7 The upper limb
The bones of the upper limb
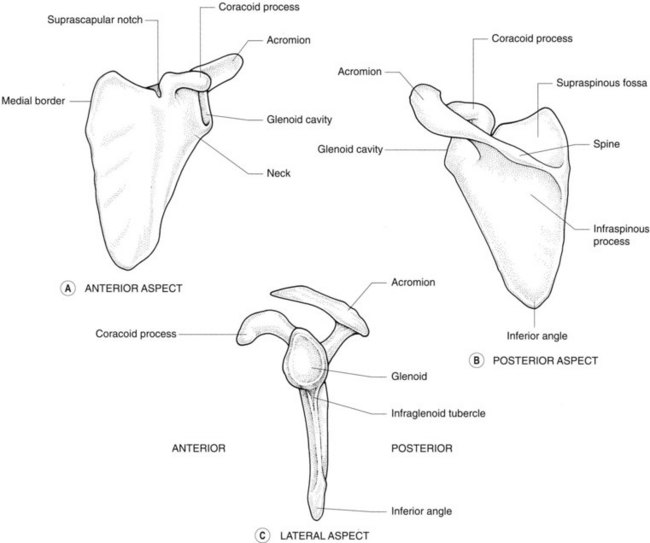
The scapula (Figs 7.1, 7.2)
This flat triangular bone has three processes:
Radiological features of the scapula
Isotope bone scan
The inferior angle of the scapula overlying the seventh rib may appear as a ‘hot spot’.
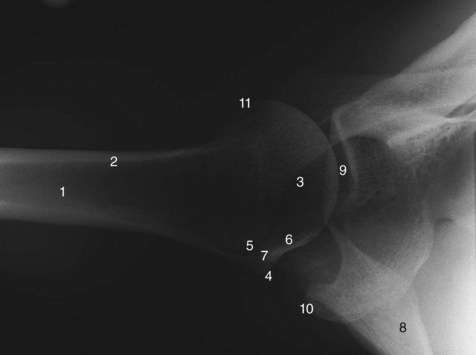
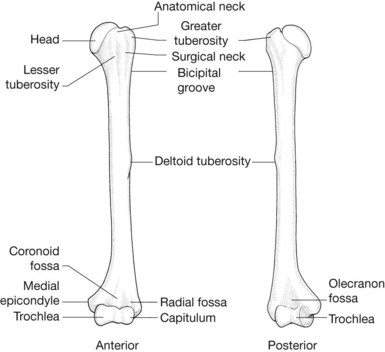
Radiological features of the humerus
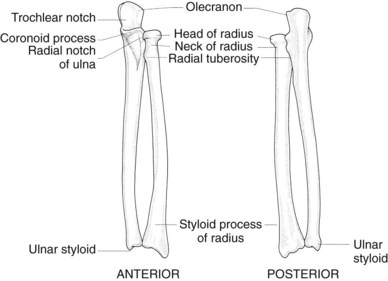
The radius and ulna (Figs 7.6, 7.7; see also Fig. 7.5)
Radiological features of the radius and ulna
Plain radiographs
The head of the radius has a single cortical line on its upper surface and is perpendicular to the neck in the normal radiograph (see Fig. 7.5). Angulation of the head or a double cortical line are signs of fracture of the radial head.
The ulnar styloid is proximal to the radial styloid, with a line joining them on an AP radiograph lying at an angle of 110° with the long axis of the radius (see Fig. 7.7). In a lateral radiograph, the articulating surface of the distal radius is angled 10° to a line through the shaft of the radius. Recognition of these normal angles is important in reduction of fractures of the wrist.
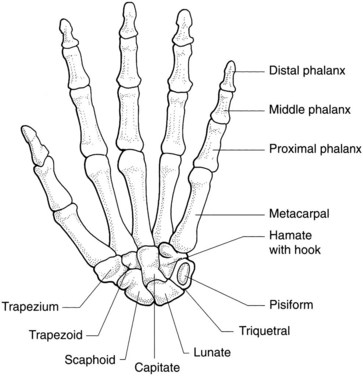
The carpal bones (Fig. 7.8; see also Fig. 7.7)
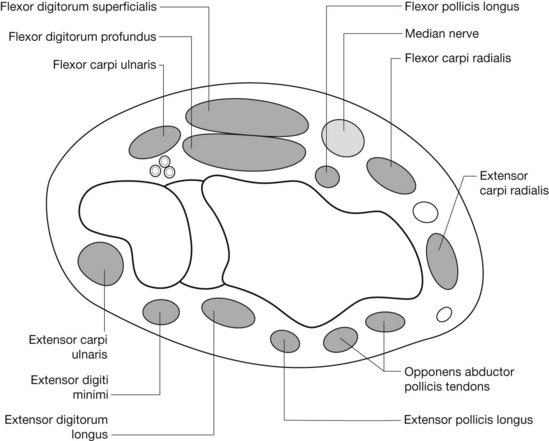
Together the carpal bones form an arch, with its concavity situated anteriorly. The flexor retinaculum is attached laterally to the scaphoid and the ridge of the trapezium, and medially to the pisiform and the hook of the hamate. It converts the arch of bones into a tunnel, the carpal tunnel, which conveys the superficial and deep flexor tendons of the fingers and the thumb (except flexor carpi ulnaris and palmaris longus tendons) and the median nerve. The extensor retinaculum on the dorsum of the wrist attaches to the pisiform and triquetrum medially and the radius laterally. Six separate synovial sheaths run beneath it (Fig. 7.9).
Radiological features of the carpal bones
Radiography
These are radiographed in the anteroposterior, lateral and oblique positions (see Fig. 7.7). Carpal tunnel views are obtained by extending the wrist and taking an inferosuperior view that is centred over the anterior part of the wrist.
The joints of the upper limb
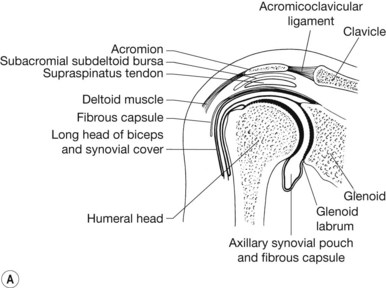
The shoulder (glenohumeral) joint (Fig. 7.11)
Articular surfaces
The articular surface of the humeral head is four times the area of the glenoid cavity.
Ligaments
Stability
The inferior part of the joint is least well protected by either ligaments or muscles.
Radiological features of the shoulder joint
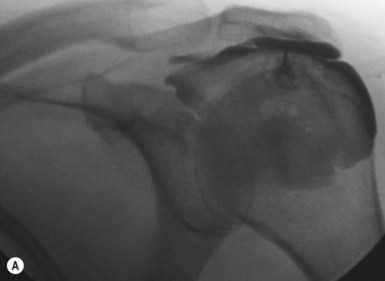
Subacromial bursography
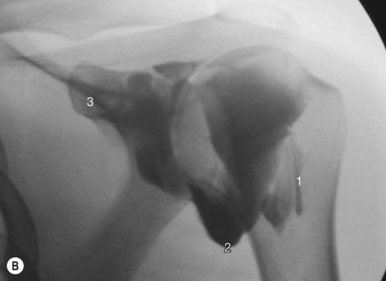
Contrast injection to the subacromial bursa with either ultrasound or fluoroscopic guidance is often followed by therapeutic injection of steroid and bupivacaine (Marcain). Subacromial bursitis or inflammation of the bursa is most frequently secondary to impingement (Fig. 7.10A, B).
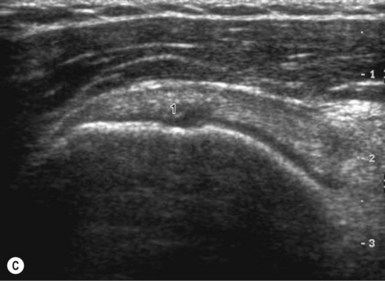
Ultrasound
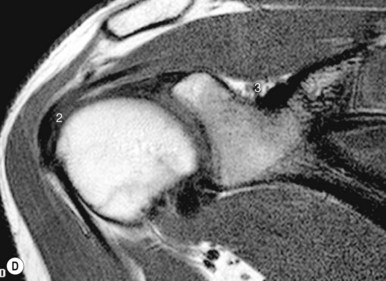
High-frequency linear probes are now often employed as an alternative to MRI to evaluate the rotator cuff (Fig. 7.10C, D).
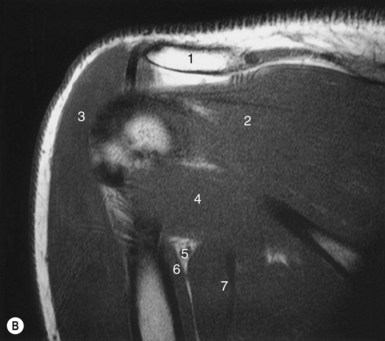
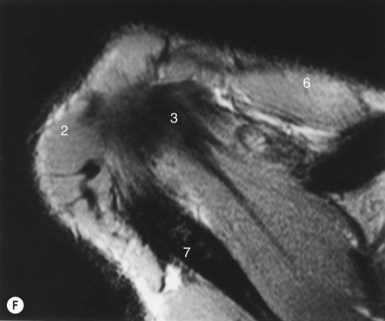
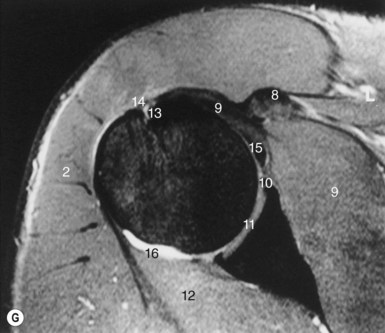
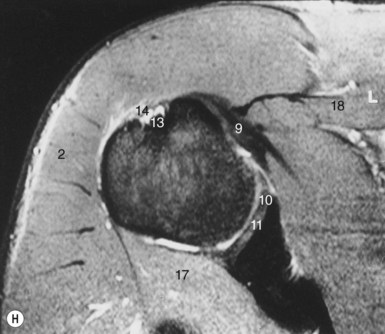
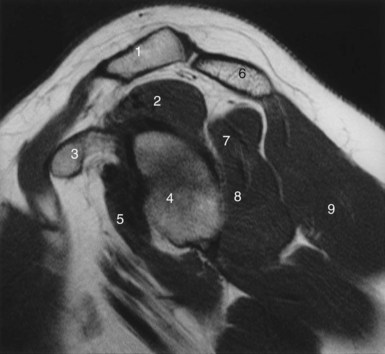
Magnetic resonance imaging (Figs 7.11, 7.12)
MRI with surface coils is used increasingly to image the shoulder joint.