, Carlos Capuñay1, Carlos E. Sueldo2 and Juan Mariano Baronio3
(1)
Diagnóstico Maipú, Buenos Aires, Argentina
(2)
University of California, San Francisco, CA, USA
(3)
CEGYR, Buenos Aires, Argentina
The VHSG is a novel non invasive diagnostic modality which allows a complete evaluation of the gynecologic system (cervix, uterus and Fallopian tubes) in a single study [1–5]. It is performed with multislice computed tomography (MSCT) that obtains volumetric acquisitions in few seconds. Images can then be post-processed on diverse planes without loss of definition [6–8]. The MSCT achieves the concept of isotropy where, despite the acquisition of the image on the axial plane, it can evaluate the anatomy or the pathology in any other plane with similar image quality [9, 10] (Fig. 3.1).
Fig. 3.1
MSCT isotropic reconstruction. (a) The cube represents the acquired volume of the CT scan. The axial CT acquisition obtained with a thin slice thickness and 50 % image overlapping enables to reconstruct the CT data in any plane without loss of resolution. This is known as isotropy. (b) 3D volume rendering image. It exhibits the neck, uterine silhouette and Fallopian tubes. (c, d) Maximum intensity projection (MIP) images that show the gynecologic apparatus in its totality with this three-dimensional format. The MIP images identify very well the uterine tubes. (e, f) Virtual endoscopy images display endoluminal views of the isthmic and cervical region and the uterine fundus
VHSG needs multislice CT of 64 or more rows to acquire the images in less than 5 s. The objective of the study is to analyze all of the gynecologic system: cervix, uterus and Fallopian tubes. The structures most difficult to assess are the Fallopian tubes due to the fact that they are philliform and require optimum contrast distention during scanning to be evaluated. They opacify and empty very quickly, so it is essential that the scanning last the shortest time possible.
The VHSG study, provides useful information of the gynecologic apparatus and, simultaneously, evaluates intra-pelvic structures (Fig. 3.2).
Fig. 3.2
Associated findings. The VHSG study permits the evaluation of the intra-pelvic extra-gynecologic structures, offering complementary information. The findings can be of diverse etiology. (a) Osteolytic lesion in the left iliac bone (arrow). (b) Bilateral sacroiliac arthrosis (arrow). (c) Bone island on right acetabular roof (arrow). (d) Muscular atrophy in right pelvic region (arrow)
The way the study is performed is detailed in the present chapter. It consists in:
Preparation of the patient before the study.
Preparation of the patient during the study.
Technical parameters
Ways of reprocessing and analyzing the information.
Final report on findings and presentation of the study to the referring physician.
Complications.
Patient’s acceptance and discomfort to the VHSG study.
Preparation of the Patient Before the Study
A similar preparation to the conventional hysterosalpingography (HSG) procedure is required. A fact that stands out is that, being the VHSG a non invasive technique that does not require clamping the uterine cervix, a prophylactic treatment with antibiotics is not necessary.
The indications against carrying out the VHSG include pregnancy and active pelvic infection.
The study is performed between the 6th and 11th day of the menstrual cycle to avoid the interruption of any possible pregnancy. From the interruption of the menstrual bleeding until 48 h after the study, the patient must abstain from sexual intercourse.
Preparation of the Patient During the Study
The patient lies down on the CT table in the gynecologic position (Fig. 3.3).
Fig. 3.3
Patient’s position on the CT table to perform the VHSG study
The perineum is cleansed with Povidone-Iodine solution and sterilized gauze. Later, a speculum is placed at the vaginal level so as to have access the external cervical orifice which is also sanitized with sterilized gauze and Povidone-Iodine solution [4].
A digital explorer radiography is carried out (Scout View) previous to the study acquisition (Fig. 3.4). A plastic cannula of 10 F is placed in the external cervical orifice (Fig. 3.5) and approximately 15 ml of a mix of contrast and physiological solution of 70 % is instilled. The solution is applied with an injector pump at a speed of 0.3 ml/s (Fig. 3.6). The aim of doing it automatically is achieving a constant and smooth speed and pressure which reduces the discomfort during the procedure and assures an optimal uterine distention.

Fig. 3.4
(a) Scout view of the pelvis. (b) Scout view with the subsequent CT examination planned
Fig. 3.5
10F cannula utilized in the VHSG study

Fig. 3.6
Injector pump for automatic contrast administration
The acquisition initiates 30 s after beginning the contrast instillation.
As mentioned before, CT scanners of 64 or more rows that acquire images in less than 5 s are necessary to carry out the VHSG studies. CT scanners with lower number of detectors rows acquire studies in more prolonged times, of 10–12 s approximately, making the correct evaluation of the Fallopian tubes almost impossible in many cases.
The MSCT units of 256 or 320 detectors rows perform this technique in only 1.5 s, transforming this modality into a real time study because it can show the contrast passing from the ampullary region to the perineum [11–13] (Fig. 3.7), transforming this modality into a real time study.
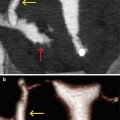
Fig. 3.7
256-slice VHSG study in real time. (a–d) Volume rendering images in different views that show a uterus of normal morphology. Bilateral tubal dilatation (yellow arrows) with contrast spillage into the peritoneal cavity (red arrows)
Technical Parameters to Use on the Units
The technical parameters used depend on the CT scanner used (Table 3.1).
Table 3.1
Technical parameters of VHSG according to CT scanner
Scanner | 64-slice | 256-slice |
Slice thickness (mm) | 0.9 | 0.625 |
Reconstruction interval (mm) | 0.45 | 0.3 |
kV | 80–100 | 80–100 |
mAs | 100–150 | 100–150 |
Scan time (s) | 3.2 | 1.5 |
Radiation dose (mSv) | 0.6 | 0.3 |
An automatic tube current modulation which reduces the radiation dose is used during the study. Furthermore, new scanners allow the so called iterative reconstruction that helps further diminish the radiation dose, without losing the image quality [14].
Once acquired, the images are transferred to a workstation where diverse types of reconstructions are carried out.
Ways of Reprocessing and Analyzing the Information
Various post-processing algorithms that consist of multiplane reconstructions, maximum intensity projection (MIP) reconstructions, volume rendering reconstructions and endoscopic views (EV) are used [15, 16].
Multiplanar Reconstructions
Coronary, sagittal and oblique reconstructions with soft tissue windows allow the evaluation of the cervix, uterus, Fallopian tubes and extra- uterine structures (Figs. 3.8 and 3.9).
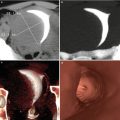
Fig. 3.8
Multiplanar reconstruction (MPR) images. Endometrial stalked polyp. (a) Magnified axial image of retroverted uterus which shows a stalked polyp. The head (yellow arrow) and the stalk (red arrow) of the polyp that extends to the cervix can be clearly observed. (b) Oblique MPR image. (c) Sagittal MPR image
Fig. 3.9




Multiplanar reconstruction (MPR) images of submucosal myoma with endocavitary projection (arrows). (a) Axial image that exhibits an elevated lesion which projects from the right lateral wall towards the uterine cavity compatible with submucosal myoma. (b) Coronal MPR image. (c) Sagittal MPR image
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree