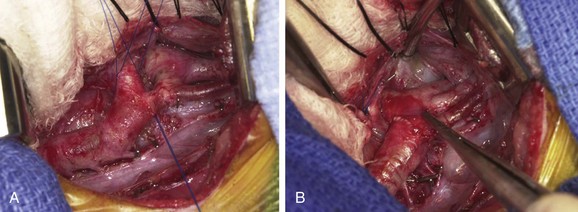
Chapter 70 Surgery for congenital heart disease is most commonly performed via a median sternotomy incision. Such an incision involves an anterior midline thoracic incision with dissection through the subcutaneous tissues down to the sternum. Once the sternum has been exposed, a sternal saw is used to split the sternum and a retractor is placed to define the operative field within which the pericardial sac is contained (Fig. 70-1). Because this incision offers excellent access to all of the structures contained within the mediastinum, including all chambers of the heart, ventricular outflow tracts, and venous returns, it is useful when multiple lesions are present or if a complicated repair must be performed. Figure 70-1 Median sternotomy. Less invasive options for repair of congenital heart lesions also exist, such as a partial median sternotomy or a thoracotomy. In the case of a partial median sternotomy, the skin incision is kept small and only the upper or lower sternum is divided (e-Fig. 70-2). Depending on the necessary exposure, thoracotomy incisions can be anterior, lateral, or posterior (e-Fig. 70-3). Historically, thoracotomy incisions involved the sectioning of a rib; in general these incisions now are made simply by dividing the intercostal muscles and leaving the ribs intact. e-Figure 70-2 Partial lower median sternotomy. e-Figure 70-3 Anterior right thoracotomy incisions for minimally invasive heart surgery. The type of lesion being repaired determines the choice of surgical incision. Straightforward repair of extracardiac lesions such as aortic coarctation, vascular rings, or PDA generally can be performed through a left thoracotomy (e-Fig. 70-4). In addition, in the case of simple intracardiac repairs such as an atrial septal defect (ASD), a minimally invasive approach can be used even though the operation requires the use of cardiopulmonary bypass (CPB). As techniques have been refined in recent years, interest has increased in operating on simple defects, as well as the mitral, tricuspid, and aortic valves, through minimally invasive incisions. In addition, interest has developed in performing relatively straightforward operations, including some heart valve surgery, using thoracoscopic or robotic techniques. In these cases, several very small incisions are made through which specially designed instruments can be placed and used to perform the procedure (e-Fig. 70-5). Advantages touted include an improved cosmetic result and potentially shorter recovery times inside and outside the hospital. e-Figure 70-4 Aortic coarctation. For most complex congenital heart defects, such as repair of an atrioventricular (AV) septal defect lesion, a median sternotomy is used. In this case the repair includes a right atriotomy, closure of a ventricular septal defect (VSD), repair of the ASD, and partitioning of the common AV valve into right and left components, with closure of the “cleft” in the left-sided AV valve (e-Fig. 70-6). Additionally, repair of cyanotic lesions typically requires the use of a median sternotomy incision. The reasoning is that these lesions often require greater exposure of both intracardiac and extracardiac structures that need to be repaired. One example of the need for a median sternotomy incision is a repair in a patient with TOF where an approach through the right atrium and the pulmonary artery is needed to close the VSD and relieve the right ventricular outflow obstruction. In some cases in which a very small pulmonary annulus or significant infundibular stenosis is present, the incision might even need to be extended to the right ventricular cavity (e-Fig. 70-7). e-Figure 70-6 Repaired complete atrioventricular septal defect seen through a right atriotomy. e-Figure 70-7 An intraoperative photograph of an infant with tetralogy of Fallot (TOF) demonstrates a typical setup for cardiopulmonary bypass. The choice of surgical approach also is important in the case of staged operations. A patient with HLHS generally will undergo three operations for complete palliation, and the need for a repeat sternotomy carries both operative and radiographic implications. Radiographically, imaging of the chest can help with operative planning because repeating median sternotomy incisions carries a greater risk of damage to the thoracic contents as a result of the formation of postoperative adhesions. For example, the aorta or other structures can be found very close to the sternum (e-Fig. 70-8) and might be damaged upon entry to the chest during the sternotomy, requiring the emergent institution of CPB. Careful review of chest imaging and the potential use of alternative, peripheral cannulation (discussed later) can help make the redo operation safer. Lesions that commonly require multiple operations include HLHS, TOF, and truncus arteriosus. e-Figure 70-8 Axial computed tomography images of a patient with previously repaired tetralogy of Fallot. Other scenarios influencing operative planning and the choice of incision include the presence of multiple lesions or when a complete repair is not indicated and a palliative procedure is indicated instead. Many congenital heart defects can occur together, such as coarctation of the aorta and VSD. In this case, a surgical procedure that might have been accomplished through a thoracotomy incision for isolated coarctation (e-Fig. 70-9
Surgical Considerations for Congenital Heart Disease
Surgical Approaches
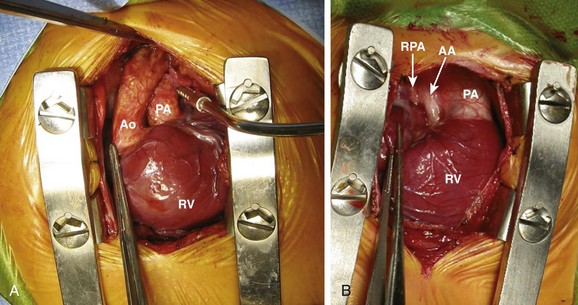
A, A sternal retractor is in place in a patient with transposition of the great arteries. The pericardium has been opened and sutured to the margins of the incision to expose the heart. The aorta (Ao) arises from the right ventricle (RV) and the pulmonary artery (PA) from the left ventricle. The left coronary artery and some of its branches also are seen. Note that the left ventricle, which is a posterior structure, is not well exposed. B, Similar exposure in a patient with hypoplastic left heart syndrome. The main PA is large and the ascending aorta (AA) is diminutive. The right pulmonary artery (RPA) is visible emerging from behind the aorta. The right atrial appendage is being grasped with a forceps. The right ventricle (RV) is also exposed. The cut pericardial edge, which is sutured to the skin edge, is more easily seen in this picture.
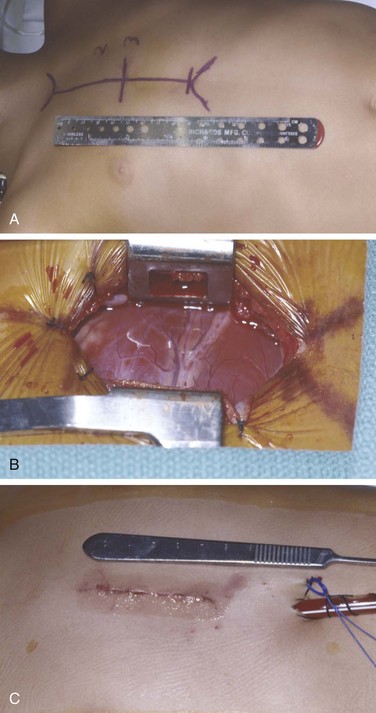
A, With the patient supine and the head to the left of the picture, the skin is marked preoperatively to show the length of the entire sternum, the second and third intercostal spaces (2 and 3), and the planned incision between the horizontal lines. In small children, a skin incision approximately 4 cm long can be used. B, The exposure created with this incision is shown. Compared with Figure 70-1, less of the pericardial contents are immediately obvious. C, The closed incision following repair of an atrial septal defect. A chest tube and pacing wires are seen exiting the skin caudal to the incision.
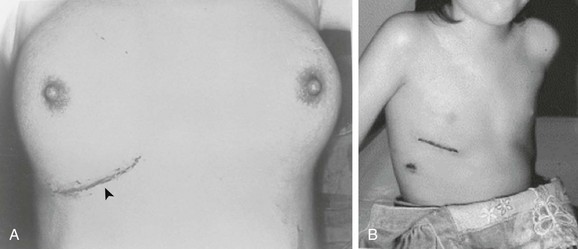
The incisions are generally made in the inframammary crease. These incisions sometimes are preferred, particularly for female patients.
A, Aortic arch, ductus arteriosus (vessel with two sutures encircling it), and aortic coarctation (vessel with single stay suture). Narrowing of the aortic isthmus occurs just proximal to the insertion of the ductus. B, The coarctation repair is complete. The ductus arteriosus has been ligated and divided, the coarctation has been excised, and the proximal and distal segments of the aorta have been connected with an extended end to end anastomosis. (Copyright 2010 CTSNet, Inc. All rights reserved. Image (http://www.ctsnet.org/sections/clinicalresources/congenital/expert_tech-.htm) is reproduced by permission of CTSNet, Inc.)
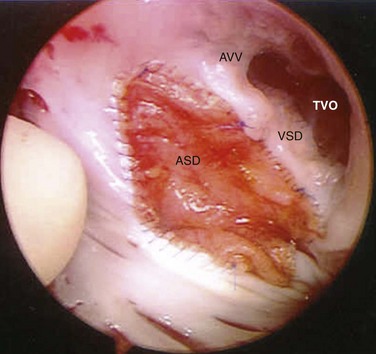
The pericardial atrial septal defect patch (ASD) and prosthetic inlet ventricular septal defect patch (VSD) can be seen. The patches are connected at the level of the atrioventricular valves (AVV). The right-sided (“tricuspid”) component of the AVV is labeled, as is the “tricuspid” valve orifice (TVO).
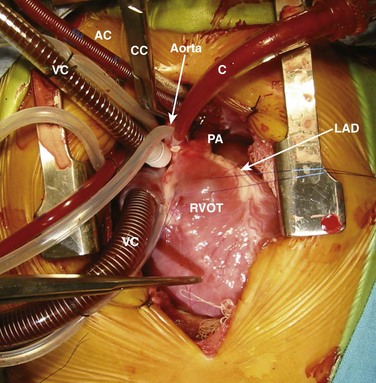
The patient’s head is toward the top of the picture. A cross-clamp (CC) has been applied to the aorta between the arterial cannula (AC) and the cardioplegia catheter (C). Venous cannulae (VC) are positioned in the superior vena cava and right atrium. The surface of the right ventricle is visible, and sutures are present in the right ventricular infundibulum (RVOT). The diminutive main pulmonary artery (PA), which is typical of patients with TOF, is seen. The left anterior descending coronary artery (LAD) is seen at the left lateral margin of the field. The left ventricle typically is not visible without retraction through a median sternotomy because it is a posterior structure.
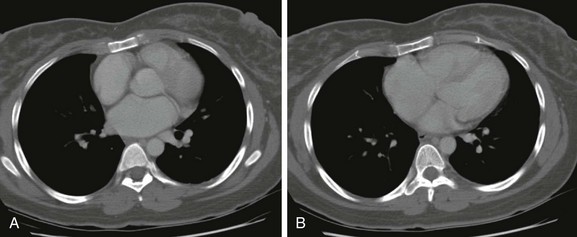
A, The right atrium and right ventricular outflow tract are in close proximity to the anterior chest wall. B, A more caudal image showing close proximity of the right atrium and ventricle to the anterior chest wall.
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Radiology Key
Fastest Radiology Insight Engine






