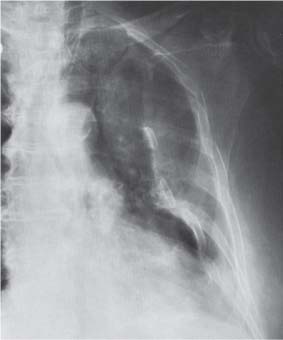
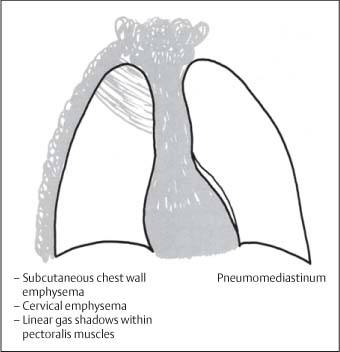
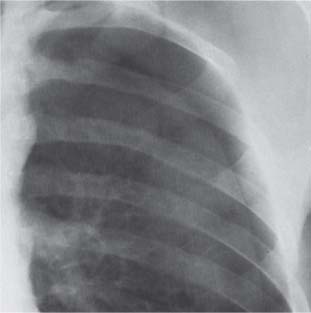
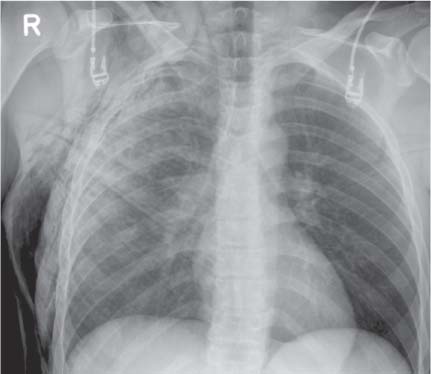
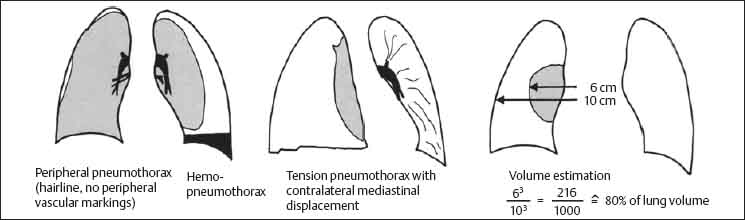
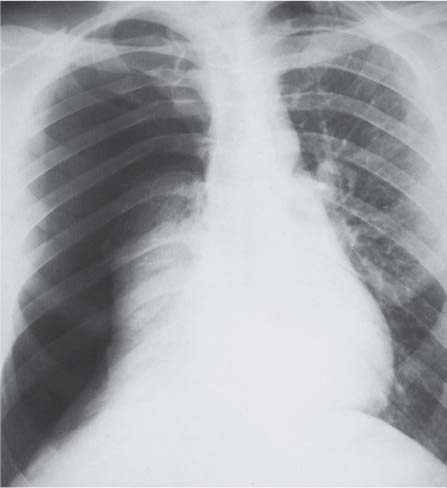
8 Thoracic Trauma In this, the age of motorized transport, road traffic accidents (RTAs) frequently result in nonpenetrating chest injury. In Northern Europe, penetrating injuries from gunshot and stab wounds are less common. Thoracic injuries are important as they account for up to 50% of trauma deaths (Wiot 1975). Imaging is initially with chest radiographs proceeding in many cases to computed tomography (CT) and less commonly to aortography. Multiple injuries are frequent but the following anatomic classification is helpful: Isolated rib fractures occur at sites of limited impact. Wide impact injuries deform the chest wall over a large area and result in multiple rib fractures which most commonly occur posteriorly adjacent to the costotransverse articulations. There may be accompanying fractures through the lateral ribs (Fig. 8.1) and costal cartilages. When a large segment of the chest wall loses continuity with the remainder of the bony thorax, there are paradoxical respiratory excursions that may cause life-threatening ventilatory impairment (flail chest, Fig. 8.2). Fig. 8.1 Rib fractures. Minor adjacent pleural thickening may be due to a small hematoma. Fractures through the 1st and 2nd or 11th and 12th ribs are unusual but they are frequently complicated by vascular (aortic, subclavian artery) and visceral (liver, spleen, kidneys) injury, respectively. Arch aortography will demonstrate aortic and subclavian artery transection and helical CT now plays an important role in patient selection for angiography. Upper abdominal visceral injury is best evaluated with contrast-enhanced CT of the abdomen. Rib fractures may appear as radiolucent lines, steplike contour deformities, or overriding bone fragments on the chest radiograph (Fig. 8.3). Fractures of the costal cartilages are not visible on standard radiographs and are detected only when there is gross displacement (Fig. 8.4). While isolated rib fractures may not be significant, when they are present it is important to exclude associated pleural, vascular, and visceral injury and particularly pneumothorax. Sternal fractures result from severe direct trauma such as from a sudden forward thrust against the steering wheel of a car during rapid deceleration of the vehicle. They sometimes are visible on the chest radiograph but are imaged optimally with computed tomography. Kehdy et al. recently have described the utility of three-dimensional CT reconstructions in diagnosis and evaluation of sternal fractures (Kehdy et al. 2006). There is frequently an associated pneumomediastinum, pneumothorax, or pulmonary contusion (see Fig. 8.16). Fig. 8.2 Flail chest in a patient with multiple rib fractures. Fig. 8.3 Multiple rib fractures on the right side with hemothorax. Fig. 8.4 Fractures and dislocations of the bony thorax. Thoracic vertebral body fractures usually result from hyperflexion injuries. Fig. 8.5 Pneumomediastinum and chest-wall emphysema. The lateral chest radiograph/lateral thoracic spine may show vertebral body wedging. There may be a step-like deformity of the anterior vertebral margin as the compressed spongiosa produces a line of sclerosis. The degree of vertebral body fragment retropulsion is important to assess. On the frontal radiograph, associated paravertebral soft-tissue hematoma may cause a convex lateral bulge of the paravertebral stripe. CT of the thoracic spine with sagittal and coronal reformatted images will define accurately the extent of both bony and associated soft tissue injury. Magnetic resonance imaging (MRI) may be complementary to CT when there is clinical evidence of spinal cord or peripheral nerve root injury. Subcutaneous chest wall emphysema occurs when intrathoracic air leaks into the soft tissues. There is usually an associated pneumothorax or pneumomediastinum. A characteristic subcutaneous crackling sensation is noted on palpation. The chest radiograph shows vesicular or linear gas shadows and there may be quite marked thickening of the subcutaneous tissues. Characteristically, air also spreads along the fibers of the pectoralis major muscle and produces fan-shaped linear lucencies overlying the upper thorax (Figs. 8.5, 8.6). Fig. 8.6 Subcutaneous chest-wall and cervical emphysema. Linear gas shadows outline fibers of pectoralis major muscle. Air entering the pleural space results in a pneumothorax. Leakage is most commonly from the lung. A pleurocutaneous fistula resulting from penetrating chest injury and a bronchopleural fistula will also produce pneumothoraces. Traumatic bronchopleural fistulas usually result from nonpenetrating compressive trauma with sudden elevation of intra-alveolar pressure; this leads to alveolar rupture and tearing of the visceral pleura. The negative intrapleural pressure then draws air into the pleural cavity. Sharp rib fragments may also injure the pleura and result in pneumothorax. The elastic recoil of the lung may lead to closure of pleural tears through relaxation atelectasis. Occasionally, the visceral pleural flap may produce a check-valve obstruction with air entering the pleura during inspiration and air trapping within the pleura during expiration. This leads to a tension pneumothorax with mediastinal displacement and compression of major vessels and the contralateral lung. A tension pneumothorax constitutes a medical emergency. The following are relatively unusual causes of a pneumothorax; they, however, have important implications for patient management: A small pneumothorax may be asymptomatic but if it occupies more than 25% of the hemithorax it may lead to significant pulmonary atelectasis with hypoxemia and dyspnea. The hemithorax is hyperresonant to percussion and on auscultation breathing sounds are diminished. Tension pneumothorax is associated with progressively increasing chest pain, dyspnea, and cyanosis. When possible, an upright chest radiograph should be acquired. In severely traumatized patients, cross-table lateral or supine views only may be possible. On the frontal chest radiograph, the visceral pleura is separated from the chest wall and becomes visible as a laterally convex “pleural line” that parallels the chest wall (Fig. 8.8). Pulmonary vascular markings are absent lateral to this line. On both upright and decubitus views, intrapleural air is seen at the most superior point in the hemithorax except when loculation from adhesions is present. Tension pneumothorax is associated with complete pulmonary atelectasis. There is flattening of the ipsilateral hemidiaphragm, widening of intercostal spaces, and mediastinal shift to the contralateral side (Fig. 8.9). In the supine position, air tends to collect anteriorly. Radiographic findings in anterior pneumothorax include increased clarity of the mediastinal contours and costophrenic angle on the affected side. These signs frequently are subtle and may not be detected in the patient with multiple trauma (Dee 1995d). A number of studies have shown that only 40 to 50% of pneumothoraces are detected on supine radiographs in the clinical setting of acute trauma (Wall 1983, Tocino 1984). Fig. 8.7 Pneumothorax. Fig. 8.8 Visceral pleural line in peripheral pneumothorax. Pleural aspiration is advocated by some sources if the volume of the pneumothorax exceeds 25% of the hemithorax, if serial radiographs show a progressive increase in intrapleural air or if the pneumothorax persists for more than 1 week (Light 1983). Tension pneumothorax is life-threatening and requires immediate aspiration. Computed tomography is highly accurate in detection of pneumothoraces that may be missed on supine radiographs; sensitivities of up to 100% have been reported (Wall 1983, McGonigal 1990). The most superior images through the lung bases therefore should be reviewed at lung windows when CT abdomen is performed in patients with suspected intra-abdominal visceral trauma. Fig. 8.9 Tension pneumothorax with contralateral mediastinal displacement. Blood in the pleural cavity may be due to transection of pulmonary, mediastinal, or intercostal vessels. Large volumes of blood are unlikely to be secondary to pulmonary parenchymal injury as the expanding hemothorax tends to compress the lung and tamponade the hemorrhage. All except trivial hemothoraces should be evacuated to prevent development of fibrothorax. If the volume of the hematoma is more than 1500 mL or if drainage from the chest tube is more than 100 mL per hour, thoracotomy may be indicated (Light 1983).
Chest Wall Injuries
Rib Fractures
Clinical Features

Sternal Fractures

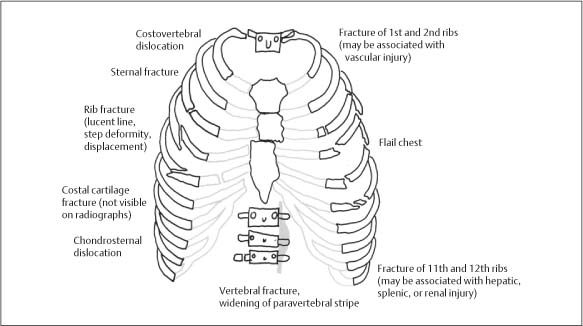
Vertebral Fractures
Radiologic Findings
Subcutaneous Emphysema
Radiologic Findings
Pleural Injuries
Pneumothorax
Pathology
Clinical Features
Radiologic Findings
Chest Radiograph (Fig. 8.7)
Computed Tomography
Hemothorax
Clinical Features
Radiologic Findings
Chest Radiograph
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree