Fig. 1
Example of soft tissue sarcoma radiotherapy immobilization. (a) A right foot immobilized for a radical course of radiotherapy to the right thigh. Rotation is secured by the mini vacuum cushion placed underneath the limb which also provides patient comfort for the longer RT treatment delivery times typical of IMRT/IGRT/Tomotherapy/3D CRT. (b) A thermoplastic shell is molded over the limb to reduce patient setup uncertainty in all dimensions. This immobilization system attaches to the radiotherapy treatment couch. It can be used for upper and lower extremity immobilization. (c) Upper extremity immobilization for an STS sarcoma of the elbow. A larger mini vacuum cushion is utilized to support the contour change from the shoulder to the wrist typical of this anatomic area. (d) Another STS sarcoma of the elbow using a modified version of the device shown in (a). Styrofoam is used instead of the vacuum cushion for superior hand definition in the thermoplastic mold. Both systems attach to the radiotherapy treatment couch. (e) Medial upper thigh sarcoma immobilized with a device placed on the foot to secure rotation and reduce setup uncertainty. Five permanent tattoos are used to enhance patient setup consistency; the tattoos are artificially depicted by the white crosses in this image. The tattoos were used for daily patient positional reproducibility and alignment, in addition to other marks placed on the immobilization device. The scrotum is retracted from the treatment volume. (f) A retroperitoneal sarcoma setup using a large polystyrene vacuum cushion to support the arms away from the treatment volume with 5 setup tattoos. One is placed on each side of the patient for rotational reproducibility and 3 along the central axis for patient alignment (see 4 white crosses depicting the 3 central axis tattoo points with the right lateral visible tattoo point)
Achieve optimal normal tissue avoidance in RT planning
Facilitate the most straightforward RT beam arrangement
A reproducible marking on the patient should be defined for daily setup points of reference (i.e., permanent tattoos).
A six-point patient setup system is ideal, with three setup points chosen along the central axis plane and three along the sagittal plane.
Preferably, these points should be placed above and below a joint to assess and maintain the joint angle throughout RT and should also be placed beyond any anticipated tumor volume changes as shown in Fig. 1c–f.
For highly conformal RT techniques, reinforcement of limb stability is important to ensure fixed rotation is maintained throughout the treatment. This can be accomplished with a thermoplastic sheet molded, as in head and neck immobilization for radiotherapy, over the top of the limb and secured to the treatment couch.
Any chosen immobilization device should attach to the RT treatment couch securely to reinforce stability in all dimensions and maximize setup reproducibility. Various immobilization devices appropriate to different anatomic sites are available.
Pelvic, abdominal, and retroperitoneal patients require positional support for their arms, which must be spatially separated from the treatment volume (e.g., optimally supported above their head). This can be accomplished with a large polystyrene vacuum cushion or other commercial device that supports the desired arm position (see Fig. 1f).
Daily image guidance is preferred. For example, 2D KV/2D MV for orthogonal localization or 3D image guidance (i.e., cone beam CT) for target volume/soft tissue localization.
4 Target Volume Delineation and Treatment Planning
For preoperative planning target volume definition, CT simulation imaging fused with MR imaging should be performed, ideally with the patient in the treatment position. These will facilitate delineation of the gross tumor volume (GTV) and clinical target volume (CTV) (see Figs. 2 and 3).

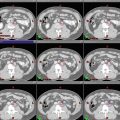
Fig. 2
T2bN0M0 grade 3 dedifferentiated liposarcoma in the posterolateral thigh treated with preoperative radiotherapy to 50 Gy in 25 fractions. This patient presented with a previous unplanned and incomplete excision of a superficial lesion where the fascia of the vastus lateralis was breached, and the tumor had not involved the deeper compartment originally. CT simulation used 2.0 mm slice thickness. Note the area of violated fascia (arrows) due to previous surgical error which now must be included in the CTV with a substantial volume increase (also see Fig. 3). Shown are representative slices

Fig. 3
Example of the GTV, CTV, and PTV for the case in Fig. 2 displayed in the sagittal view as well as an axial MRI view of the disrupted fascia as a result of an unplanned excision with the corresponding planning CT target volumes
For postoperative planning target volume definition after presumed complete surgical resection, there is no GTV to delineate. The location of the original GTV following the operation ( postop GTV) should be recreated as realistically as possible in the original planning CT dataset using preoperative CT/MR imaging if available (see Figs. 4 and 5).

Fig. 4
T2bN0M0 grade 3 pleomorphic rhabdomyosarcoma in the left anterior thigh treated with postoperative radiotherapy to 66 Gy in 33 fractions. This patient received postoperative RT for negative but close margins. CT simulation used 2.0 mm slice thickness. Edema was contoured in the superior aspect of the postop GTV and included in the CTV56. Shown are representative slices. CTV56 is limited by the femoral head and bone throughout the target. In some cases where the subcutaneous tissues have been contaminated, bolus may be applied to the surgical scar for a component of the treatment (e.g., 50 Gy)

Fig. 5
Sagittal CT simulation view of the radiotherapy target volumes for the postoperative STS case demonstrated in Fig. 4 with the corresponding preoperative and postoperative MRI. Note the CTV56 is defined by edema and the postoperative surgical changes. Where the CTV and PTV target volumes may appear concordant in this scaled anatomic illustration, the usual margins were applied (e.g., 0.5–1 cm PTV expansion). In addition, the preoperative imaging was imported and co-registered with the postoperative RT planning CT dataset in order to appreciate the original tumor extent for delineation of the postop GTV
For preoperative cases, 50 Gy is ordinarily used and target volumes include the GTV and the CTV50 and should be delineated on every slice of the planning CT dataset.
For postoperative RT delivery, 66 Gy is ordinarily used (60 Gy can be used in surgical margin clear, low-grade cases) and should encompass the prior location of the GTV with an additional peripheral elective subclinical CTV volume for tissues with lesser risk of microscopic tumor infestation, i.e., equivalent to 50 Gy in 25 fractions, e.g., 56 Gy in 33 fractions, or 54 Gy in 30 fractions if a simultaneously integrated boost technique is used (see Table 2 and Fig. 5).
For unresectable residual gross disease, 70 Gy in 2 Gy/fraction or an equivalent dose fractionation is ordinarily used depending on the tolerance of the anatomic region. This is delivered to the location of any residual GTV with an additional peripheral elective dose CTV volume.
Suggested target volumes for different treatment settings are as follows:
GTV and CTV50 for preoperative IMRT of extremity STS are detailed in Table 1. (Figs. 2, 3, 10, 11, 12, 13)
Table 1
Suggested target volumes for preoperative extremity STS
Target volumes
Definition and description
GTV
Primary: all gross disease on physical examination and imaging. T1-weighted contrast-enhanced MRI preferable (Fig. 2). Co-registration of the MRI and planning CT datasets is facilitated by immobilizing the patient in the treatment position
CTV50 a
Includes all areas at risk of subclinical spread defined by the distance from the GTV or edema
Includes the GTV + 4 cm margin in the longitudinal dimensions + 1.5 cm margin in the radial dimension limited to but including any anatomic barrier to tumor spread, such as the bone and fascia (Fig. 2)
Suspicious peritumoral edema, best demonstrated on T2-weighted MRI sequences, may contain microscopic tumor cells and should be contoured separately with an adequate margin (usually 1–2 cm)
For cases of “unplanned excision,” margins should include postop GTV or any residual GTV and all surgically manipulated and disturbed tissues and violated fascia + 4 cm longitudinally + 1.5 cm radially limited to but including any barrier to tumor spread
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree

 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access