the dens to the anterior margin of the foramen magnum while the alar ligaments run laterally, from the dens to each occipital condyle (Fig. 2.5).
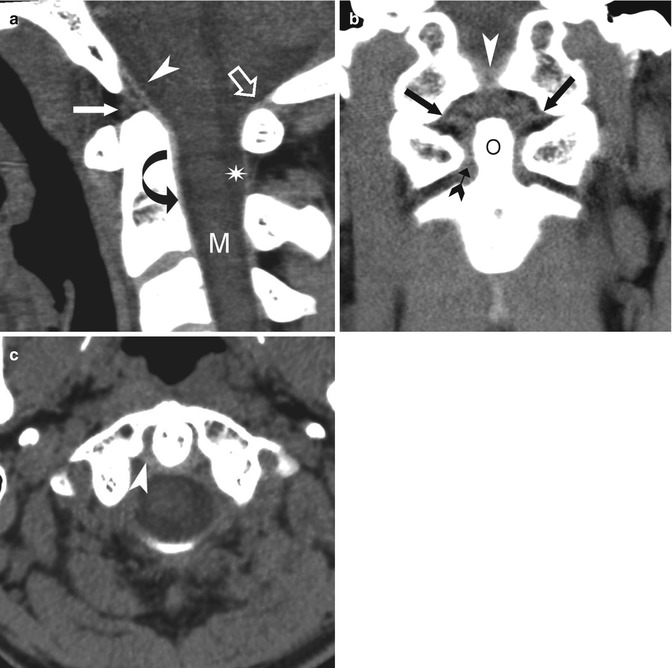
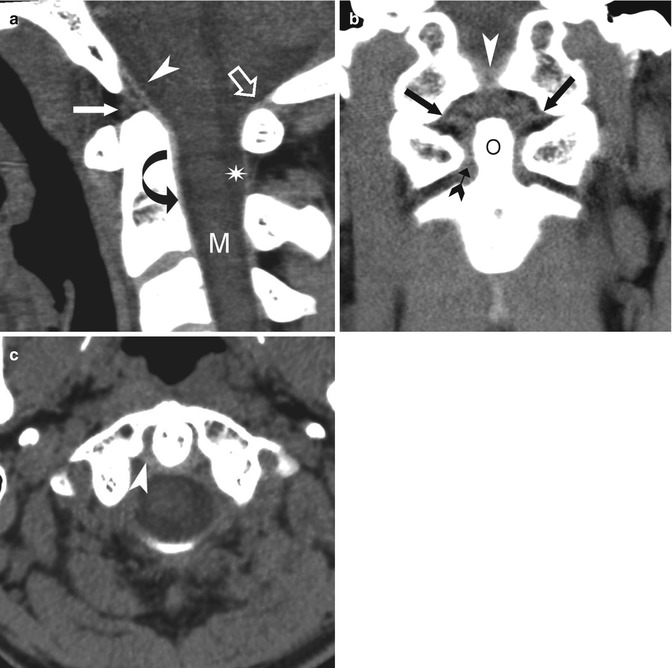
Fig. 2.5
CT sagittal (a), coronal (b), and axial (c) reconstruction, with algorithm for soft parts, showing the main ligaments of occipito-cervical junction. (a) The tectorial membrane (arrowhead), cranial part of the posterior longitudinal ligament (curved arrow), apical ligament (arrow), and atlantooccipital membrane (empty arrow). Cervical cord (M) contained in the hypointense cerebrospinal fluid of the subarachnoid space (star). (b) The alar ligament (arrows), transverse ligament (arched arrow), tectorial membrane (arrowhead), and odontoid process (O). (c) The transverse ligament (arrowhead), horizontal part of the cruciate ligament, inserting into the internal tubercles
2.1.4 Vertebral Canal
The cylindrical space, going from the occipital foramen to the sacrum, is the vertebral canal, and it is, therefore, the first “content” structure of the vertebral column; it has the form of a tube, structurally irregular for the alternation of rigid (vertebrae) and elastic (intervertebral discs) elements and for the presence of the lateral foramina (neural foramina) (Fig. 2.3). The vertebral canal, during the spine movements, is under mechanical stress; this is the reason why its anatomy is so complex; it is structured for the protection of the nerve structures contained therein.
The structure of the vertebral canal changes according to the kinematics of the rachis; in particular, the variations in flexion-extension determine sensible variations in the behaviour of the osteoligamentous walls: for example, during extension, the vertebral canal reduces from 5 to 9 cm, according to the different mobility, which is not equal in all the rachis tracts and that increases in the cervical and lumbar regions.
The transversal section dimensions of each vertebral canal tract vary on an individual basis and have been subject to several researches because of their clinical relevance. If the channel is too narrow, the adaptability of the spinal cord to the canal bone walls is limited. In vertebral canals smaller than the normal, any pathological issue, especially of degenerative-arthrosic nature, may determine a direct compression of the nerves (in particular, in the cervical-lumbar region) or involve the vascular systems and therefore indirectly affect the nerves.
The measurement of the diameters of the vertebral canal, previously based on the direct radiography or tomography, is currently carried out with computed tomography (CT) or magnetic resonance imaging (MRI). For such a purpose, it is important to remind that the pathological variations of the canal diameters can be almost exclusively performed with sagittal section and, in adults, diameters inferior to 11.5 mm should be considered abnormal. The transverse diameter is always wider than the sagittal one, in all regions of the spine; the maximum diameters are located in the cervical and lumbar regions.
2.1.5 Meninges
The spinal cord and its roots are enveloped by the meninges arriving from the cranial cavity. The adjacent dura and arachnoid mater (only virtually separated) surround the subarachnoid space, whose internal border is determined by the pia mater, strictly adherent to the spinal cord and the nerve roots (Fig. 2.6). In the fibrous dural sac, very resistant and closely adherent the anterior wall of the vertebral canal, the dura mater separates the cerebrospinal fluid—which freely circulates into the subarachnoid space (the space between the arachnoid and pia mater) and the ventricular system around and inside the brain and spinal cord—from the epidural space, where two components play an essential role: the adipose tissue, plugging the spaces between the dural sac and the vertebral bones’ borders, and the venous plexuses, draining the blood coming from the tissues of the vertebral spongiosa, functioning as an hydraulic cushion for the external stresses received by the nerve structures.
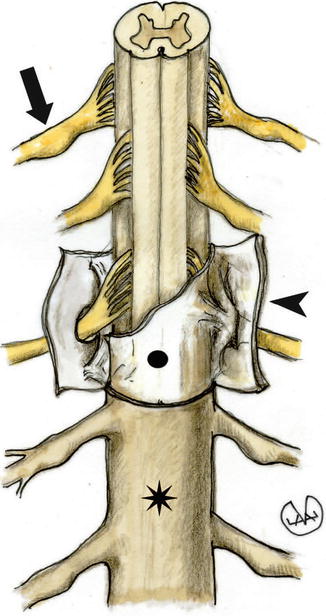
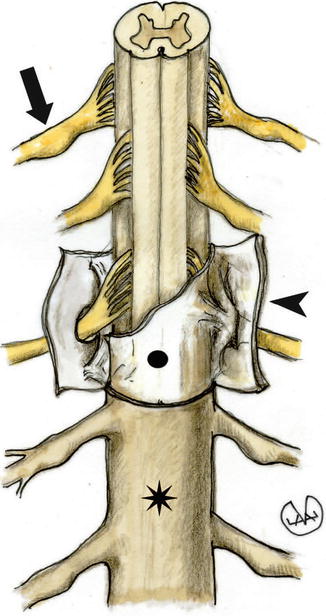
Fig. 2.6




Anatomy of the spinal cord. Dura mater (star), adherent to the arachnoid (circle). The arrow shows a spinal ganglion and the arrowhead shows the dura mater in section
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree