Category (mammography and MRI)
Assessment
Probability of malignancy, description
Clinical management recommendation
BI-RADS 0
Incomplete diagnostic information
Category that is primarily assigned in screening situations
Needs additional diagnostic evaluation
BI-RADS 1
Negative
0 % probability of malignancy
Needs no diagnostic workup; normal interval follow-up
BI-RADS 2
Definitely benign
0 % probability of malignancy, e.g., cyst, fatty tissue necrosis, hamartoma (fibroadenolipoma), juvenile fibroadenoma
Needs no diagnostic workup; normal interval follow-up
BI-RADS 3
Probably benign
<2 % probability of malignancy, e.g., adult fibroadenoma
Short-interval follow-up (6 months)
BI-RADS 4
Suspicious abnormality
Lesion with a few features not typical of malignancy; probability of malignancy of 30 % (range, 2–90 %); subcategories:
Short-interval follow-up; biopsy should be considered
4a: low suspicion (1–3 %)
4b: moderate suspicion (4–50 %)
4c: high suspicion (51–94 %)
BI-RADS 5
Highly suggestive of malignancy
Typical imaging features of malignancy, e.g., irregular margin, spiculation, inhomogeneous appearance; >90 % probability of malignancy
Short-interval follow-up and initiation of appropriate treatment
BI-RADS 6
Histologically proven malignancy
Breast cancer confirmed by histology
Additional diagnostic workup before initiation of appropriate treatment
Outside the screening context, breast lesions categorized as BI-RADS 0 are very rarely encountered because breast MRI is typically performed after conventional mammography and ultrasound (Mendelson et al. 2003).
Criteria used to assess breast lesions on contrast-enhanced MR images include the shape and demarcation of enhancing lesions, the pattern of enhancement, and the time course of enhancement. Malignancy is suggested by an irregular, star-shaped appearance with ring enhancement or rapid initial enhancement with postinitial washout, while a sharply marginated, round, or oval lesion with slow and continuous contrast medium uptake tends to be benign (Fischer 2012; Macura et al. 2006) (Table 11.2).
Table 11.2
Malignancy criteria of breast lesions on MRI
Criterion | Features suggesting malignancy | Nonspecific features |
|---|---|---|
Lesion shape | Dendritic, star shaped | Round, oval |
Lesion margin | Irregular margin, spiculated | Smooth margin |
Enhancement pattern | Ring enhancement | Inhomogeneous |
Enhancement kinetics | Strong initial signal increase; postinitial washout | Moderate initial signal increase; continuous postinitial signal increase, plateau phase |
Water content on T2-weighted images | Low water content | High water content, septa |
The so-called Goettingen score has been developed and used as a standardized tool for the comprehensive multifactorial evaluation of breast abnormalities on MRI and is most useful for the characterization of hypervascularized mass lesions. The tool integrates a maximum of criteria that have shown promise in differentiating between malignant and benign breast lesions. The strongest malignancy criteria – ring enhancement, strong initial enhancement (>100 %), and postinitial washout – are each assigned a score of 2. Less suspicious features are assigned a score of 1 and include irregular shape, ill-defined margins, inhomogeneous enhancement, 50–100 % initial contrast enhancement, and postinitial plateau. A score of 0 is assigned to features suggesting a benign lesion; these include round or oval shape, sharp margin, homogeneous enhancement, moderate initial signal increase of <50 %, and continuous postinitial signal increase. A lesion can thus be assigned a total score of 0–8 points. Breast lesions with a total Goettingen score of 1 or 2 (corresponding to ACR BI-RADS categories 1 and 2) are more likely benign, while lesions assigned a score of 4 or higher (corresponding to ACR BI-RADS categories 4 and 5) are more suspicious for malignancy (Fischer 2012).
Additional information for characterizing a breast lesion is provided by postprocessing tools that analyze contrast enhancement kinetics over time. This is done in a region of interest (ROI) placed in an area of contrast enhancement. In case of inhomogeneous lesion enhancement, the ROI is placed in the area showing the strongest enhancement. The ROI should include at least three pixels because misinterpretation of the enhancement pattern may result when the ROI is too small.
The signal increase after contrast medium administration can be expressed as a percentage relative to the baseline value on precontrast images or as a normalized value relative to the signal intensity of surrounding fat.
Strong initial enhancement with rapid washout is characteristic of a malignant breast lesion, while moderate initial enhancement with a slight further increase or plateau phase thereafter favors a benign lesion (Table 11.2).
Pitfalls in image interpretation arise from focal areas of enhancement within the glandular tissue in young premenopausal women (Amarosa et al. 2013) and in postmenopausal women on hormone replacement therapy (Pfleiderer et al. 2004). These foci may show the same rapid and strong initial enhancement as breast cancer. However, these foci are usually temporary and will no longer be detectable in a repeat examination (Kuhl et al. 1995; Liberman et al. 2002).
More recent studies suggest that fat-saturated diffusion-weighted SE images with generation of apparent diffusion coefficient (ADC) maps can help in characterizing breast lesions with inconclusive morphologic MRI features and dynamic kinetic patterns (Rahbar et al. 2011 ; Tsushima et al. 2009). High signal intensity of a suspicious lesion on diffusion-weighted images with low values in ADC maps suggests reduced perfusion and hypercellularity. Benign lesions or tumors that have responded to treatment usually have normal diffusion (De Bazelaire et al. 2010).
The following sections discuss the most important and most common incidental breast findings detected by MR mammography in the setting of whole-body MRI screening.
11.2 Benign Breast Lesions
11.2.1 Simple Breast Cysts
Breast cysts are round or oval fluid-filled structures that are highly variable in size (from microscopic to 5–6 cm). A larger cyst can often be palpated as a firm, elastic mass. Some breast cysts present with nipple discharge (Hines et al. 2010). Histologically, the fluid collection is surrounded by a double-layered wall – an inner epithelial and outer myoepithelial layer. Occasional thin septa may be present. Simple breast cysts are single or multiple (Fischer 2000) (Fig. 11.1 and Table 11.3). Cysts are a typical feature of fibrocystic breast changes. There is no risk of malignant transformation. Cysts are best detected by a meticulous ultrasound examination of the breast (Bhate et al. 2007; Mendelson et al. 2003).
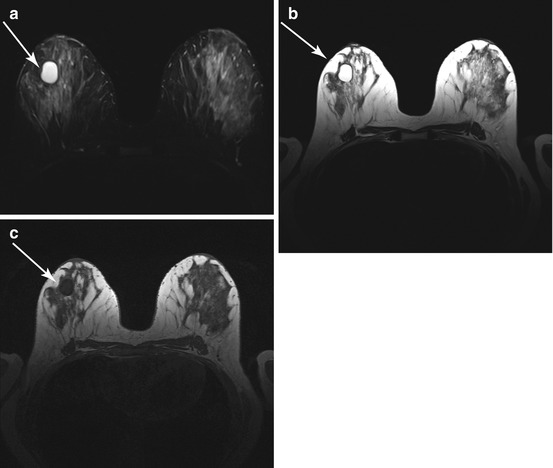
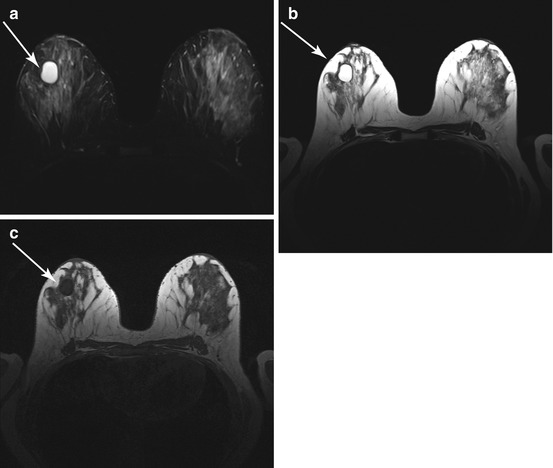
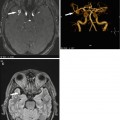
Fig. 11.1
Simple breast cyst (arrow) in a 48-year-old subject. (a) The cyst is depicted as a bright, sharply demarcated lesion on T2w TIRM image. (b) The cyst also has very high signal intensity on T2w TSE image. (c) Signal intensity is low on T1w image
Table 11.3
Simple breast cysts
Frequency | 10 % of all women |
Age predilection | Perimenopausal, typically between 30 and 50 years |
Type of lesion | Benign |
Signs and symptoms | Small breast cysts usually cause no symptoms; a large cyst is often palpable as a firm, elastic, freely movable mass |
MRI Features
T2-weighted images:
Very bright, fluid-filled, round or oval mass.
High protein content results in lower signal intensity.
Thin septa may be present within the cyst.
Non-contrast-enhanced T1-weighted images:
Dark, fluid-filled, round or oval mass
Contrast-enhanced T1-weighted images:
A simple breast cyst shows virtually no enhancement.
Cystic lesions become more conspicuous due to enhancement of surrounding glandular tissue.
Cyst content does not enhance (Uematsu and Kasami 2009b).
Differential Diagnosis
Complex breast cyst (see next section; intralesional hemorrhage or higher protein content results in higher T1 and lower T2 signal intensity)
Postoperative seroma (also high T2 and low T1 signal intensity; however, seroma is usually very large and sometimes painful; may appear heterogeneous and irregular and is typically located near the chest wall; and develops in the early postoperative phase) (Whipp and Halliwell 2008)
Other circumscribed lesions (intramammary lymph node, abscess, metastasis, fatty tissue necrosis, papilloma)
11.2.2 Complex Breast Cysts
Complex or complicated breast cysts (Table 11.4) differ from simple cysts in that they have debris within the fluid-filled sac or in that the wall or fluid may show signs of inflammation, hemorrhage, or neoplasm (Bhate et al. 2007; Hines et al. 2010) (Fig. 11.2).
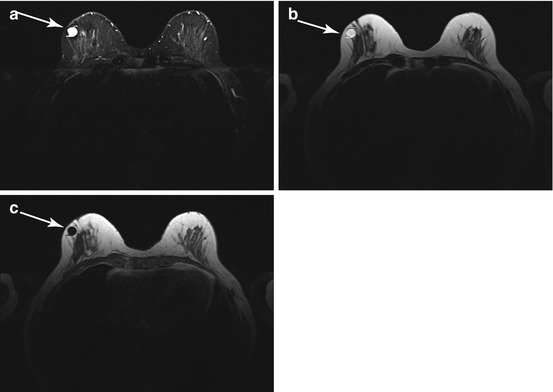
Table 11.4
Complex breast cysts
Frequency | 10 % of all women |
Age predilection | Perimenopausal, typically between 30 and 50 years |
Type of lesion | Benign; neoplastic changes in rare cases (0.2 %) |
Signs and symptoms | Small breast cysts usually cause no symptoms; a large cyst is often palpable as a firm, elastic, freely movable mass |
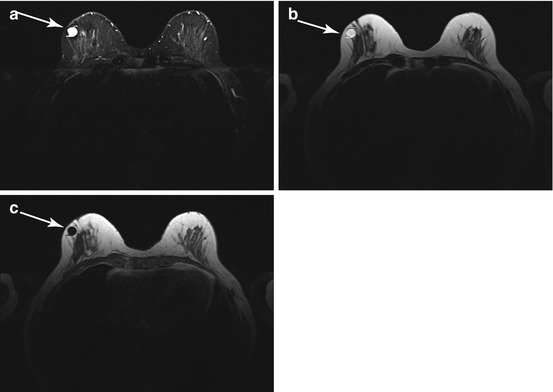
Fig. 11.2
Complex breast cyst (arrow) in a 66-year-old subject. (a) T2w TIRM image shows a smoothly demarcated lesion of predominantly high signal intensity. (b) On the T2w TSE image, the bright cyst fluid is surrounded by a hypointense rim. (c) On the T1w image, the cyst fluid has low signal intensity, and the rim appears bright
MRI Features
T2-weighted images:
Bright, fluid-filled, round, or oval mass.
High protein content results in lower signal intensity.
Thin septa may be present.
Non-contrast-enhanced T1-weighted images:
Sharply demarcated, dark lesion.
High protein content or blood in the cyst fluid can lead to markedly higher signal intensity (Uematsu and Kasami 2009b).
Contrast-enhanced T1-weighted images:
Differential Diagnosis
Simple cyst (see preceding section; no enhancement of cyst content or wall; very bright on T2-weighted image and dark on T1-weighted image)
Abscess (often accompanied by erythema, skin thickening, and edema; typically located close to the nipple; thickened wall)
Invasive ductal carcinoma (see below; if there is central necrosis, invasive ductal carcinoma may be mistaken for a complex cyst; rim enhancement may be seen, typically when there is wall thickening (>2 mm))
Fibroadenoma (see below; enhancement is strong in juvenile adenoma, while adult fibroadenoma is characterized by little initial enhancement and a continuous increase thereafter)
Clinical Management
Sharply demarcated cysts are classified as BI-RADS 2 and can be left alone. There is no risk of malignant transformation. Complex cysts are categorized as BI-RADS 3 and require further evaluation. Workup should include ultrasound-guided aspiration of cyst fluid for cytologic examination.
11.2.3 Intramammary Lymph Nodes
An intramammary lymph node is an oval mass with smooth borders in the breast parenchyma (Fig. 11.3). Histologically, it is identical to lymph nodes elsewhere in the body (Table 11.5). Intramammary lymph nodes can be found anywhere in the breast but are most common in the upper outer quadrant. As a rule, they are not palpable (Iglesias et al. 2007). As with other normal lymph nodes, they are characterized by the presence of a fatty hilum (Schmidt et al. 2001; Spillane et al. 1999).
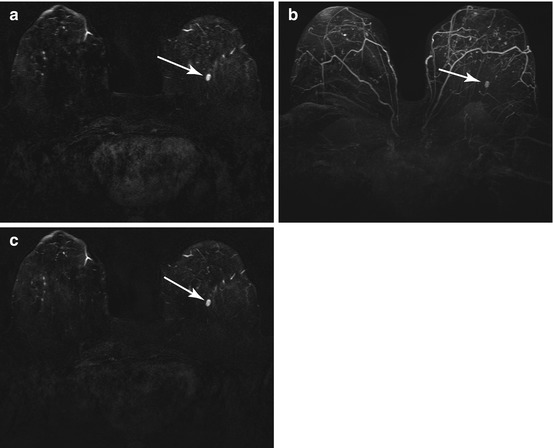
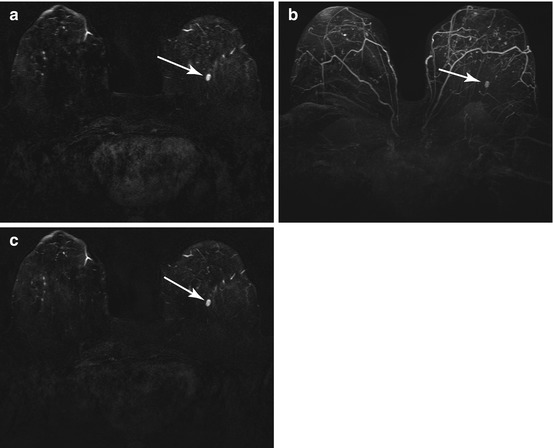
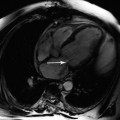
Fig. 11.3
Intramammary lymph node (arrow) in a 63-year-old subject. Contrast-enhanced T1w series. (a) Early postcontrast subtraction image. (b) Maximum intensity projection (MIP). (c) Late postcontrast subtraction image
Table 11.5
Intramammary lymph nodes
Frequency | 47 % of all women |
Age predilection | All ages |
Type of lesion | Benign; harmless incidental finding |
Signs and symptoms | No typical clinical presentation |
MRI Features
T2-weighted images:
Intermediate or high signal intensity, which, in some cases, may be confined to the margin.
On fat-suppressed images, the fatty hilum shows loss of signal intensity.
Non-contrast-enhanced T1-weighted images:
An intramammary lymph node within the parenchyma may be indistinct from the surrounding tissue.
Outside the parenchyma, an intramammary lymph node is depicted as an oval, smooth mass of lower signal intensity.
Hilar fat may appear bright.
Contrast-enhanced T1-weighted images:
Typically no or very little contrast enhancement.
In case of reactive inflammation, an intramammary lymph node may show rapid and strong enhancement, mimicking the enhancement kinetics of malignant breast lesions (Iglesias et al. 2007).
Reactive inflammation of an intramammary lymph node may lead to rim enhancement sparing the fatty hilum
Differential Diagnosis
Other well-circumscribed, encapsulated masses containing fat
Examples include lipoma, fibroadenolipoma, galactocele, and clusters of cysts embedded in fat
Other well-circumscribed, noncalcified masses
Cysts, fibroadenoma, lymphoma, and metastasis (rare)
Clinical Management
An intramammary lymph node is assessed as BI-RADS 2, meaning that no further workup is needed. It is typically a harmless, incidental finding and has no malignant potential. Metastasis in an intramammary lymph node is extremely uncommon.
11.2.4 Fibroadenoma
Breast fibroadenoma is a mixed fibroepithelial tumor. The juvenile type of this benign tumor, occurring in younger women, has a large epithelial component (Fig. 11.4).
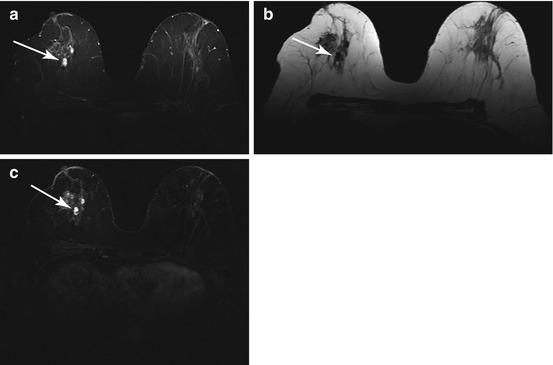
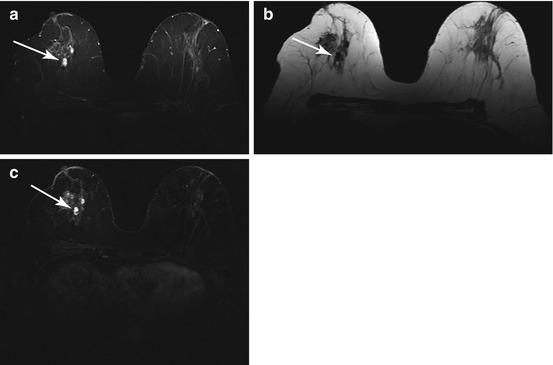
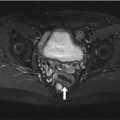
Fig. 11.4
Juvenile fibroadenomas (arrow) in a 33-year-old subject. (a) Conspicuous small foci of high signal intensity on T2w TIRM image. (b) The foci have low signal intensity on unenhanced T1w image. (c) Subtracted postcontrast T1w image shows strong enhancement of the lesions
The fibrous component increases with age, undergoes progressive hyalinization and calcification, and becomes predominant in postmenopausal women (Fischer 2000; Kuusk 1988) (Fig. 11.5). Fibroadenomas account for 75 % of all breast lesions. They are multiple in approx. 25 % of cases (Table 11.6). Women with adult fibroadenoma have an increased risk of breast cancer (Dupont et al. 1994; McDivitt et al. 1992).
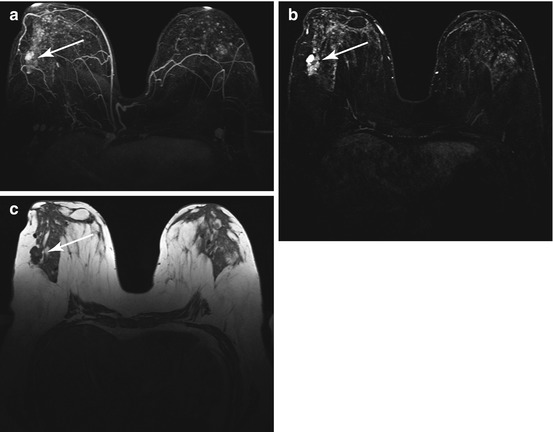
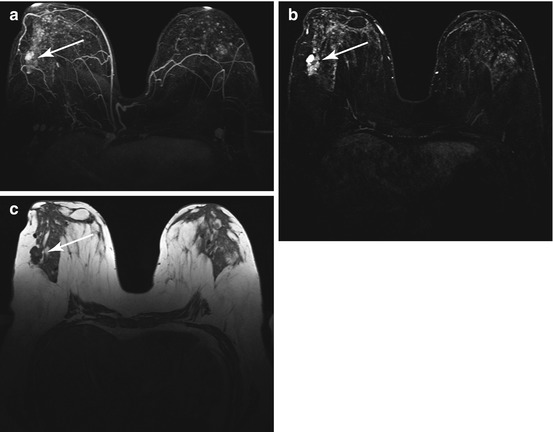
Fig. 11.5
Adult fibroadenoma in a 55-year-old subject. (a, b) Contrast-enhanced T1w imaging (MIP and subtracted image) shows inhomogeneous enhancement of the lesion with areas of strong and less strong contrast medium uptake (arrow). (c) Unenhanced T1w image depicts a lobulated focal lesion of predominantly low signal intensity (arrow)
Table 11.6
Fibroadenoma
Frequency | 10 % of all women (most common benign breast tumor) |
Age predilection | Occurs at any age, most common between 20 and 50 years |
Type of lesion | Benign |
Signs and symptoms | Small fibroadenoma is not palpable |
Larger fibroadenoma is palpable as a circumscribed, painless, movable lump |
MRI Features
T2-weighted images:
Juvenile fibroadenomas have high signal intensity, making them difficult to differentiate from cysts
Adult fibroadenomas, containing a large amount of fibrous tissue, are usually isointense and occasionally hypointense to breast parenchyma
Non-contrast-enhanced T1-weighted images:
Smooth round, oval, or lobulated mass of parenchymal signal intensity (adult type) or slightly lower signal intensity (juvenile type); hence, fibroadenoma is more difficult to identify on T1-weighted images unless it is surrounded by fatty tissue (Uematsu and Kasami 2009a)
Contrast-enhanced T1-weighted images:
Enhancement is highly variable due to the inhomogeneous composition of fibroadenomas
Strong and rapid enhancement of juvenile fibroadenomas as a result of the large epithelial component (Hirose et al. 2007)
As the amount of fibrous tissue increases in older tumors, enhancement may be less strong and more inhomogeneous; internal septa do not take up contrast medium
Differential Diagnosis
Papilloma (see below; similar contrast enhancement as juvenile fibroadenoma, i.e., strong enhancement, especially in the initial phase, and low T1 and high T2 signal intensity on unenhanced images)
Invasive papillary carcinoma (1–2 % of all breast cancers, peak between 50 and 60 years; fingerlike projections, often with cystic component, can develop from benign papilloma; unenhanced T1-weighted images, oval, lobulated, or irregular focal lesion of low signal intensity, with unsharp borders, rarely smooth borders; contrast-enhanced images, typically moderate or strong initial enhancement with later plateau or washout, rarely rim enhancement; T2-weighted images, moderate signal intensity with cystic component, if present, appearing bright) (Brookes and Bourke 2008; Fischer 2000)
Complex cyst (see above; inhomogeneous signal, low T1 signal intensity with hyperintensities indicating protein accumulation or hemorrhage)
Tubular adenoma (benign; contrast enhancement similar to juvenile fibroadenoma, typically well-demarcated round or oval focal lesion) (Soo et al. 2000)
Medullary or mucinous breast cancer (rare) (unenhanced T1-weighted images: star-shaped mass of low signal intensity; T2-weighted images: intermediate or slightly lower signal intensity than glandular parenchyma; contrast-enhanced images: strong initial enhancement, typically followed by postinitial plateau, rarely by washout) (Uematsu and Kasami 2009a)
Clinical Management
If the lesion is small and the MRI findings are consistent with fibroadenoma, it is classified as BI-RADS 2, and no diagnostic workup is necessary.
If the lesion is larger and the MRI findings are inconclusive, it is classified as BI-RADS 3, and further testing, including mammography and ultrasound, is recommended. A percutaneous biopsy should be obtained for confirmation.
11.3 Benign Breast Lesions with Increased Malignant Potential
11.3.1 Radial Scar
A radial scar consists of a fibroelastic (retracted) core surrounded by a stellate pattern of emanating ducts displaying variable epithelial hyperplasia and papillomatosis (Fig. 11.6 and Table 11.7). It has been attributed to chronic infection and reduced perfusion. Transition to tubular carcinoma is possible (Fischer 2000; Jacobs et al. 1999). Because of its malignant potential, surgical removal is recommended in most cases (Pediconi et al. 2005).
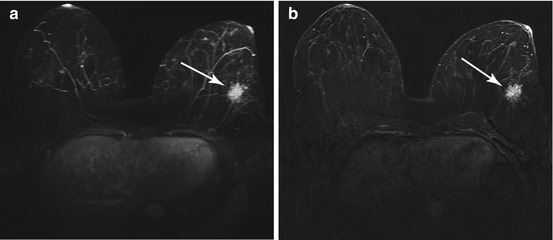
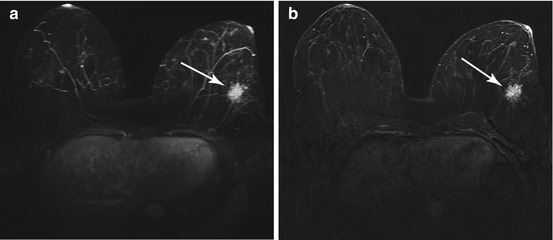
Fig. 11.6
Radial scar (arrow) in a 39-year-old subject on contrast-enhanced T1w images. (a) Maximum intensity projection (MIP). (b) Late postcontast substraction image shows an enhancing, spiculated mass in the left breast
Table 11.7
Radial scar
Frequency | Rare |
Age predilection | All ages |
Type of lesion | There is an association with malignancy, especially for radial scars >2 cm; transition to tubular carcinoma is possible |
Signs and symptoms | Typically not palpable; often presents as an incidental finding on mammogram |
MRI Features
T2-weighted images:
No characteristic features; often not apparent on fat-saturated T2-weighted images
Non-contrast-enhanced T1-weighted images:
Star-shaped lesion with the same signal intensity as parenchyma
Therefore difficult to identify when surrounded by parenchyma
Easily seen when surrounded by fatty tissue
Contrast-enhanced T1-weighted images:
Typically little or moderate contrast uptake within the star-shaped lesion (Pediconi et al. 2005)
An occasional radial scar may show rapid initial enhancement
May be difficult to differentiate from breast cancer
Differential Diagnosis
Ductal carcinoma in situ (DCIS) (see below; not apparent on T1- and T2-weighted images; on contrast-enhanced images, DCIS tends to lack the kinetic enhancement pattern of malignancy, but may occasionally show focal enhancement)
Invasive ductal carcinoma (see below; T1-weighted images: irregularly shaped, spiculated mass; T2-weighted images: intermediate or low signal intensity; postcontrast images: strong initial enhancement with postinitial plateau or washout, irregular and often rim enhancement)
Tubular breast cancer (rare) (can arise from radial scar; star-shaped lesion of low T1 signal intensity; T2-weighted images: intermediate or slightly lower signal intensity than glandular parenchyma, sometimes with hyperintense peritumoral edema; postcontrast images: spiculated focal lesion, often with strong initial enhancement followed by postinitial plateau, less often by washout, nonspecific enhancement may also occur) (Fischer 2000)
Postoperative scar
Clinical Management
A radial scar is classified as BI-RADS 4b because malignancy cannot be reliably excluded. This means that the finding should be communicated for prompt workup. Biopsy is recommended. If biopsy demonstrates atypia, the lesion should be excised.
11.3.2 Papilloma
Breast papillomas are intraductal tumors made up of benign epithelial cells (Fischer 2000). Central papillomas tend to be solitary and are often located behind the nipple. Bloody, milky, or clear nipple discharge is the presenting symptom in most women. Multiple papillomas are small and peripheral in location (Francis et al. 2002; Kramer et al. 2000) (Table 11.8).
Table 11.8
Papilloma
Frequency | Rare, 1–2 % of all benign tumors |
Age predilection | 40–50 years |
Type of lesion | Benign; increased risk of transformation to DCIS or papillary breast carcinoma; the risk is 10–33 % if multiple papillomas are present |
Signs and symptoms | Spontaneous or provoked nipple discharge, which may be bloody, milky, or clear |
MRI Features
T2-weighted images:
Signal intensity varies with lesion size: small papillomas tend to have intermediate or high signal intensity, while large papillomas typically have moderate and sometimes low signal intensity
Non-contrast-enhanced T1-weighted images:
Focal lesion of low signal intensity, same as glandular parenchyma and therefore often difficult to identify
Contrast-enhanced T1-weighted images:
Smooth tumor with homogeneous or inhomogeneous contrast enhancement.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree