Introduction
The spinal motion segment consists of the diskovertebral joint and the zygapophyseal joints of two adjacent vertebrae and their connecting ligamentous tissues. Each motion segment has six degrees of freedom of movement and rotation,1 and restriction of this motion will alter the biomechanical transmission of compressive, tensile, and rotational forces across the spine. Disorders with progressive ankylosis of the motion segments restrict normal compliance and predispose the rigid spine to fractures with a higher incidence of neurological complications than in the normal population.2,3 Ankylosing spondylitis (AS) and disseminated idiopathic skeletal hyperostosis (DISH) are the most common acquired etiologies of the rigid spine.4,5 Congenital failures of segmentation in the spine and operative spinal fusion also contribute to an increased susceptibility to fracture.2,6
Ankylosing Spondylitis
Ankylosing spondylitis begins with sacroiliitis, enthesopathic inflammation, and formation of syndesmophytes or thin vertical ossifications within the outer annulus fibrosis at the diskovertebral junction. There is progressive calcification and ossification of the posterior ligaments and the capsule of the facet joints, predominately involving the interspinous and supraspinous ligaments within multiple motion segments of the spine. The thoracic and lumbar spine are typically affected earlier than the cervical spine,4 however, cervical ankylosis is reported to develop in 75% of patients whose disease duration is 16 years or greater.7 The prevalence of AS is estimated to be approximately 1-2% of the population.4
Disseminated Idiopathic Skeletal Hyperostosis
The prevalence of DISH has been estimated to be 25% in men over 50 years of age, 35% in men over the age of 70, and 15% in women over 50 years of age.8 Fractures in patients with DISH are consequently more commonly seen than in patients with AS.
The radiological diagnosis of DISH includes flowing ossification or calcification across the anterolateral aspect of four or more contiguous vertebral bodies in the absenceof extensive degenerative diskopathy (such as vacuum gas, significant loss of disk height or marginal body sclerosis), the absence of apophyseal joint ankylosis and erosion, or intraarticular osseous fusion of the sacroiliac joints. Involvement of the mid and lower thoracic spine is most frequent, followed by the upper lumbar spine and the mid and lower cervical spine.5 Although the diagnostic criteria requires ankylosis across three consecutive disk spaces, enthesopathic ossification may involve less than four contiguous vertebral bodies and in some patients, the features of both AS and DISH in the spine may coexist.
While extensive ossification within adjacent motion segments may be present throughout the spine in both AS and DISH there are differences in the anatomical site of ligament ossification as well the extent of extraosseous enthesopathic ossification. As the syndesmophytes of AS become more extensive, a thin continuous undulating contour or bamboo spine is formed. There is progressive ossification of the posterior ligaments including the ligamentum flavum and the capsule of the apophyseal joints with ankylosis of the facet joints in more advanced AS.4
The apophyseal joints are uninvolved with DISH, and ankylosis of the ligamentum flavum and supraspinous ligaments is less commonly seen. Anterior longitudinal ligament and anterolateral paravertebral calcifications or ossifications are generally thicker and may be up to 20 mm thick in the thoracic and lumbar spine and 12 mm in the cervical spine in DISH. Ossification of the posterior longitudinal ligament (OPLL) of the cervical spine may present in patients with DISH, and is less frequently seen in the thoracic spine.5 OPLL is uncommon in AS, although quadriplegia has been described as a complication of cervical trauma with this combination.9
Mechanisms and Imaging Techniques
In the presence of multi-segmental ankylosis, the action of compressive, tensile, and shear forces on the spine resembles an extended lever arm of a long bone of the appendicular skeleton.10 These injuries cause shearing, axial, or oblique transverse fractures with failure in tension of the ossified ligaments and disk, or across the vertebral body with an associated fracture of the posterior column. Fractures are distracted anteriorly with an extension injury, or posteriorly with a flexion injury. Since the nucleus pulposus is frequently preserved, a herniation of the nucleus pulposus with fractures traversing the disk may cause nonosseous cord compression. Long segments of ankylosis with AS or DISH renders the spine more prone to fracture, especially in the presence osteoporosis. While a highvelocity traumatic impact frequently results in significant injury, there is commonly a history of relatively low-velocity impact or minor trauma, such as a fall from an upright or seated position at ground level or a history of a glancing blow to the head. New onset of neck, thoracic, or lower back pain even in the absence of any trauma should prompt an imaging investigation for an insufficiency fracture.10,11

Fig. 10.1 Transverse fracture within a congenital thoracic anterior nonsegmented bar in a 26-year-old man involved in a nonconstrained motor vehicle accident. The image shows a sagittal T2W MRI of the thoracic spine. There is increased signal in a transverse fracture of the body of T9 subjacent to the T8-T9 disk within a congenital nonsegmented bar involving T9-T12. The disruption of the posterior ligaments at T8-T9 and anterior widening of the fracture indicate an extension tensile injury.
Conventional radiographs are the first imaging modality performed on patients sustaining minor trauma or complaining of neck pain. However, the lower cervical and cervicothoracic spine are frequently obscured due to the overlying shoulders, and the lack of mobility and often exaggerated cervicothoracic kyphosis limits the usefulness of the swimmers lateral projection. Oblique projections, however, may demonstrate a fracture across the posterior arch. Severe osteoporosis, ossification of the ligaments, and annulus fibrosus distorting the landmarks may delay the diagnosis of bone injury in AS. The enthesopathy in DISH also leads to extensive ossification and calcification that obscures the normal vertebral anatomy. The suspicion of any discontinuity of the anterior vertebral cortex or ossified anterior longitudinal ligament or hyperostosis, particularly in the presence of widening of a portion, or all of the adjacent disk space, should prompt a search for a fracture in the posterior cortex of the vertebral body and the corresponding posterior arch and ossified ligamentous structures.
Cross-sectional imaging is increasingly utilized to corroborate and define the extent of the injury. Since as many as 40% of patients sustaining a cervical spine fracture have been reported to have multiple fractures within the cervical spine or the thoracic spine, additional imaging of the entire spine at presentation is essential.11 Patients with a severe kyphosis and a transverse fracture are at risk of further neurological injury when placed supine on a spinal board or a radiographic table by causing hyperextension of the fracture, and should be supported in a flexed position.12
The development of multi-channel/multi-detector spiral or helical CT scans has markedly improved the visualization of subtle fractures, and these scans have become routine in the assessment of the cervical thoracic junction when overlapping shoulder and other soft tissue densities preclude adequate visualization. Multi-planar high-resolution sagittal and coronal reformatted imaging is especially useful in demonstrating fractures that may be poorly seen in the axial transverse plane and has largely supplanted tomography.13–15
Multi-detector spiral CT scans with thin axial collimation and overlapping reconstruction increments of half a slice thickness allow post-processing of high resolution sagittal and coronal reformatted images that provide excellent bone detail in all planes of the cervical spine from the occiput through the upper thoracic spine. Evaluation of the thoracic and lumbar spine with high-resolution sagittal and coronal reformatted images may also obviate the need for conventional radiographs and CT scans have the advantage of scanning patients with a prominent thoracic kyphosis in the lateral decubitus position.14,15
MRI will demonstrate fractures, bone marrow hemorrhage, and contusion and is especially useful in detecting occult unsuspected fractures remote to the primary injury (Fig. 10.1). MRI is most sensitive in the detection of spinal cord contusion, intramedullary hematoma, and compression of the cord from an epidural hematoma, or displaced disk or bone fragments and is the preferred exam if neurological deficit is suspected.16,17
A mid-line sagittal STIR imaging series with a large field of view encompassing the cervical and upper thoracic spine in one sequence and the lower thoracic and lumbar spine on a second sequence has been advocated as a minimum screening MRI exam to detect the presence of intraosseous or intraspinal hemorrhage consequent to a fracture and to search for a second occult fracture.17,18 MRI examination sequences vary with institutional preference and also may include sagittal T1W spin-echo, sagittal T2W fast spinecho, sagittal inversion recovery (STIR), and sagittal gradient-echo with axial T1W spin-echo, T2W fast spin-echo, and gradient sequence images as well as sagittal and axial T1W fat-suppressed imaging following intravenous gadolinium.
Cervical Spine Injuries
Congenital failure of segmentation of one or more segments such as in the Klippel-Feil syndrome, or the presence of a previous surgical fusion, particularly in the cervical spine, transfers forces to an adjacent mobile spinal motion segment and predisposes these segments to clinical injury (Fig. 10.2).2,6
Patients with Klippel-Feil syndrome have been categorized into three main types:
- Type 1 anomaly: the nonsegmentation or congenital fusion is present in three or more levels of the cervical or upper thoracic spine.
- Type 2 anomaly: the nonsegmentation fusion anomaly is isolated to one or two levels in the cervical spine.
- Type 3 anomaly: the cervical fusion is associated with nonsegmentation in the lower thoracic or lumber spine.
The junctional mobile segments in this disorder have been shown to be hypermobile. This excess motion and segmental overload accelerate degenerative disk disease causing disk bulge and spinal stenosis predisposing to injury of the spinal cord (Fig. 10.3).2,6,19
Fractures of the odontoid process were associated with a fusion of the upper cervical spine, while singlelevel lower cervical spine fusion was associated with unilateral facet fracture-dislocation in 20 patients with congenital or post-surgical spinal fusion in a series of 368 patients with cervical spine injury.2
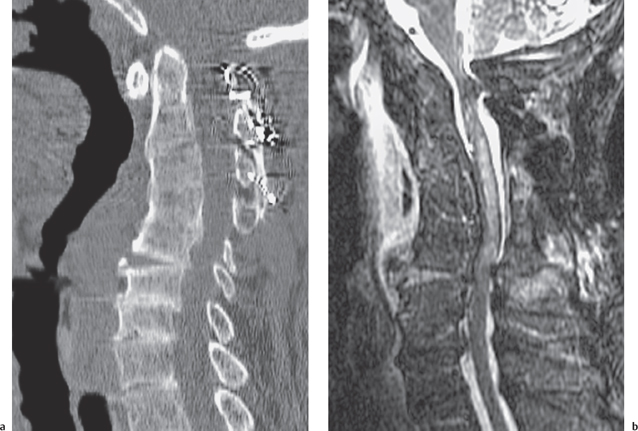
Fig. 10.2 Disk disruption below a cervical fusion in a 73year-old man involved in a motor vehicle accident. A central cord syndrome was diagnosed at presentation. a Sagittal CT scan of the cervical spine. A mature posterior interspinous fusion with cerclage wires and secondary anterior kyphotic ankylosis is seen at C2-C5, there is also anterior widening of the C5C6 disk. The subjacent disks are severely narrowed. b Sagittal STIR MR image of the cervical spine. Extensive prevertebral edema is associated with disruption of the C5-C6 annulus and anterior longitudinal ligament. Increased signal in the posterior column reflects the extension injury. Significant cord compression at C5-C6 is due to buckling of the ligamentum flavum and mild retropulsion of C5 on C6. Fluid signal within the central spinal cord reflects cord contusion. No signal abnormality was seen in the cord on T1W images. The apparent narrowing of the cord at C1 is related to a metal susceptibility artifact.

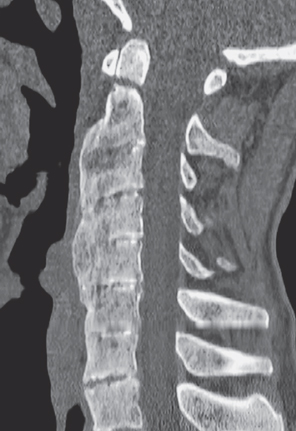
Fig. 10.4 Type II odontoid fracture in a 59-year-old man with AS who suffered a ground level fall. Sagittal reformatted CT of the cervical spine. A high transverse fracture of the odontoid process is seen with anterior ankylosis and disk narrowing of C2 through C7. Enthesopathic anterior vertebral ossification indicates a component of DISH. Bilateral ankylosis of the facet joints was demonstrated on other CT images.
Fractures of the cervical spine occurring in preexisting ankylosing spondylitis comprised 2% of a series of 1028 patients with cervical spine injuries.20
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree