Multiple sclerosis (MS) pathology is originally defined by the presence of focal white matter lesions, characterized by inflammation, primary demyelination, and reactive glial scaring. More recently, however, it became clear that focal white matter plaques in MS comprise of a broad spectrum of different lesion types, reflecting different stages of activity and different degrees of neurodegeneration or repair. In addition, the MS brain is affected by global changes in the normal-appearing white matter and gray matter. All types of changes in the MS brain and spinal cord occur on the background of inflammation; the type of inflammation, however, differs between different stages and forms of the disease.
Multiple sclerosis (MS) is defined as an inflammatory demyelinating disease of the central nervous system (CNS). Its pathologic hallmark is the presence of focal demyelinated plaques with reactive glial scaring in the white matter of the brain and spinal cord. Seminal studies, performed in the late nineteenth and early twentieth centuries have defined the key pathologic features of the disease. The studies showed that demyelinated lesions develop around small veins and venules and occur on the background of an inflammatory reaction, mainly composed of lymphocytes and macrophages. Primary demyelination, as defined by selective destruction of myelin with preservation of axons, is the dominant structural alterations within MS plaques; the process of demyelination is accompanied by reactive astrocytic scar formation. Axons are preserved within the lesions in relation to the complete myelin destruction, but this preservation is not absolute. In fact, axonal injury and loss are seen in all MS lesions; the degree, however, is highly variable. In addition to these destructive aspects in MS lesions, there are also attempts of remyelination and repair. Signs of remyelination, defined by the appearance of newly formed thin myelin sheaths with widened nodes of Ravier can be seen quite frequently even in newly formed lesions. In addition, shadow plaques, defined by a global appearance of thin myelin sheaths throughout the whole lesion, suggest that whole MS lesions can be repaired by remyelination.
For more than one hundred years, this plaque-centered view was regarded sufficient to explain the pathology of MS. It allowed clinicians to distinguish MS from other inflammatory diseases of the CNS. The perspective, at least in part, explained the clinical deficits of the patients and it was generally believed that preventing the formation of new demyelinating lesions in the CNS should stop the disease process. During recent decades, however, this view was fundamentally challenged by clinical studies on the natural course of the disease and on the response to disease modifying treatments. Most importantly, recent observations, obtained in cross-sectional and longitudinal studies, on the development of brain changes seen by magnetic resonance (MR) imaging, suggest, that MS pathology is much more complicated than it was assumed before. These observations, which were unpredicted by previous disease concepts, stimulated extensive research efforts to redefine MS pathology, in particular focusing on alterations, affecting the brain and spinal cord outside classical white matter plaques. From these investigations, it became clear that the CNS of MS patients is affected not only by white matter plaques but also by global changes in the gray matter and the normal-appearing white matter (NAWM). Furthermore, longitudinal MR imaging studies revealed dynamic changes within the classical MS plaques, for which the pathologic substrate had still to be elucidated.
Focal white matter lesions
Focal MS lesions can be present in any location of the CNS. However, since they arise around veins and venules, areas of the CNS with high venular density are more frequently affected than others. Such predilection sites are the periventricular and the subcortical white matter of the forebrain, the optic nerves and chiasm, the cerebellar peduncles and the lateral columns of the spinal cord.
MS plaques are sharply demarcated focal white matter lesions, characterized by primary demyelination, a variable extent of axonal injury and reactive astrocytic scar formation. Several different types of lesions can be distinguished. Active lesions contain numerous inflammatory infiltrates, which are mainly composed of T- and B-lymphocytes, some plasma cells, and activated macrophages or microglia cells. Remnants of the myelin sheaths or of destroyed axons are contained within the lysosomes of macrophages; the molecular composition of the degradation products can be used to define stages of demyelinating activity within a given lesion. In inactive lesions, inflammation is sparse. The cell density in the inactive lesions is low, due to the profound loss of oligodendrocytes. Demyelinated fibers are embedded in a glial scar, formed by densely packed fibrillary astrocytic cell processes. In remyelinated lesions or lesion areas, myelin sheaths are surrounded by unusually thin myelin sheaths, which frequently show widened nodes of Ranvier. The cell density in remyelinated lesions, in general, is high and the number of oligodendrocytes may even exceed that seen in the surrounding NAWM. Fully remyelinated plaques are sharply demarcated areas with reduced myelin density, due to the homogeneously thin myelin sheaths throughout the plaque. Such lesions are called “shadow plaques.”
MR imaging, even when restricted to the analysis of conventional T2-weighted images, is very sensitive in regard to detecting focal white matter lesions. Indeed, early studies, correlating T2 images with pathology showed good agreement in the detection of white matter plaques. However, when postmortem MR imaging was performed and T2 lesion areas were specifically sampled for pathologic analysis, the situation became more complicated. In the study by Barkhof and colleagues, 161 T2 lesion areas were sampled. From those, 78% revealed focal white matter lesions. Based on the T2 signal, it was, however, not possible to distinguish demyelinated from partially or fully remyelinated lesions. Furthermore, 22% of the lesion areas which were identified by MR imaging showed no pathologic substrate and, in particular, no demyelination.
There are several possible explanations for this unexpected finding. First, it is possible that remyelination in MS lesions may become so complete that a reduction of myelin density due to the thinly remyelinated fibers is no longer visible. Currently, neuropathology does not offer a technique to unequivocally prove or disprove this scenario. Alternatively, these abnormal T2 areas shown in MR imaging may reflect a subtle pathology, which currently escapes neuropathological detection. One such subtle pathology may be focal areas of edema. A similar problem with the correlation between MR imaging and pathologic findings is also seen in leukoarayosis.
Axonal injury and widening of the extracellular space
Axonal destruction within the plaques is an important feature of MS pathology because axonal destruction appears to be the major substrate for permanent functional deficit. The extent of axonal destruction is variable between different lesions within a given patient and between different patients; the variation ranges from 20% to more than 80%. Most pronounced acute axonal injury occurs during the active stage of the lesion. In active lesions, an average reduction of axonal density by 30% may be seen, which is in part due to true axonal destruction, but also in part to inflammation and edema, which is pronounced during this stage. A partial normalization of axonal density values is generally seen, when lesions mature, due to the clearance of edema. Therefore, the average axonal loss in lesions in the late active stage is only between 10% and 20%. Similar values for axonal density are also seen in remyelinated shadow plaques. Within permanently demyelinated lesions, which are present in the late chronic stage of the disease, axonal loss is much more dramatic. In such lesions, axonal density is reduced on average by 60% to 70%. These data indicate that, in MS lesions, two different patterns of axonal injury occur. Massive and synchronous axonal injuries occur during the active stage of the lesions, while there is a further accumulation of axonal loss in demyelinated plaques at late stages. Whether this chronic loss of axons is due to repeated demyelination of remyelinated lesion areas or to a slow and continuous injury of chronically demyelinated axons is not yet clear. It should, however, be emphasized that active axonal injury in the acute stages, as well as in the late chronic stage, is invariably associated with inflammation and microglia activation.
Demyelination and axonal loss within MS lesions are associated with a widening of the extracellular space, which in extremely destructive lesions may be reflected in cystic tissue necrosis. This widening of the extracellular space seems to have a correlate in the reduced density within lesions in T1-weigted scans. In fact, quantitative MR imaging and pathology reveal that the extent of T1 signal reduction in part correlates with the degree of axonal loss in the lesions. It has, however, to be emphasized that tissue loss and widening of the extracellular space is due to axonal and myelin loss as well as to edema. All three factors, therefore, may influence dynamic changes of T1 signal intensity during lesion evolution.
Axonal injury and widening of the extracellular space
Axonal destruction within the plaques is an important feature of MS pathology because axonal destruction appears to be the major substrate for permanent functional deficit. The extent of axonal destruction is variable between different lesions within a given patient and between different patients; the variation ranges from 20% to more than 80%. Most pronounced acute axonal injury occurs during the active stage of the lesion. In active lesions, an average reduction of axonal density by 30% may be seen, which is in part due to true axonal destruction, but also in part to inflammation and edema, which is pronounced during this stage. A partial normalization of axonal density values is generally seen, when lesions mature, due to the clearance of edema. Therefore, the average axonal loss in lesions in the late active stage is only between 10% and 20%. Similar values for axonal density are also seen in remyelinated shadow plaques. Within permanently demyelinated lesions, which are present in the late chronic stage of the disease, axonal loss is much more dramatic. In such lesions, axonal density is reduced on average by 60% to 70%. These data indicate that, in MS lesions, two different patterns of axonal injury occur. Massive and synchronous axonal injuries occur during the active stage of the lesions, while there is a further accumulation of axonal loss in demyelinated plaques at late stages. Whether this chronic loss of axons is due to repeated demyelination of remyelinated lesion areas or to a slow and continuous injury of chronically demyelinated axons is not yet clear. It should, however, be emphasized that active axonal injury in the acute stages, as well as in the late chronic stage, is invariably associated with inflammation and microglia activation.
Demyelination and axonal loss within MS lesions are associated with a widening of the extracellular space, which in extremely destructive lesions may be reflected in cystic tissue necrosis. This widening of the extracellular space seems to have a correlate in the reduced density within lesions in T1-weigted scans. In fact, quantitative MR imaging and pathology reveal that the extent of T1 signal reduction in part correlates with the degree of axonal loss in the lesions. It has, however, to be emphasized that tissue loss and widening of the extracellular space is due to axonal and myelin loss as well as to edema. All three factors, therefore, may influence dynamic changes of T1 signal intensity during lesion evolution.
Remyelination
Although evidence for remyelination in MS lesions has been provided in the earliest neuropathological accounts of this disease, it was believed for a long time, that repair of myelin is sparse or absent in white matter lesions of the CNS. However, systematic ultrastructural studies provided unequivocal evidence for myelin repair within the lesions. Furthermore, these studies showed that remyelinated lesions may become affected by new demyelinating attacks. Remyelination is seen in parts of the lesions or it may lead to complete restoration of myelin within the entire plaque. Recruitment of new oligodendrocytes and formation of new thin myelin sheaths are frequent findings in most MS lesions in early stages of lesional activity. This early stage of remyelination occurs on the background of massive macrophage infiltration within the lesions. Based on these findings, it was suggested that remyelination is extensive in the early stage of MS, where classical active lesions are frequently seen, but that remylelination fails in the later progressive stage of the disease.
A systematic analysis of stable remyelination, which was seen in the form of shadow plaques or plaque areas, revealed a different picture. Extensive remyelination is seen in a subset of patients, although other patients show very little myelin repair; ( Fig. 1 ). In fact, MS patients can be separated into two distinct groups. In one group, extensive remyelination was seen in most lesions, with the exception of those that were still in the process of active demyelination. In others, remyelination was sparse and was restricted to small areas at the plaque margins. Contrary to previous views, the most extensive remyelination was seen in patients who were dying at very old ages and with long-standing disease. These data indicate that remyelination is initiated in the early stages of lesion formation in many cases, but this newly formed myelin may be instable and subject to subsequent demyelination. Only when the inflammatory disease process becomes inactive, remyelination may become stable and permanent. However, remyelination is extensive in some patients, but fails in others. The reason for these interindividual differences is so far unknown.
Although there is no specific MR imaging sequence that distinguishes remyelinated from demyelinated areas in MS brains, indirect information about remyelination can be obtained by assessing dynamic changes in T1-weighted scans or in voxel-based analysis of magnetization transfer ratio (MTR) changes. Using this technology, it was shown recently that, within a given patient, the dynamic changes within multiple lesions are strikingly similar and, in a subset of patients, lesions changed from hypointense to isointense on T1-weighted scans. These data are consistent with neuropathological findings that suggest pronounced remyelination in a subpopulation of MS patients.
Blood brain barrier damage and inflammation
Assessing blood–brain barrier (BBB) damage in MS lesions through the leakage of gadolinium (Gd) became a very useful tool to determine the activity of the disease process in clinical diagnosis and therapeutic trials. There is good agreement between studies showing that Gd-enhancement is a characteristic feature of newly forming lesions in the brain and spinal cord. Brain biopsies in early MS lesions have shown that Gd-enhancement is associated with inflammation. Based on these observations, a common dogmatic view has been established that equates Gd-enhancement with inflammation in the MS brain. This view, however, is incorrect and misleading.
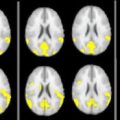
Neuropathological studies have provided ample evidence that the BBB is disturbed in MS not only in active lesions, but also in inactive plaques and in the NAWM. There is, however, a difference in the degree of BBB disturbance, it being most pronounced in classical active plaques. Thus, the selective Gd-leakage in active MS lesions is due to the low sensitivity of this technique to detect changes in BBB alterations ( Fig. 2 ).
Even more complicated is the relation between BBB disturbance and inflammation ( Fig. 3 ). In classical active MS plaques, massive BBB disturbance is seen and this is generally associated with intravascular and perivascular inflammatory infiltrates. However, in the vicinity of active lesions, numerous vessels are seen that show profound leakage of serum protein and evidence for leaky endothelial cells in the absence of inflammatory infiltrates. It is likely that, in such vessels, BBB function is disturbed by soluble inflammatory mediators that are liberated from inflammatory cells in the adjacent lesions. Despite this dissociation between inflammation and BBB damage in individual vessels, these data are still consistent with MR imaging observations, linking active lesions with Gd-enhancement.
The situation, however, is different in the late (progressive) stage of the disease where Gd-enhancing lesions are rare or absent. However, there is pronounced inflammation within the brain tissue in such patients, which is reflected by perivascular inflammatory cuffs as well as by diffuse infiltration of the tissue by lymphocytes and macrophages. Mild disturbance of the BBB, which seems to be below the detection limit of Gd-enhancement, is seen in some of the inflamed or not inflamed vessels at this stage. In addition, many vessels with profound perivascular inflammatory infiltrates are seen that do not show any evidence for increased permeability (see Fig. 3 ). At this stage of the disease, inflammation also accumulates in the meninges and perivascular spaces in the form of lymph follicle–like structures. Thus, in the progressive stage of MS, inflammation becomes trapped or compartmentalized behind a closed or repaired BBB. Lack of Gd-enhancement in the progressive stage of MS does not mean that there is an absence of inflammation. This is important to consider when discussing MS-based neurodegeneration in relation to inflammation.
BBB damage and active demyelination
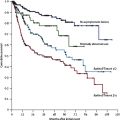
Active white matter lesions, which are defined by Gd-enhancement, are frequent in the early stages of MS, but they are rather rare in the progressive stage. In the progressive stage, up to three enhancing lesions have been described per scan and time point in the entire brain . In contrast, in pathology, active demyelination is described in more than 50% of all lesions in patients with primary or secondary progressive MS. Thus, there is a major discrepancy between the active lesions seen on MR imaging scans in progressive MS and those lesions identified within comparable brains by pathology.
This discrepancy may be partly explained by the fact that pathology allows researchers to distinguish between different types of active MS lesions ( Fig. 4 ). Classical active lesions are characterized by pronounced inflammation and extensive BBB damage. They are infiltrated by macrophages throughout the lesion and, depending upon the time after onset of demyelination, these macrophages contain myelin degradation products in different stages of digestion. Such lesions apparently represent those seen on MR imaging scans with homogeneous Gd-enhancement. Other classical, active plaques have a peripheral rim of ongoing myelin destruction that, similarly to other classical active plaques, show dense inflammatory infiltrates and a broad rim of activated macrophages. The center of these lesions is also densely packed with macrophages, but these cells contain late (sudanophilic) remnants of myelin degradation such as cholesterol and free fatty acids. Such lesions, in general, show ring enhancement and a small hypointense rim in T2-weighted images, delineating the zone of dense macrophage infiltration. Classical active lesions, as described here, are mainly found in patients with acute and early relapsing disease, but they are rare in patients with progressive MS.
The other type of actively demyelinating lesions is the slowly expanding pre-existing plaque. Such lesions have an inactive center, which is surrounded at the plaque margin by a rim of densely packed activated microglia cells and a low to moderate number of macrophages (see Fig. 4 ). Only few of the macrophages and activated microglia cells contain early myelin degradation products, suggesting a very slow, active expansion of the lesions. Inflammation and BBB damage in such lesions is generally mild. It is thus unlikely that such lesions show Gd-enhancement at least when standard doses of contrast material are used. Slowly expanding lesions are already present in the brains from patients with relapsing-remitting MS, but they become the dominant active lesions in patients with progressive MS. Thus, in practical terms, the absence of Gd-enhancement on MR imaging scans does not necessarily mean that the corresponding lesions are inactive in terms of inflammation, ongoing demyelination, or tissue injury.
Focal white matter changes preceding the appearance of a demyelinating lesion
For a long time, it was assumed that focal disturbance of the BBB, as seen on Gd-enhanced MR imaging scans, is the initial event in the formation of a new white matter lesion of MS. However, subsequent studies, performing serial MR imaging investigations separated by small time intervals, showed that, at least in some lesions, subtle changes in the white matter can be seen in areas, which days to weeks later develop into classical Gd-enhancing active lesions. These changes consisted of reduction of the MTR signal and a mild to moderate reduction of N-acetyl aspartate. These observations suggested that subtle changes within the tissue may precede inflammation in MS plaques.
In an attempt to define the pathologic substrate of such lesions, De Groot and colleagues analyzed the neuropathology of white matter areas that were abnormal on T2-weighted MR imaging scans. They identified a specific lesion type, described as (p)reactive lesions, which was characterized by mild inflammation, edema, and microglia activation, in patients with progressive MS. The incidence of such lesions within the brains, however, was more than 25% of all lesions analyzed, and was thus much higher than expected for initial stages of active plaques in patients with late progressive disease. No attempts were made to differentiate in these (p)reactive lesions areas from remyelination or secondary (Wallerian) tract degeneration.
A different approach was taken by Barnett and Prineas. They described the pathology in the brain stem of an individual MS patient, who died within a few days after the onset of a new attack of the disease. The authors found, besides classical active lesions, areas of microglia activation and oligodendrocyte apoptosis surrounding the established demyelinating plaque. Inflammation in these areas of oligodendrocyte death was sparse and restricted to the perivascular space. The authors also found similar lesion areas in other patients with active disease. From these data, it was concluded that the earliest stages of the formation of MS lesions may be driven by microglia activation and may be independent from lymphocytic inflammatory infiltrates.
A more recent study addressed this question by analyzing the global pathology of the brain in patients dying in the course of fulminating MS, using an approach that was similar to that described by Barnet and Prineas, but using large hemispheric or double hemispheric brain sections. In such patients, multiple active lesions develop in a very short time window of a few weeks to months and, therefore, the chance to find initial tissue alterations, preceding the formation of new classical plaques, is high. The authors found areas of tissue alteration either in close vicinity to active plaques or even topographically unrelated to existing plaques that fulfilled the criteria for initial lesions predicted by MR imaging studies. In these areas, there was a mild perivascular inflammatory reaction associated with mild edema and BBB damage, which is likely to be below the threshold of detection by Gd-enhancement. Precipitation of fibrin adjacent to the surface of microglia was associated with profound expression of inducible nitric oxide synthase and myeloperoxidase. In addition, there was a moderate acute axonal injury, seen by the accumulation of amyloid precursor protein within the axoplasm. Such pre-lesional tissue alterations were only found in a subset of MS patients, in whom demyelinated plaques follow a hypoxia-like tissue injury (pattern III), but not in patients with other patterns of demyelination. In patients following pattern II (antibody and complement associated demyelination), inflammation, demyelination, and tissue injury occurs in parallel. Thus, in such lesions, inflammation and massive BBB damage is the earliest event in lesion development.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree