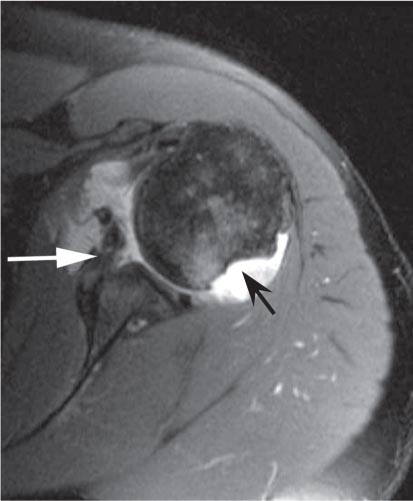
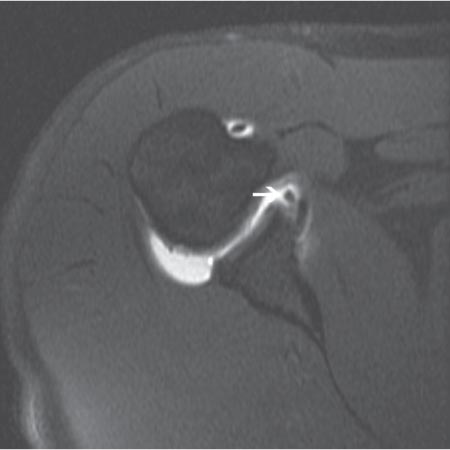
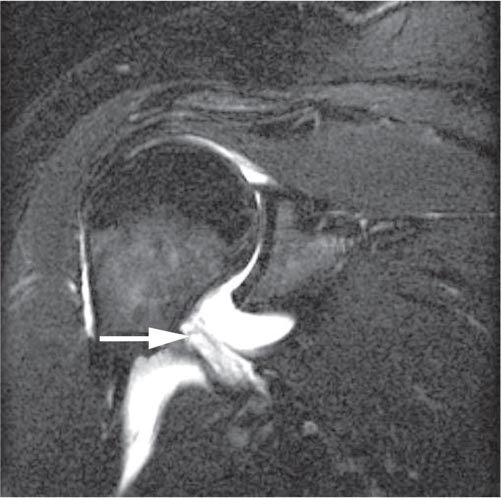
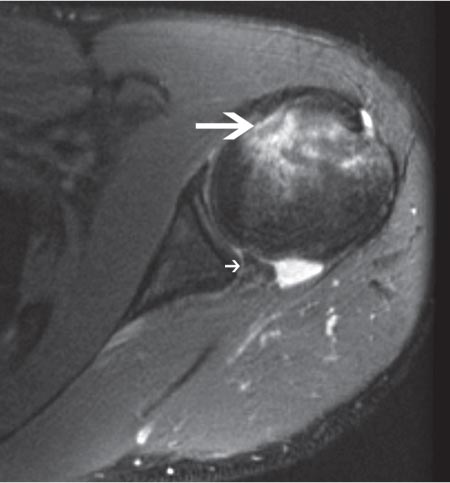
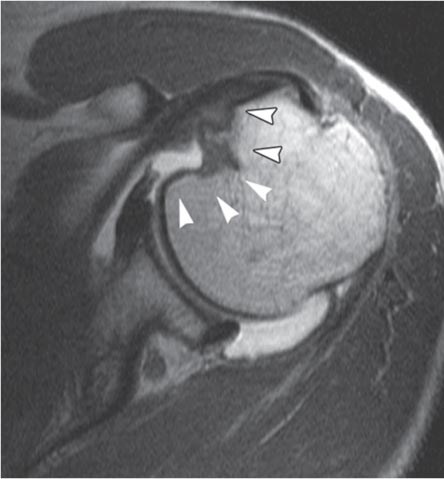
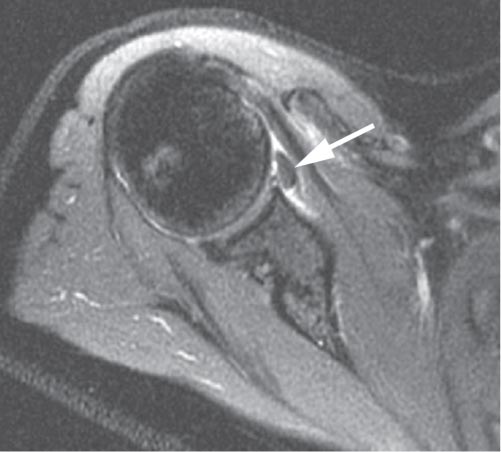
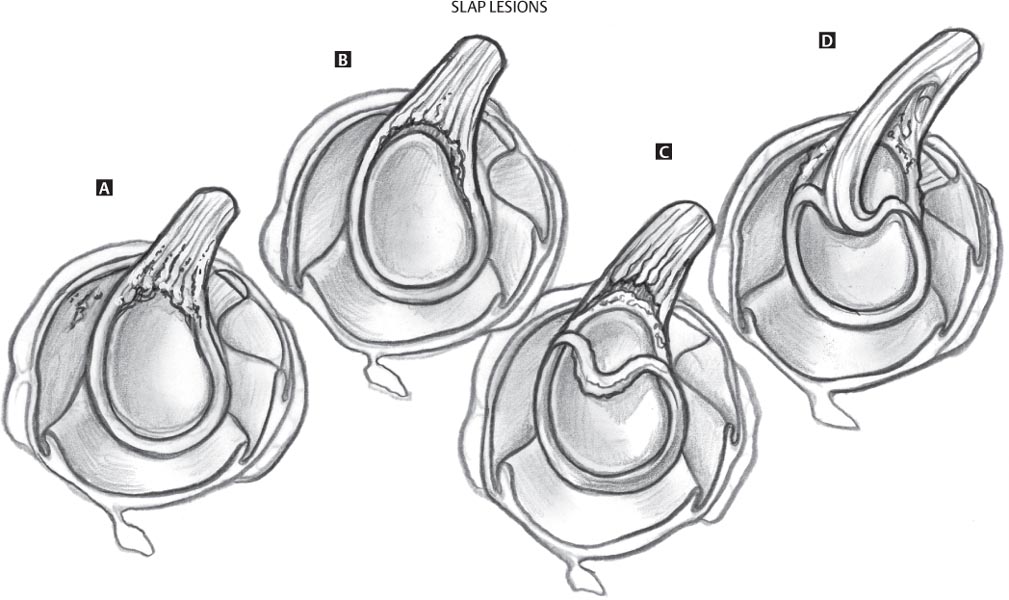
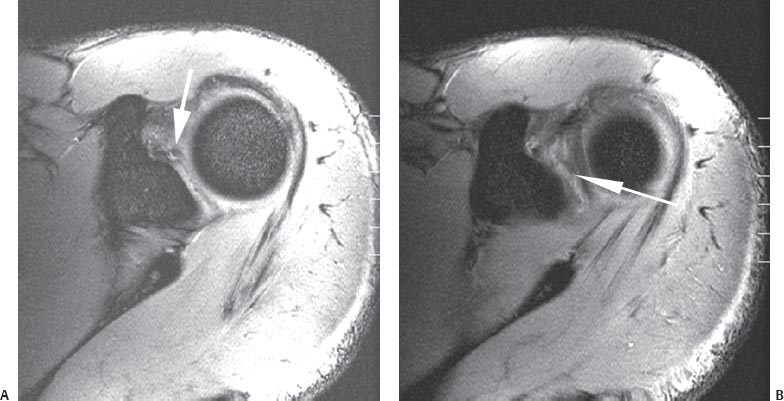
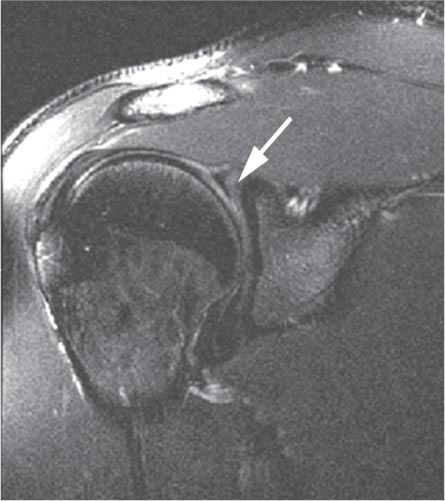
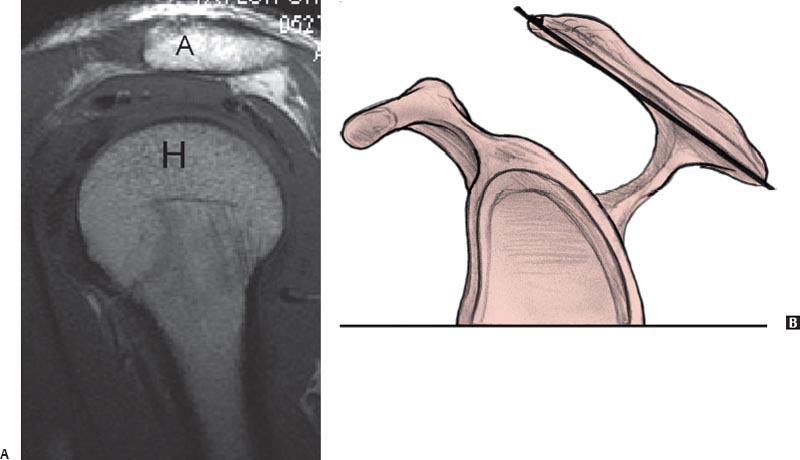
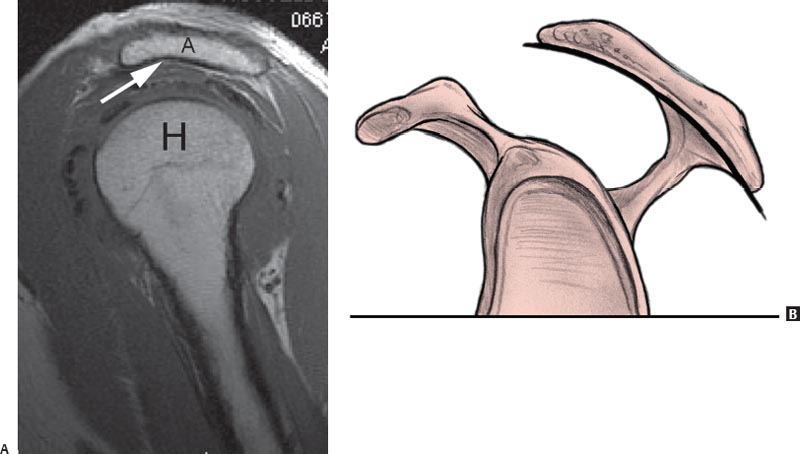
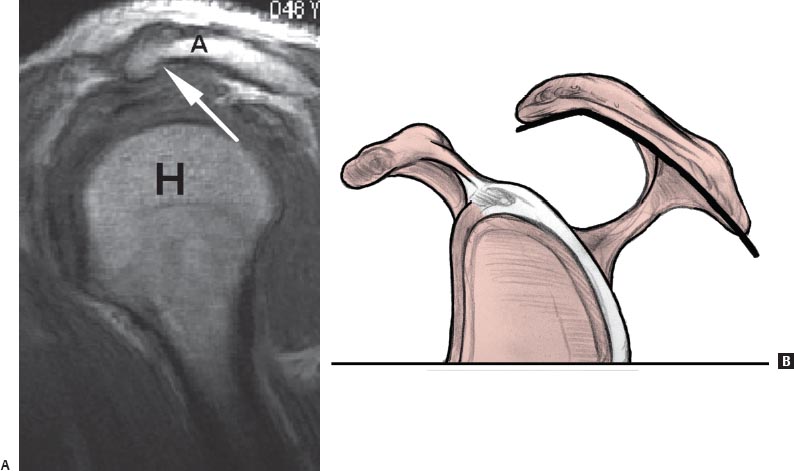
4 The Shoulder MRI of the shoulder has improved with the development of high-field systems and enhanced surface coil technology.1 The patient is imaged in the supine position and the arm is held at the side, rather than across the chest, to minimize transmission of respiratory motion to the shoulder. To optimally visualize the supraspinatus tendon and its insertion and to prevent confusing overlap with the infraspinatus tendon on coronal oblique images, the arm is placed in slight external rotation. Axial, coronal oblique, and sagittal oblique images are obtained routinely. Most centers use a standard screening examination, consisting of an array of specified imaging planes and pulse sequences.1 In addition to standard intermediate-weighted (proton-density) images, fat-suppressed proton-density, fat-suppressed T2-weighted, and STIR sequences are sensitive to the presence of fluid. The latter sequences allow the detection of soft-tissue pathology by accentuating the increased signal of edema relative to the surrounding structures. In some centers, non–fat-suppressed T2-weighted imaging is preferred for the evaluation of the rotator cuff tendons because it aids in the distinction of tendinosis and partial tears. In general, these sequences are acquired with an FSE technique that produces the desired contrast in a fraction of the time needed for conventional SE sequences. In addition, gradient-echo sequences may be used to evaluate the articular cartilage (see Chapter 14) and to delineate the presence of intraarticular bodies or accentuate calcification seen with calcium hydroxyapatite deposition. However, gradient-echo sequences should be avoided after shoulder surgery (especially in the presence of metal hardware) because of the increased artifact inherent to the gradient-echo technique (see Chapter 1). MR arthrography can be performed via direct or indirect methods. Direct MR arthrography is performed by injecting approximately 10 to 15 mL of diluted gadolinium contrast agent into the glenohumeral joint from an anterior or posterior approach and acquiring fat-suppressed T1-weighted and T2-weighted images. Indirect MR arthrography is performed by injecting gadolinium intravenously and imaging the joint after contrast has been taken up by the synovium and then diffused into the joint. Direct MR arthrography of the shoulder has been shown to improve visualization of the labrum, the articular cartilage, and the rotator cuff tendons. Indirect MR arthrography has limited use for evaluation of the labrum, but it aids in the detection of rotator cuff pathology and in the assessment of arthritis, neoplasm, and infection. However, with the advent of high-field, high-resolution imaging and novel noncontrast MR techniques, direct and indirect MR arthrography techniques may be rendered obsolete in the future.2 Traumatic conditions affecting the shoulder that are commonly evaluated by MRI include the following: • Glenohumeral instability • Labral pathology • Occult fractures • Rotator cuff tears Many rotator cuff tears occur in the setting of long-standing tendinosis (see Degenerative Conditions, below). Because of the shoulder’s extensive range of motion, it is the most commonly dislocated joint in the body.3,4 Instability encompasses a spectrum of disorders of varying direction, degree, and etiology. Shoulder instability is classified based on the direction of dislocation (i.e., anterior [most common], posterior, or multidirectional) and by degree (dislocation, subluxation, and microinstability), force (traumatic versus atraumatic), and patient contribution (voluntary versus involuntary). Instability episodes range from subluxation to complete dislocation and are associated with a spectrum of injury to the shoulder stabilizers. Patients with recurrent anterior shoulder instability typically have a history of a traumatic (direct or indirect) anterior shoulder dislocation, report recurrent episodes of subluxation or dislocation, and describe symptoms such as pain or apprehension during arm abduction and external rotation. Patients with recurrent posterior instability pose more complex diagnostic challenges and can present with traumatic posterior instability or with atraumatic subluxations not associated with trauma. Trauma, direct or indirect, also may be the mechanism of injury of a posterior shoulder instability or dislocation. Seizures and electrocution are common causes of posterior shoulder dislocation. Fig. 4.1 An axial fat-suppressed proton-density image of the left shoulder showing an osseous Bankart lesion (white arrow) and a Hill-Sachs lesion (black arrow). Although conventional radiographs often are sufficient for diagnosing shoulder dislocation, MRI is valuable in evaluating patients with presumed instability but no history of a dislocation, or to evaluate the status of the rotator cuff in patients preoperatively. The MRI findings of anterior instability vary depending on the degree of instability and the chronicity of instability. The most common pathologies associated with traumatic anterior shoulder instability are detachment of the anterior-inferior labrum (known as a Perthes-Bankart lesion) and tears of the anterior capsule.5 The Bankart lesion (Figs. 4.1 and 4.2) represents an avulsion of the anterior-inferior glenoid labrum from the glenoid rim (soft-tissue Bankart lesion). When this lesion is associated with an intact anterior scapular periosteum, it is called an anterior labrum periosteal sleeve avulsion lesion. There may be an associated fracture of the anterior inferior glenoid rim (osseous Bankart lesion)6 or a contusion of the posterior aspect of the humeral head (Hill-Sachs lesion).6 The MRI appearance of a Bankart lesion includes the following7: • A linear high signal intensity coursing through the normally homogeneously low signal intensity labral substance, • An abnormally small or absent anterior labrum, or • A displaced anterior glenoid labrum with the presence of fluid signal intensity between the anterior rim of the osseous glenoid and the displaced labrum. In addition, a low signal intensity fracture line surrounded by edema (intermediate T1-weighted signal intensity and high T2-weighted signal intensity) is seen in the presence of a fracture.8 These findings are best appreciated on the axial images (Figs. 4.1 and 4.2). As with most traumatic conditions, the pattern of MRI signal intensity often can be used to estimate the approximate age of a given injury. High signal intensity on T2-weighted or fat-suppressed T2-weighted images (along with low signal intensity on T1-weighted images) suggests the presence of an acute, or at least subacute, injury because it indicates the presence of edema at the site of injury. Conversely, the absence of increased signal intensity on T2-weighted or fat-suppressed T2-weighted images suggests the presence of a chronic injury with no substantial edema present. A finding known as the double axillary pouch sign is assessed with coronal oblique images and is very specific for anterior labral tears.9 A lesion known as the anterior labroligamentous periosteal sleeve avulsion injury is a variation of the Bankart lesion; unlike a Bankart lesion, the anterior labroligamentous periosteal sleeve avulsion lesion has an intact anterior scapular periosteum, allowing the labroligamentous structures to displace medially and to rotate inferiorly on the scapular neck.10 This lesion is visualized on axial MR images as medial displacement and inferior rotation of a torn anterior labrum (Fig. 4.3).10 Fig. 4.2 An axial fat-suppressed proton-density image of the right shoulder showing the labral tear of a Bankart lesion (arrow). Fig. 4.3 An axial fat-suppressed T2-weighted image of an anterior labroligamentous periosteal sleeve avulsion lesion in the right shoulder showing the medially displaced anterior labrum (arrow). Anterior shoulder dislocations may also produce a posterolateral impression fracture in the humeral head, known as a Hill-Sachs lesion.11 This lesion is seen on MRI as a flattening or concavity of the posterolateral humeral head detected on the two most superior axial images through the level of the humeral head; on those superior images, the humeral head is normally round above the bicipital groove and tuberosities (Fig. 4.4).12,13 Finally, an anterior shoulder dislocation may tear the IGHL without injuring the anterior labrum. This injury, known as a HAGHL, is defined as an avulsion of the IGHL from the anatomic neck of the humerus.14,15 On MRI, a HAGHL shows morphologic disruption of the normally low signal intensity IGHL on axial images.14 In addition, fluid signal intensity often is seen within the soft tissues anterior and inferior to the shoulder joint, which likely represents edema, hematoma, or extravasated joint fluid (Fig. 4.5).14 The HAGHL is frequently associated with tears of the subscapularis tendon.14 Posterior instability of the shoulder is much less common than anterior instability. MRI findings of posterior instability are analogous to the findings seen with anterior instability, but the word reverse is used to describe lesions that convey a posterior direction to the instability. Therefore, in a patient who has sustained posterior shoulder instability in which the humeral head has subluxated or dislocated posterior to the glenoid, a reverse Bankart lesion represents an avulsion of the posterior-inferior capsulolabral structures from the glenoid rim (Fig. 4.6); similarly, a reverse Hill-Sachs lesion represents edema or an impaction fracture of the anteromedial humeral head16 (Fig. 4.7). In addition to these findings, MRI typically reveals posterior capsular disruption, which is evident as a disruption or marked irregularity of the normally low signal intensity line representing the posterior capsule.16 Fig. 4.4 An axial fat-suppressed T1-weighted image showing a Hill-Sachs impression fracture (arrow) on the posterolateral aspect of the humeral head in a left shoulder. Fig. 4.5 A coronal fat-suppressed T2-weighted image of a HAGHL lesion in the right shoulder showing fluid signal passage through the anterior band of the IGHL (arrow). Fig. 4.6 An axial fat-suppressed proton-density image of a reverse soft-tissue Bankart lesion in the left shoulder showing an avulsion of the posterior-inferior labrum from the glenoid rim (small arrow) and a reverse Hill-Sachs impaction fracture on the anteromedial aspect of the humeral head (large arrow). Fig. 4.7 An axial intermediate weighted MR arthrographic image of the left shoulder showing a medium-sized reverse Hill-Sachs defect (arrowheads) involving 25% to 50% of the articular surface of the humeral head. Reprinted by permission from Saupe N, White LM, Bleakney R, et al.: Acute traumatic posterior shoulder dislocation: MR findings. Radiology 2008;248:185–193. Other MRI findings associated with episodes of shoulder instability include injuries to the rotator cuff, especially in patients more than 40 years old. Anterior dislocations are associated with tears of the supraspinatus and subscapularis, whereas posterior dislocations are associated with tears of the subscapularis or fractures of the lesser tuberosity. MRI has proved to be a sensitive, specific, and accurate modality for evaluating the glenoid labrum,7,17,18 which routinely is assessed in all three imaging planes.19 Coronal oblique and axial plane images, however, provide the most diagnostic information.20 The axial plane best shows the anterior and posterior labrum, whereas the coronal oblique plane visualizes the superior and inferior portions.21 The normal labrum is approximately 3 mm in craniocaudal dimension from base to apex and is 4 mm in width at its base of insertion into the glenoid cartilage.22 The classic morphology is described as smooth, with triangular anterior and posterior wedges, as seen on axial images.21 The intact fibrous labrum shows low signal intensity on all pulse sequences. The peripheral attachment of the labrum joins the capsule and glenohumeral ligaments, creating the capsulolabral complex. This capsulolabral or labral ligamentous complex is best appreciated on sagittal oblique MR images. The sagittal oblique plane also is useful for evaluating displaced bucket-handle tears of the labrum.22 Labral tears and SLAP lesions (superior labrum from anterior to posterior, relative to the biceps tendon anchor) are best appreciated on fluid-sensitive sequences.17 There is considerable variation in the attachment and morphology of the glenoid labrum. Labral anatomy anteriorly and posteriorly is best evaluated with axial images. Above the equator of the glenoid, the labrum may not be attached to the glenoid, but inferior to the middle of the glenoid, the labrum often is confluent with the articular cartilage. The greatest variation in labrum anatomy occurs in the anterosuperior glenoid.23 To detect true abnormalities, knowledge of these normal variants of labral anatomy as visualized on MRI is very important. Specifically, the absence of a labral attachment in the anterosuperior quadrant is a normal variant and should be differentiated from pathologic labral tears. Therefore, one must be cautious about interpreting an isolated labral tear in the anterosuperior quadrant. A normal sublabral foramen, or hole, between the labrum and the glenoid rim is often misinterpreted as an anterior labral disruption or tear. When present, the sublabral foramen is located in the 1 o’clock to 3 o’clock positions, anterior to the biceps-labral complex, and represents space between the anterosuperior labrum and the adjacent glenoid cartilage.22 A sublabral foramen can vary in size from a few millimeters to the entire anterosuperior quadrant above the level of the subscapularis tendon.24 Another normal anatomic variant, known as the Buford complex (Fig. 4.8), consists of three elements25: • An MGHL that attaches directly to the superior labrum anterior to the biceps (at the base of the biceps anchor) • The absence of anterosuperior labral tissue The sagittal oblique plane shows the course of the cord-like MGHL attaching directly to the superior labrum at the anterior base of the biceps tendon. The sublabral recess, or sublabral sulcus, is an additional anatomic variant that should be recognized. In this variant, the superior labrum (from the 11 o’clock to 1 o’clock positions) is meniscoid in morphology.22,26 On coronal oblique views, a recess appears as an area of high signal intensity on T2-weighted images between the labrum and the superior glenoid. The recess curves medially and follows the contour between the superior labrum and adjacent hyaline cartilage of the superior glenoid.22,26 The caudal meniscoid portion of the labrum is not attached to the superior portion of the glenoid, but the base of the superior labrum remains attached near the insertion of the long head of the biceps tendon.22,26 In 1990, Snyder and associates27 were the first to describe SLAP lesions. Patients with SLAP lesions usually present with complaints of deep pain (typically with overhead activities) and/or mechanical symptoms of catching, locking, popping, or grinding.28 Frequently, there is a history of overhead activities or sports. The mechanism of injury often is traction or compression.28 Fig. 4.8 An axial fat-suppressed proton-density image of the right shoulder showing the Buford complex, which consists of three elements: a cord-like MGHL (arrow), an MGHL that attaches directly to the superior labrum anterior to the biceps (at the base of the biceps anchor), and an absence of anterosuperior labral tissue. Fig. 4.9 Types of SLAP lesions. (A) Type I, a frayed and degenerative superior labrum with a normal (stable) biceps tendon anchor. (B) Type II, detachment of the superior labrum and biceps anchor. (C) Type III, a bucket-handle tear of a meniscoid superior labrum without extension into the biceps tendon. The biceps anchor is stable and the remaining labrum is intact. (D) Type IV, a bucket-handle tear of a meniscoid superior labrum with extension into the biceps tendon. (Based on Powell SE, Nord KD, Ryu RKN: The diagnosis, classification, and treatment of SLAP lesions. Oper Tech Sports Med 2004;12:99–110.) Fig. 4.10 Type II SLAP lesion. (A,B) Axial fat-suppressed gradient-echo images of the left shoulder showing increased signal intensity within the superior glenoid labrum (arrow) in a patient with a type II SLAP lesion verified by arthroscopy. The most common classification of SLAP tears includes four distinct lesions, although recently new lesions and subclassifications have been added (Fig. 4.9).27,29 In type I lesions, there is a frayed and degenerative superior labrum with a normal (stable) biceps tendon anchor. On MRI, the labral contour appears blunted or irregular with a slight increase in signal intensity on T2-weighted images.30,31 Type II lesions have similar labral fraying but have detachment of the superior labrum and biceps anchor, making them unstable. MRI findings of type II SLAP lesions include a line of high-intensity signal coursing across the base of the hyperintense labrum to the periphery (Figs. 4.10 and 4.11). The long head of the biceps tendon has normal signal and shape and is attached to the avulsed labrum.31 The sublabral recess can be differentiated from a type II SLAP lesion by two MRI signs on T2-weighted images present in these SLAP lesions, but not in sublabral recesses26: • High signal intensity in the labrum posterior to the biceps anchor, which extends to the articular surface • An area of high signal intensity irregular or curved laterally and distinct from the medial curvilinear area of signal intensity at the labral–glenoid junction seen in a sublabral recess In type III lesions, there is a bucket-handle tear of a meniscoid superior labrum without extension into the biceps tendon. The biceps anchor is stable and the remaining labrum is intact. On MRI, type III SLAP lesions are characterized by a line of high signal intensity coursing across the base of the hyperintense labrum but extending beyond the equator in the case of a nondisplaced bucket-handle tear. In the case of a displaced bucket-handle tear, a discrete piece of fibrocartilage is identified within the joint capsule. On MRI, the displaced piece of fibrocartilage appears as a low signal intensity intraarticular fragment surrounded by high signal intensity joint fluid.32 In type III SLAP lesions, the superior labrum also is deficient, yet the biceps tendon can be followed to the supraglenoid tubercle.31 Fig. 4.11 A coronal oblique fat-suppressed T2-weighted image of the right shoulder showing increased signal intensity within the superior glenoid labrum (arrow) posterior to the long head of the biceps tendon origin in a patient with a type II SLAP lesion verified by arthroscopy. Fig. 4.12 An axial fat-suppressed proton-density image of a type IV SLAP lesion in the right shoulder showing increased signal intensity within the superior glenoid labrum with extension into the biceps anchor (arrow). In type IV SLAP lesions, there is a bucket-handle tear of a meniscoid superior labrum with extension into the biceps tendon. On MRI, a type IV SLAP lesion is characterized by a line of high signal intensity coursing across the base of the normally hypointense labrum to the periphery and extending beyond the equator with a deficient labrum (Fig. 4.12).30 In addition, there is hyperintensity and splitting of fibers of the biceps tendon.31 SLAP lesions frequently are associated with other shoulder pathology that can be visualized on MRI. The presence of paralabral cysts, almost invariably associated with labral tears,21,33,34 should incite the search for a labral tear. The imaging features include a cystic-appearing mass adjacent to the labrum or capsule with increased signal on T2-weighted sequences.21 Rotator cuff tears (both partial thickness and full thickness) and Bankart lesions are commonly associated with SLAP lesions.35,36 The shoulder is affected by numerous degenerative conditions, including the following: • Subacromial impingement syndrome • Rotator cuff tears • Glenohumeral osteoarthritis • AC osteoarthritis • Pathologic conditions affecting the biceps tendon Subacromial impingement syndrome is a continuum of abnormalities and clinical symptoms; in its final stages, it may be associated with full-thickness rotator cuff tears. Impingement syndrome is secondary to compression of the rotator cuff by abnormal morphology of structures within the supraspinatus outlet. Patients with chronic impingement syndrome typically present with the insidious onset of diffuse shoulder pain in the area of the deltoid muscle; the pain is activity related, worse with overhead activities, and often worse at night.37 However, it must be stated that there is often no correlation between clinical symptoms and rotator cuff pathology found on MRI or during autopsy. Osseous factors that contribute to subacromial impingement syndrome include the following38,39: • Anterior acromial spurs • The shape of the acromion • The slope of the acromion • The morphology of the AC joint (e.g., hypertrophic bone, calcification of the coracoacromial ligament, callus formation) The shape of the acromion (acromial morphology) is best evaluated with sagittal oblique MR images. Bigliani and associates38 classified acromial morphology into three types: • Type I, a flat undersurface (Fig. 4.13) • Type II, a smooth curved inferior surface (Fig. 4.14) • Type III, an anteroinferior hook or beak (Fig. 4.15) The type II and type III acromions that create narrowing of the supraspinatus outlet are associated with a predisposition to rotator cuff disease.40,41 In addition to acromial morphology in the sagittal plane, the slope of the acromion in the coronal plane may predispose patients to impingement syndrome and subsequent rotator cuff tears. Normally, the anterior acromion should be nearly horizontal when viewed in the oblique coronal plane. Lateral downsloping of the acromion narrows the supraspinatus outlet and may predispose to impingement syndrome.42 Sagittal oblique MR images can be used to assess the morphology of the acromion from posterior to anterior, whereas coronal oblique MR images can be used to evaluate the lateral acromial slope. Fig. 4.13 Type I acromion. (A) A sagittal oblique T1-weighted image. A, acromion; H, humeral head. (B) Artist’s sketch. Straight line indicates flat inferior surface. Fig. 4.14 Type II acromion. (A) A sagittal oblique T1-weighted image (arrow, curved inferior surface). A, acromion; H, humeral head. (B) Artist’s sketch. Curved line indicates curved inferior surface. Fig. 4.15 Type III acromion. (A) A sagittal oblique T1-weighted image (arrow, anterolateral hook or beak). A, acromion; H, humeral head. (B) Artist’s sketch. Bent line indicates an anteroinferior hook or beak. The spectrum of MRI changes in subacromial impingement syndrome have been characterized and documented.43,44 Rotator cuff disease is evaluated on the basis of tendon morphology and changes in the observed signal intensity within the specific cuff tendons. In addition, pathologic processes within the supraspinatus outlet, including abnormalities of the acromion, AC joint, and the subacromial-subdeltoid bursa, may be identified in the spectrum of findings in patients with impingement symptoms. Changes in the subacromial bursa often are seen on MRI in association with impingement syndrome.45,46
 Specialized Pulse Sequences and Imaging Protocols
Specialized Pulse Sequences and Imaging Protocols
 Traumatic Conditions
Traumatic Conditions
Glenohumeral Instability
Labral Pathology and SLAP Lesions
 Degenerative Conditions
Degenerative Conditions
Subacromial Impingement Syndrome
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree