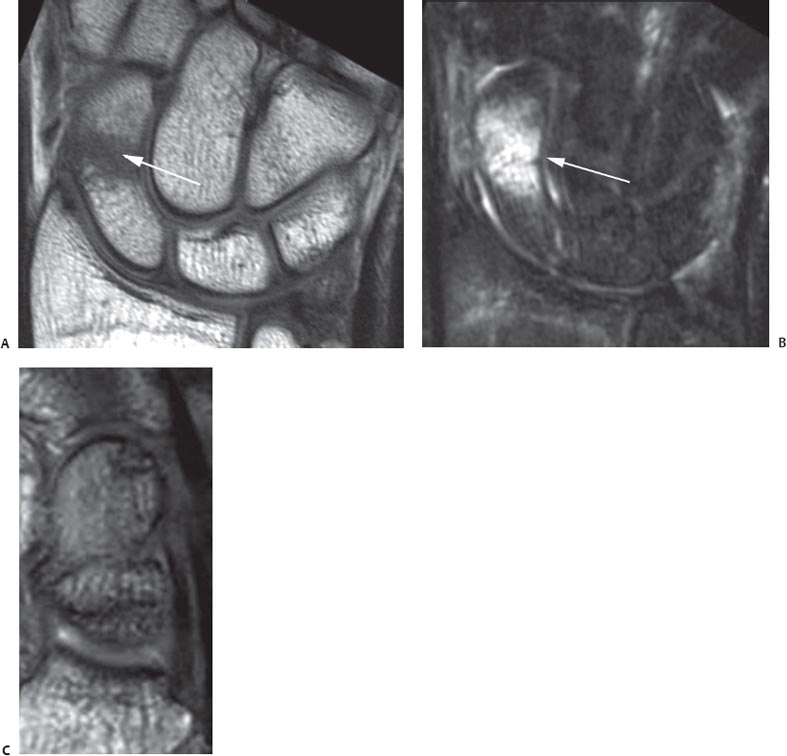
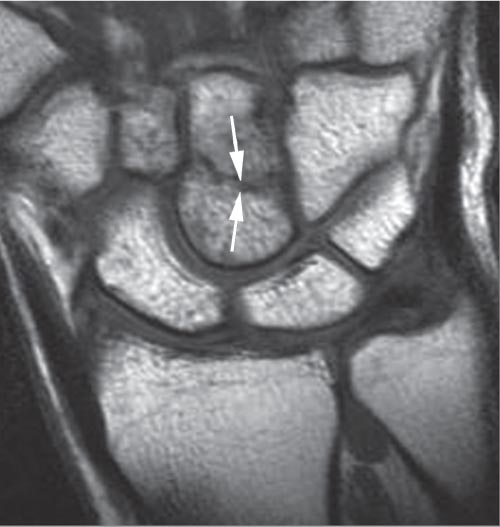
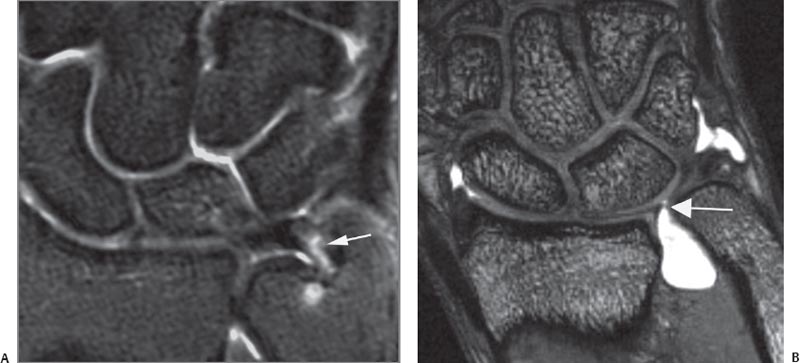
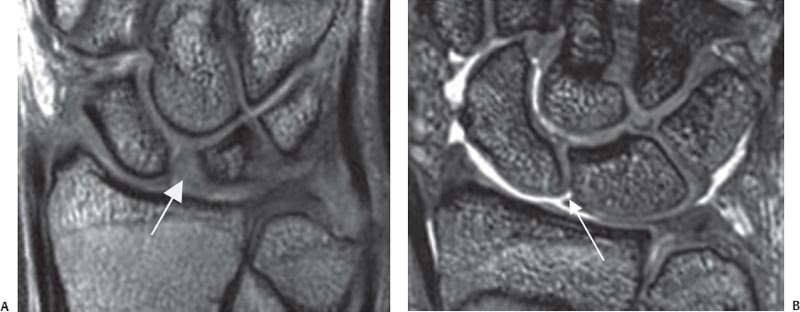
6 The Wrist and Hand The routine use of MRI for the distal upper extremity, compared with its use for larger joints, has been hindered by the technical challenges of imaging small anatomic structures. MRI of the wrist and hand typically is performed at a magnetic field strength of 0.2 to 3.0 T, using systems with dedicated surface coils. Recent advances in high field strength magnets and extremity surface coil design, however, have resulted in additional improvement in image quality. One prospective study revealed significantly higher contrast-to-noise ratios between muscle and bone and between bone and cartilage for all sequences with a 3-T system than with a 1.5-T system.1 3-T systems are now becoming available for clinical use, but most hand and wrist examinations are still performed with 1.5-T magnets. The hand or wrist is best imaged with the patient prone and the affected extremity placed above the head with the forearm pronated. Typically, the closer the body part being imaged is to the isocenter of the magnet, the better the image quality that is obtained. Because this position is uncomfortable for many patients, scanning may also be performed with the patient supine, the arm positioned at the patient’s side, and the forearm in neutral, with the attendant risk of some degradation of image quality. A small field of view and 1- to 3-mm-thick sections are preferable. Scanning is routinely performed in the axial, coronal, and sagittal planes. Most centers use a standard screening examination, consisting of an array of specified imaging planes and their corresponding pulse sequences. Based on the indication, additional pulse sequences may be added. Standard pulse sequences include the following: • T1-weighted • T2-weighted FSE with fat suppression • STIR • Gradient-echo T1-weighted images provide good anatomic detail and are especially useful for identifying fat (given its high signal intensity on these images) in lipomatous masses or atrophied muscles. Fat- suppressed, T2-weighted sequences are the most sensitive for detecting many pathologic conditions by accentuating the presence of abnormal fluid, edema, or hemorrhage related to traumatic injury or an inflammatory process. Gradient-echo sequences, especially with a 3D, thin-section technique, are useful for evaluating the carpal ligaments and articular cartilage (see Chapter 14). MR arthrography of the wrist can be performed with single-, double-, or triple-compartment (radiocarpal, intercarpal, or distal radioulnar compartments) injection of contrast material. Approximately 2 to 5 mL of contrast are administered under sterile technique and fluoroscopic guidance. A single-compartment radiocarpal technique is used most often, with normal dissemination of contrast material between the proximal carpal row and the distal radius. Fat-suppressed, T1-weighted images are typically obtained in all three planes, in addition to other sequences. MR arthrography of the wrist has proven useful in the evaluation of the scapholunate ligament, the lunotriquetral ligament, and the TFCC.2 Intravenous contrast provides valuable information for the evaluation of a soft-tissue mass or possible synovial process involving the wrist and hand, especially when combined with fat-suppressed T1-weighted images. It is useful for differentiating solid and cystic lesions, showing rim-enhancing soft-tissue abscesses, and determining bone vascularity in cases of suspected osteonecrosis. Intravenous contrast may also be used to perform indirect arthrography, in which the contrast may migrate into the joint over time. This effect is most notable in an inflamed joint. The potential information gained from these procedures must always be weighed against the additional cost and risk associated with an invasive procedure. Traumatic conditions affecting the wrist and hand that are commonly evaluated by MRI include occult fractures, tears of the TFCC, and injuries to the interosseous carpal ligaments and small joint ligaments and tendons. At initial presentation, a patient with wrist pain after a traumatic injury to the outstretched hand may not have radiographic evidence of a fractured scaphoid. However, when a patient continues to have tenderness in the anatomic snuffbox or over the scaphoid tubercle at follow-up examination, other advanced imaging modalities often are used for the detection of a radiographically occult scaphoid fracture. Recent comparative studies have sought to determine the superior modality for confirming the diagnosis: bone scintigraphy, CT, MRI, or ultrasound.3–6 MRI has consistently outperformed other methods in the accurate early detection of scaphoid fracture and other radiographically indeterminate carpal injuries.7–9 In addition, the use of early MRI in the management of clinically suspected scaphoid fractures may prove to be more cost-effective than follow-up conventional radiography.10,11 A fracture may be identified on T1-weighted images as a distinct line of low signal intensity that contrasts with the surrounding high-signal marrow (Fig. 6.1A). Fat-suppressed, T2-weighted images typically show high-signal marrow edema surrounding the fracture line (Fig. 6.1B). A scaphoid humpback deformity may also be shown on sagittal images (Fig. 6.1C). MRI has proven to be sensitive in the detection of occult fractures in the distal radius, distal ulna, and other carpal bones (Fig. 6.2)12,13 and can also differentiate fractures from bone bruises (contusions), which show marrow edema without a discrete fracture line. MRI is also sensitive for diagnosing subtle physeal injuries in children (Fig. 6.3) and for evaluating physeal bars and growth arrest.14 Radiographically occult fractures of the metacarpals and phalanges are uncommon. Fig. 6.1 Scaphoid fracture/deformity. (A) A coronal T1-weighted image of the wrist showing a fracture through the scaphoid waist (arrow), seen as a discrete line of low signal intensity. (B) A coronal fat-suppressed T2-weighted image showing the same fracture as in (A), with focal marrow edema in the scaphoid waist consistent with fracture (arrow). (C) A sagittal gradient-echo image showing a humpback deformity of the scaphoid. Fig. 6.2 A coronal T1-weighted image of the wrist showing a radio-graphically occult capitate fracture (arrows). The TFCC encompasses the major stabilizing structures of the ulnar aspect of the wrist, spanning the distal radioulnar joint and consisting of the following components15: • Fibrocartilaginous articular disc • Dorsal and volar radioulnar ligaments • Ulnolunate ligament • Ulnotriquetral ligament • UCL • ECU subsheath • A variable meniscus homologue In general, tears of the TFCC are classified as degenerative or traumatic.16 Degenerative central perforations of the TFCC are common and often asymptomatic. On the other hand, acute injuries to the TFCC frequently lead to ulnar-side wrist pain and dysfunction. It is difficult to distinguish this condition from other causes of ulnar-side wrist pain (such as occult fractures, lunotriquetral ligament injury, ECU tendinopathy or subluxation, distal radioulnar joint injury, or pisotriquetral joint injury) by history and physical examination. Historically, three-compartment wrist arthrography was the imaging test of choice for evaluation of the TFCC. However, this modality suffers from unacceptably low sensitivity and specificity and lacks the ability to determine lesion size, location, and acuity.17,18 Although wrist arthros-copy remains the standard for the diagnosis of TFCC pathology, advances in MRI and MR arthrography are increasing the reliability in accurate diagnosis of the size, location, and character of TFCC tears before wrist arthroscopy. In the most specialized centers, the sensitivity and accuracy of MRI for detecting TFCC tears approaches 100%, using arthroscopy as the standard diagnostic modality.19 The normal TFCC is a low signal intensity structure shaped like a bowtie in the coronal plane. The articular disc is readily apparent on coronal and sagittal images. Advances in imaging techniques have enabled MRI to visualize some other individual components of the TFCC, such as the radioulnar ligaments and the ECU subsheath. T2-weighted images may help to differentiate between degenerative and traumatic tears of the TFCC, with traumatic tears showing increased signal intensity in adjacent tissues. The excellent anatomic detail afforded by MRI also helps in determining specific lesion location, with degenerative tears typically occurring in the thinner central portion and traumatic tears most often found in the periphery of the TFCC (Fig. 6.4). Nonetheless, all TFCC attachments must be carefully evaluated in all three planes. Ulnar attachment tears have been consistently more difficult to diagnose.20 Concomitant pathology of the ECU tendon, lunotriquetral ligament, and surrounding osseous structures must be pursued. MR arthrography may prove superior to MRI in detecting TFCC lesions.2,21 A TFCC tear is often shown by the presence of gadolinium contrast within the tear itself and/or in the distal radioulnar joint. Strong evidence exists that observer experience is critical for the accurate detection of TFCC pathology.22 Fig. 6.3 A sagittal STIR image of the wrist showing diffuse marrow edema in the distal radius metaphysis adjacent to the growth plate, which is widened along its volar aspect (arrow). Fig. 6.4 Peripheral TFCC tear. (A) A coronal fat-suppressed T2-weighted image showing a tear of the peripheral portion of the TFCC near its ulnar attachment (arrow). (B) A coronal STIR image showing a perforation of the peripheral portion of the TFCC near its radial attachment (arrow). The scapholunate and lunotriquetral ligaments are the most commonly injured wrist ligaments secondary to acute trauma. These C-shaped ligaments vary in thickness throughout their courses. MRI has supplanted stress radiography and conventional wrist arthrography as the study of choice for suspected carpal ligament injury. Compared with arthroscopic findings, conventional MRI is highly specific but still has an overall low sensitivity for the detection of tears of the scapholunate ligament,23 although the sensitivity seems to be improving with technologic advances in imaging techniques. Disruption of the interosseous ligaments is best evaluated on coronal gradient-echo (Fig. 6.5) and fat-suppressed T2-weighted images. Carpal ligaments show low signal intensity on most MR images. However, the scapholunate ligament normally shows a more heterogeneous appearance on coronal images, which may lead to the misdiagnosis of a tear. Distinct linear areas of high signal intensity equal to that of fluid, especially in the thick dorsal portion of the ligament, usually indicate clinically significant tears, which may lead to carpal instability if not treated adequately. Alternative findings in ligament tears include nonvisualization of the ligament or morphologic distortion.24 MR arthrography may be more accurate than conventional MRI for the detection of tears of the scapholunate ligament when compared with arthroscopic findings.25 MR arthrography is most useful for the detection of tears of the lunotriquetral ligament, which although rarely an isolated injury, often accompanies an injury to the TFCC. The assessment of lunotriquetral ligament pathology by MRI techniques is still met with skepticism in the literature.26,27 The extrinsic carpal ligaments are a complex assortment of dorsal and volar structures that lie in close relation to the wrist joint capsule. The volar extrinsic ligaments are stronger and more robust than their dorsal counterparts. Isolated acute injuries to the extrinsic ligaments are rare. Typically, disruptions of these ligaments are part of a constellation of acute bone and soft-tissue injury about the wrist joint. Although MRI can distinguish the extrinsic ligament complexes with multiple image planes or 3D reconstructions (Fig. 6.6), the role of MRI in this clinical setting is more often to exclude occult fracture, disruption of the intrinsic carpal ligaments, or injury to the TFCC. If diagnosed, these conditions may require a change in treatment algorithm. Fig. 6.5 Scapholunate ligament tear. (A) A coronal gradient-echo image of the wrist showing partial stretching of the scapholunate ligament with concurrent widening of the scapholunate interval (arrow). (B) A coronal gradient-echo image of the wrist showing a small perforation in the membranous portion of the scapholunate ligament (arrow). The UCL of the MCP joint is the primary stabilizer of the ulnar aspect of the thumb. Rupture of this ligament is common in skiers and results from forced abduction of the thumb. A Stener lesion describes displacement of the torn ligament to a position superficial to the aponeurosis of the adductor pollicis muscle, a conformation that inhibits adequate ligament healing. Although clinical presentation and stress radiography may be enough for the diagnosis of a torn UCL, MRI may detect a Stener lesion and help guide the surgical treatment of acute injuries (Fig. 6.7).28,29 Tendon pathology may occur as a result of acute trauma, chronic overuse, or inflammatory arthropathies such as RA. The spectrum of pathology ranges from tendon thickening and various degrees of tendon or tendon sheath inflammation to frank tears. In patients with traumatic injury, partial or complete rupture of a hand or wrist tendon may be difficult to diagnose clinically. Although tenderness and localized swelling are often present, the degree of flexion or extension loss may be equivocal. The use of MRI and ultrasound in this setting is evolving. Occasionally, ruptures of the extensor wrist tendons can be detected by MRI (Fig. 6.8). On T2-weighted sequences, partial tendon tears typically show increased intrasubstance signal intensity (Fig. 6.9), whereas complete tears show separation of the tendon ends with fluid tracking between its margins. Timely and accurate diagnosis has important clinical implications because early surgical repair provides the best outcome for zone II flexor tendon tears comprising >50% of their width.30
 Six Specialized Pulse Sequences and Imaging Protocols
Six Specialized Pulse Sequences and Imaging Protocols
 Traumatic Conditions
Traumatic Conditions
Occult Fractures of the Scaphoid and Other Bones
TFCC Injury
Interosseous Ligament Injury
Extrinsic Carpal Ligament Injury
Thumb UCL Injury
Tendon Injuries
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree