Fig. 5.1
Anatomy of the trachea and lobar bronchi; also the segmental bronchi are represented in the picture. T trachea, RUL segmental bronchi of the right upper lobe, ML segmental bronchi of the middle lobe, RLL segmental bronchi of the right lower lobe, LUL segmental bronchi of the left upper lobe, LLL segmental bronchi of the left lower lobe
The thoracic portion of the trachea is deeper than the cervical part; it remains, throughout its length, in the anterior part of the mediastinum, ventral to the alimentary canal, and it is surrounded by connectival soft tissue, which is full of lymph nodes.
The tracheal walls are not wider than 2–3 mm and consist of approximately 20 cartilaginous rings, horseshoe-shaped, with an opening on the posterior side; the tracheal cartilages are usually calcified in older people and merge with the adjacent cartilage. The posterior membrane, with several mucous glands, is devoid of cartilage, but there are several smooth muscle fibers inserting into the posterior part of the cartilage laminae. The trachea is supplied by the superior and inferior thyroid arteries, the thymic and the right bronchial arteries. The veins are tributaries of the azygos system. The innervation originates from the vagus nerve and the sympathetic nerve.
The two main bronchi, right and left (Fig. 5.2) are, in their external conformation, similar to the trachea. They also have cartilaginous rings, more numerous on the left (up to 12). After originating they ramify at an angle between 75° and 85°, descending laterally, toward their own lung hila. The right bronchus is oblique, with an almost vertical orientation. The left bronchus is smaller and tends toward a horizontal direction. The different diameters reflect the difference in volume; the right lung prevails over the left one.
Fig. 5.2
Anatomy of the segmental bronchi T trachea, LMB left main bronchi, RULB right upper lobe bronchus, BI bronchus intermedius, B1 apical segmental bronchus of the right upper lobe bronchus, B1+2 apical-posterior segmental bronchi of the left upper lobe bronchus, B2 posterior segmental bronchus of the right upper lobe bronchus, B3 anterior segmental bronchus of the (right or left) upper lobe bronchus, B4 on the right, lateral segmental bronchus of the middle lobe bronchus and, the left, superior lingular segmental bronchus, B5 on the right, medial segmental bronchus of the middle lobe bronchus, and on the left, inferior segmental lingular bronchus, B6 apical segmental bronchus of the (right or left) lower lobe bronchus, B 7, 8, 9, 10 on the right, respectively, medial-basal segmental bronchus, anterior basal, lateral basal and posterior basal bronchus of the lower lobe bronchus, B 7+ 8, 9, 10: on the left, respectively, anteromedial segmental basal, lateral basal and posterior basal bronchus of the lower lobar bronchus
The bronchi enter into the pulmonary peduncles; at the level of the hilum, the branches of the pulmonary artery are in front of the main bronchus while the bronchial artery is posterior. The pulmonary veins, at the level of the hilum, are below and in front of the bronchus. Behind the bronchus, cranially, we find the azygos vein on the right, and the thoracic aorta on the left. The vagus nerve is located along the posterior wall of the bronchi, on both sides. The lymph nodes are located in the periphery of the bronchi.
5.1.4 Lungs
The lungs have a convex pyramidal shape, with their base on the diaphragm and the apex toward the base of the neck; they are completely contained in the thoracic cavity and separated from the abdominal cavity by the diaphragm. The lung volume is not equal and, in any case, it changes during the different respiratory phases. The right lung descends less than the left lung, because of the gibbosity of the underlying right hepatic lobe and the corresponding change in shape of the diaphragm. The left lung has an inferior transverse diameter because of the depression containing the heart on the medial, or mediastinal, side, and its volume is almost one-fifth or one-sixth smaller than the other lung. Besides its typically weak and spongy consistency, the pulmonary parenchyma is very elastic and cohesive as it needs to resist the high intrinsic air pressure.
From a frontal view, the lung reaches 2 cm above the medial third of the clavicle. Posteriorly, the pulmonary apex is on both sides at the level of the first thoracic vertebra. On the right, the anterior lung margin reaches the medial line at the level of the sternal angle, and continues caudally, up to the level of the sixth chondrosternal joint. Therefore, the pulmonary margin curves laterally slightly, crossing the sixth rib on the emiclavear line, and the eighth rib on the midaxillary line. On the left, at the level of the fourth costal cartilage, the presence of the heart causes a lateral deviation of the lung, which, as previously explained, is expanded below rather than on the right. The inferior margin of the lung is located at the level of the diaphragmatic vault, between the eight and the ninth thoracic vertebrae on the right side, and slightly further down on the left side.
The anatomy of the lungs consists of three autonomous portions of parenchyma called lobes, determined by the pleural fissures, three lobes on the right side (upper, middle, and lower lobe) and two (upper and lower lobes) on the left, where the horizontal fissure is missing; it may vary in the case of other accessory fissures.
On both sides, the upper lobe is located in the anterior–superior part, and the lower lobe is located in the inferior–posterior part. The middle lobe is wedge-shaped with the base at the front and the apex toward the hilum.
The partition in segments, on the basis of the bronchial branches, divides each lobe into two to five segments, for a total of ten on the right and eight on the left. The pulmonary segments, from the radiological and surgical points of view, can be identified as the topographical reference unit of the lung. It may be defined as the pulmonary area supplied by fourth-generation bronchi, and, namely, the branches of a lobar tertiary bronchus –the primary bronchi being the second generation and the trachea the first generation (Fig. 5.3). The artery supplying a segment follows the course of the segment; the relevant veins are located on the peripheral side of the segment and are a good reference point.
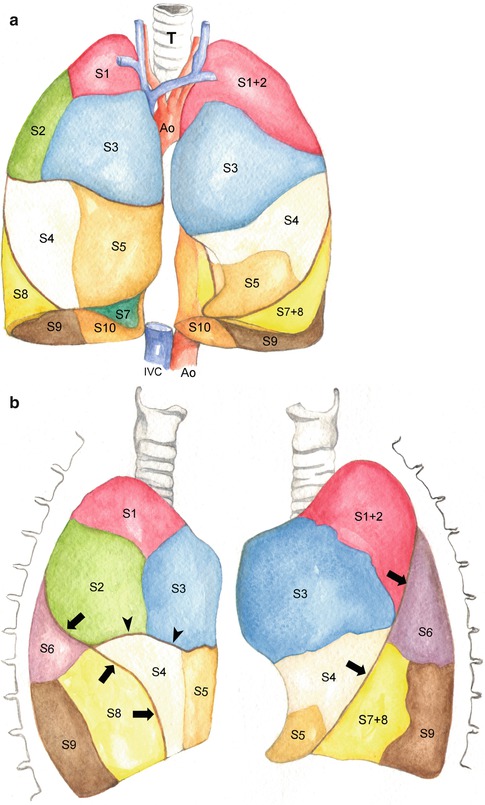
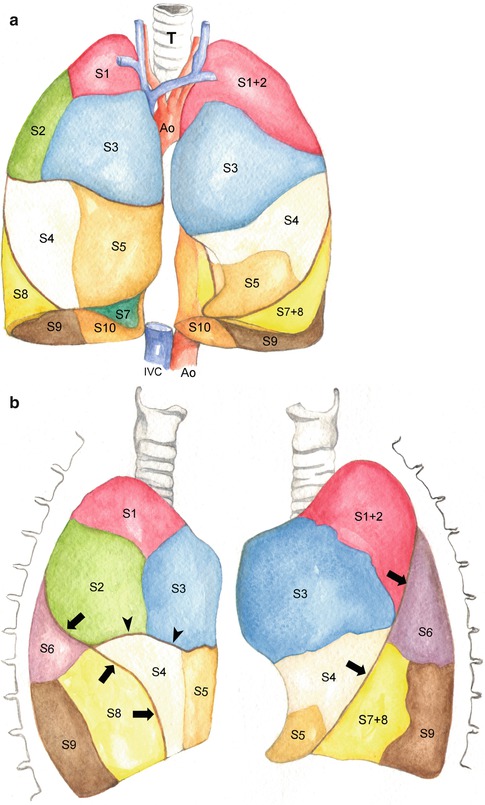
Fig. 5.3
Anatomy of the lung segments, frontal (a) and lateral view (b). S1 apical segment of the right upper lobe, S1+2 apical-posterior segment of the left upper lobe, S2 posterior segment of the right upper lobe, S3 anterior segment of the (right or left) upper lobe, S4 on the right, lateral segment of the middle lobe and, on the left, ligular upper segment, S5 medial segment of the middle lobe and, on the left, inferior ligular segment, S6 apical segment of the (right or left) lower lobe, S 7, 8, 9, 10 on the right, respectively, medial basal segment, anterior basal, lateral basal and posterior basal segment of the lower lobe, S 7+ 8, 9, 10 on the left, anteromedial basal segment, lateral basal and posterior basal segment of the lower lobe. IVC inferior vena cava, Ao aorta, T trachea. The arrow show the right major fissure and the left one; the arrowheads show the small left fissure
The upper right lobe consists of the apical segment, forming the apex of the lung; the posterior segment, going up to the lateral part of the minor fissure, and the superior part of the major fissure; the anterior segment, vertically positioned, up to the minor fissure, at the level of the fourth rib. In the middle lobe we find the middle and lateral segments, divided by a plane between the pulmonary hilum and the inferior part of the major fissure. The lower right lobe consists of the superior (or apical) segment, which occupies the whole superior part and it is usually transverse to the basilar segments, following the superior part of the major fissure, up to the vertebral side of the fifth and sixth ribs; four segments forming the so-called basal pyramid, the middle segment (exclusively in the right lung, it is sometimes separated by an accessory fissure), the anterior, lateral, and posterior segments. The upper left lobe is characterized by a bronchus that ramifies into the superior and inferior (or lingular) branches, each of them in turn divided into two segmentary bronchi. In the left upper lobe, therefore, we find the anterior segment, and the apical–posterior segment, originating from the fusion of the two segments that are separated in the right lung. The lingua, quite similar to the right middle lobe, is divided into superior and inferior segments. In the lower left lobe, contrary to the right one, the apical segment is oblique in comparison with the below segments. The bronchi of the basal segments originate from a unique trunk; usually, there is a unique bronchus for the middle basal segment, and for the anterior basal segment. The posterior basal segment is wider than the right one.
After the fourth generation, where the diameter of the bronchial segments was about 6 mm wide, we find subsegmental bronchi (up to the 9th generation), small bronchi (from the 10th to the 12th generations), bronchioles (from the 13th to the 14th generations), and terminal bronchioles (for the following two generations), respiratory bronchioles (from the 17th to the 22nd generations), alveolar ducts (corresponding to the 23rd generation), and the alveoli (the 24th generation, with a diameter of 250 μm).
From a functional point of view, we can distinguish three separate areas in the airways: the conducting zone, from the trachea to the terminal bronchioles; the transitional zone, from the respiratory bronchioles to the alveolar ducts, with both conducting and respiratory functions; and the third zone, the alveolar respiratory zone; it forms the parenchyma and represents 90 % of the pulmonary volume along with the corresponding capillary vessels: more than 50 % of the air is normally contained in the alveoli. The considerable number of alveoli (estimated at around 400 million), helps to understand the intensity of the air-exchange processes through the alveoli membrane, which is devoid of connective cells, but is characterized by smooth muscle cells. The transitional and respiratory zones, which, as previously explained, run from the respiratory bronchioles to the alveoli, are the respiratory units called acini, whose shape and size vary in adults for a maximum of 7–8 mm (Fig. 5.4); the acini are delimited, but not isolated, by connective tissue, and the air is also exchanged between adjacent acini.
Fig. 5.4
Anatomy of the pulmonary acinus. Tb terminal bronchiole, Rb1 first generation respiratory bronchiole, Rb2 second generation respiratory bronchiole, Rb3 third generation respiratory bronchiole, As alveolar sac
Three units of the lung structure at the subsegmental level have been described. These units consist of the primary lobule, the secondary lobule, and the above-mentioned acinus, originally described by Miller. The primary lobules may have different shapes and volume; they originate from the last respiratory bronchiole and consist of a series of alveolar ducts, atria, alveolar sacs, and alveoli, along with the relevant vessels and nerves. The secondary lobules are defined as smaller lung portions, surrounded by septal connective tissue. Their size and extension may vary, and the number of primary lobules forming a secondary pulmonary lobule is between 30 and 50.
From another perspective we can consider “large” all the airways made of cartilage (that in the peripheral regions permeate the bifurcation points only), supplied by bronchial blood vessels and subject to dynamic compression during forced exhalation. Starting from the bronchioles, with a diameter inferior to 1 mm, we can talk about “small” airways, with smooth parietal muscles and supplied by pulmonary vessels.
There are two vascular systems in this area: the pulmonary circulation, coming from the heart, and the bronchial circulation, coming from the aorta. The pulmonary artery, whose transverse section is generally slightly inferior to the section of the aorta, divides, just after its origin, into two branches, the bronchial arteries. The right pulmonary artery is longer and located between the superior vena cava and the main homolateral bronchus, and it divides into two branches, the superior branch, and the interlobar descending branch. The left branch passes over the main left bronchus, cranially, and, more frequently, it continues vertically into the interlobar artery, situated at the back of the inferior lobar bronchus, from where the segmental branches of the lower and upper lobe originate. The structures responsible for the vasomotor regulation of the pulmonary circulation are the pre-capillary vessels, along with the respiratory bronchioles. The diameter of the almost innumerable pulmonary capillaries is not wider than 7–9 μm. They are so thin that the red blood cells must line up in a single file. The capillary bed is drained by the pulmonary veins. Two tributary veins merge together at each bifurcation point of the airways. Two pulmonary veins from each lung receive blood from three or four bronchial veins, and drain into the left atrium.
The main controller of the autonomous nervous mechanisms is represented by the parasympathetic nervous system with bronchoconstriction function; the bronchial tone is also subject to the activity of the superficial sensory receptors.
5.1.5 Pleura
The pleura is a serous membrane formed by two layers of thin epithelium (mesothelium), located on the walls of the thoracic cavity, and surrounding the organs contained therein: the parietal pleura and visceral pleura. The former is attached to the chest wall, diaphragm, and mediastinum; it forms an acute angle when passing from the ribs to the diaphragm, originating the costodiaphragmatic sinus. It becomes smaller during inspiration, allowing the insinuation of the lung. The visceral layer is strictly attached to the lung; its external surface is therefore smooth, except for the hilum, where the visceral pleura reflects on the parietal pleura. The visceral layer adheres to the lung through a thin layer of connective tissue, the subpleural tissue, which continues into the pulmonary interlobular connective tissue.
The two pleurae delimit, in each hemithorax, a (pleural) virtual cavity that is normally oiled by a minimal amount of serous fluid that allows the membranes to slide during the respiratory kinetics. The right and left pleura have no anatomical connections, but they have three contact points: in front of the descending aorta, just behind the heart, and below the aortic arch.
The right pleural cavity is delimited by the contralateral of the mediastinum that progressively narrows from bottom to top, covered by the mediastinal pleura; the part against the parietal pericardium is termed pericardial pleura. The mediastinal pleura continues, both anteriorly and posteriorly, into the costal pleura, on the internal face of the ribs, the corresponding intercostal spaces, and the lateral face of the vertebral bodies; below, the diaphragmatic pleura adheres to the underlying muscle.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree