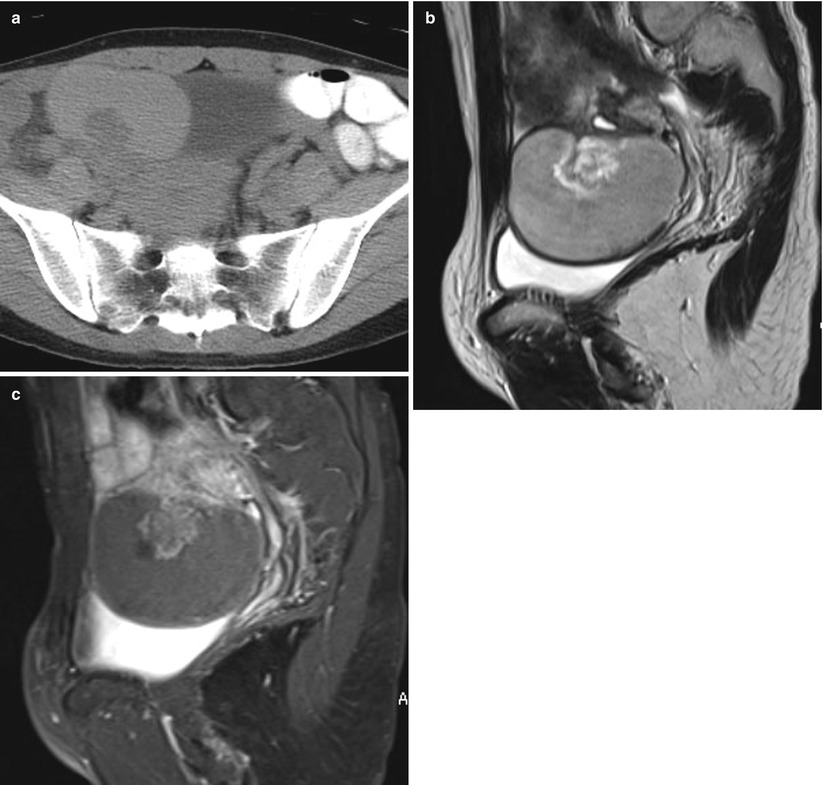
Fig. 1
(a) A 49-year-old woman with benign serous cystadenoma. Contrast-enhanced computed tomographic scan shows a unilocular cystic mass in the pelvic space. There are no solid components. (b) Sagittal T2-weighted magnetic resonance (MR) image shows a large cystic mass with a septation in the pelvic space. (c) Sagittal fat-saturated contrast-enhanced T1-weighted MR image shows a large cystic mass with a septation and no solid component in the pelvic space
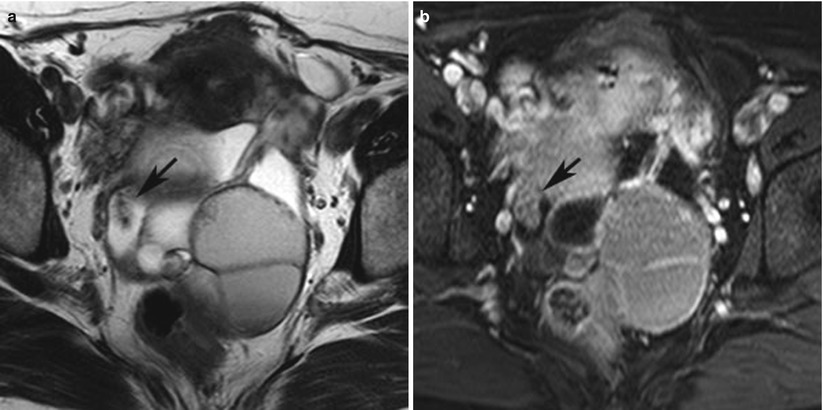
Fig. 2
(a) A 52-year-old woman with serous borderline tumor. Axial T2-weighted magnetic resonance (MR) image shows a complex cystic mass with multiple septa. Large papillary projection shows high signal intensity with low signal intensity cores (black arrow). (b) Axial fat-saturated contrast-enhanced T1-weighted MR image shows a large complex cystic mass with multiple septa. Large papillary projection shows high signal intensity with slightly low signal intensity cores (black arrow)
The signal intensity of the contents of serous cystic lesions varies but is usually low to intermediate on T1-weighted MR images and high on T2-weighted images. At CT, psammomatous calcifications can show these tumors or their implants to have very high attenuation [17]. On MR images, serous borderline ovarian tumors appear as unilocular cysts with papillary projections within the cyst wall (Fig. 3a, b), minimally separate cysts with septa that demonstrate frond-like papillary projections within the cysts that involve both the wall and septa (Fig. 4a, b), or markedly septate lesions with plaque-like excrescences (Fig. 5a–c) [16]. Approximately one-third of these tumors are bilateral. The papillary projections of the solid components commonly show moderate enhancement during contrast-enhanced CT or dynamic MR imaging. Subtraction 3-dimensional (3D) enhanced T1-weighted images are especially useful when intracystic fluid shows high signal intensity on T1-weighted image (Fig. 5c) [19].
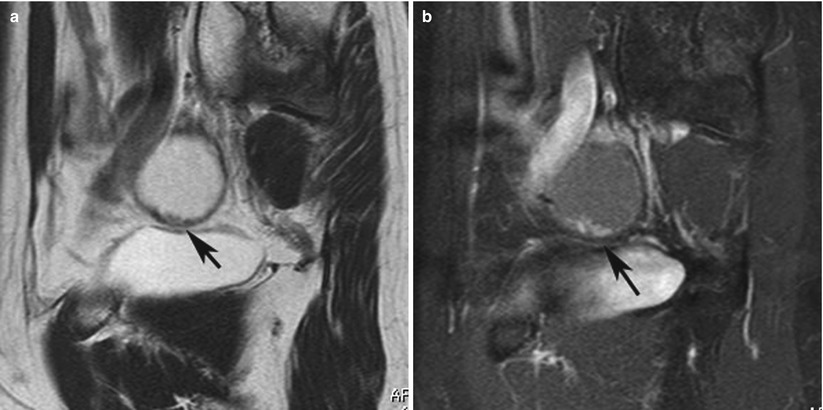
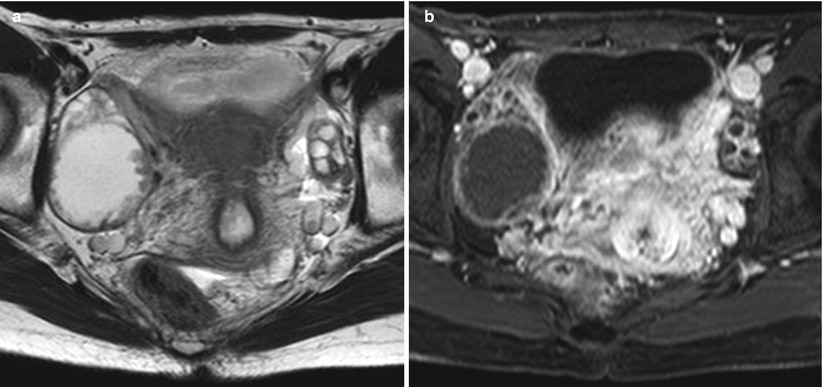
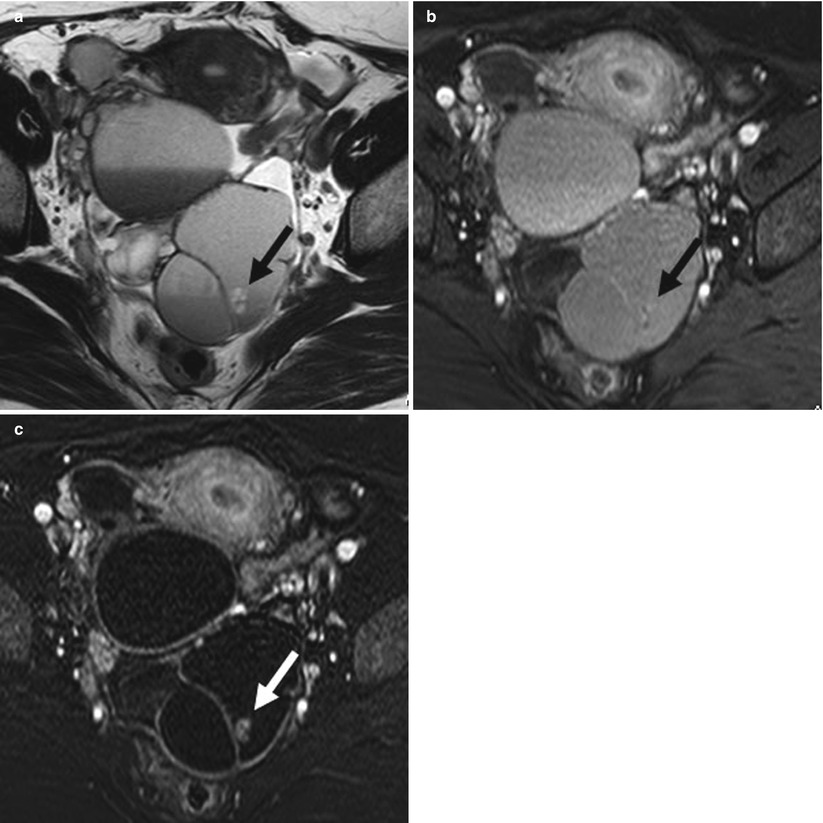
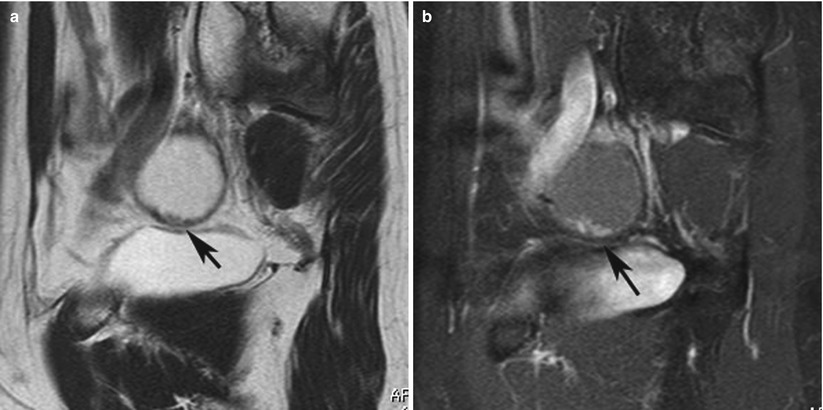
Fig. 3
(a) A 52-year-old woman with serous borderline tumor. Sagittal T2-weighted magnetic resonance (MR) image shows unilocular cystic ovarian lesion superior to the bladder. Intracystic papillary-like projections showing multiple areas of low intensity extend from the cystic wall (black arrow). (b) Sagittal fat-saturated contrast-enhanced T1-weighted MR image following gadolinium administration shows unilocular cystic ovarian lesion superior to the bladder. Intracystic papillary-like projections showing multiple areas of high signal intensity extend from the cystic wall (black arrow)
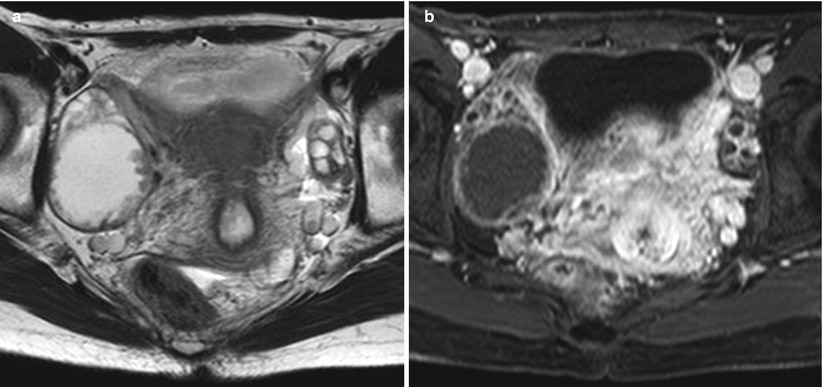
Fig. 4
(a) A 44-year-old woman with serous borderline tumor. Axial T2-weighted magnetic resonance (MR) image shows a solitary cystic lesion with several septa with intracystic papillary projections showing multiple small areas of slight low intensity in both the wall and septa in the right adnexal region. (b) Axial fat-saturated contrast-enhanced T1-weighted MR image shows a solitary cystic lesion with several septa with intracystic papillary projections showing multiple small areas of slight high signal intensity in both the wall and septa in the right adnexal region
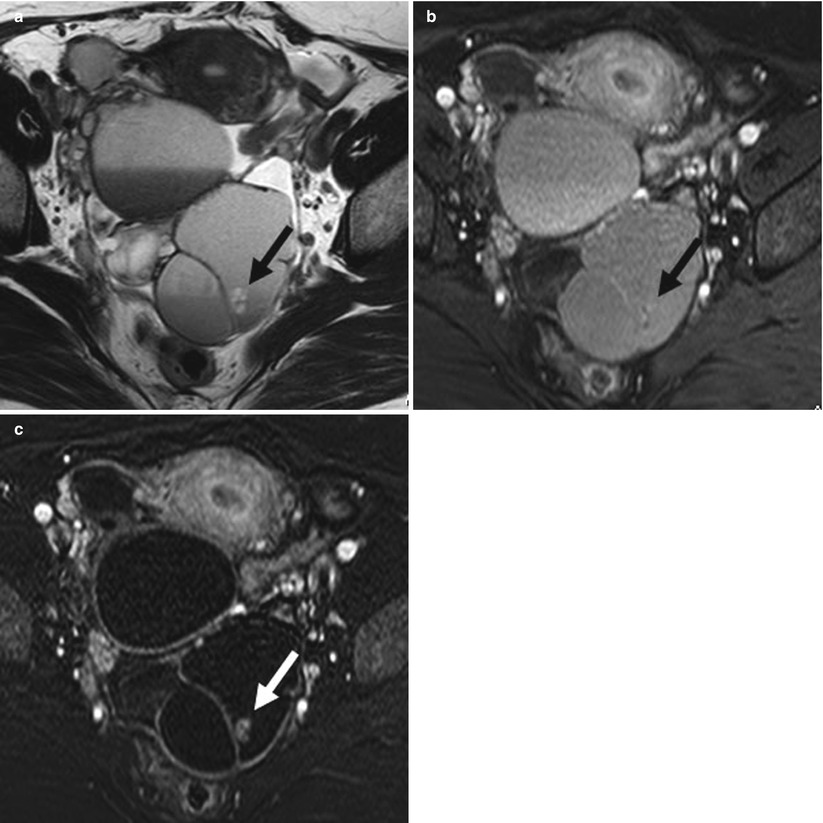
Fig. 5
(a) A 65-year-old woman with serous borderline tumor. Axial T2-weighted magnetic resonance (MR) image shows a large complex cystic mass with multiple septa. Irregular plaque-like soft tissue shows high signal intensity (black arrow). (b) Axial fat-saturated contrast-enhanced T1-weighted MR image shows a large complex cystic mass with multiple septa. Irregular plaque-like soft tissue is present but unclear (black arrow). (c) Axial 3-dimensional (3D) fat-saturated T1-weighted MR subtraction image shows a large complex cystic mass with multiple septa. Irregular plaque-like soft tissue displays strong contrast enhancement (white arrow)
Differential Diagnosis of Serous Borderline Ovarian Tumor
Serous borderline tumors often present as complex adnexal masses. Serous cystadenoma or mucinous cystadenoma may be a probable differential diagnosis. Neither of these has a solid component, and subtraction 3D enhanced T1-weighted images are useful to rule out debris or thrombus. Because serous borderline ovarian tumors appear benign clinically, their differentiation from early invasive malignant ovarian tumor is important.
Both serous borderline and stage I invasive malignant ovarian tumors are usually multiloculated with significant solid elements that include smooth round nodules, plaque-like thickening, and papillary projections. Septation thickness and nodule size are greater in malignant tumors, and papillary projections are more frequent in serous borderline tumors.
The imaging findings of serous borderline ovarian tumors are indistinguishable from those of other borderline ovarian tumors, such as mucinous, endometrioid, clear cell, transitional cell, and mixed-type tumors, except for the serous surface papillary borderline tumor, which is described immediately following. However, serous borderline ovarian tumor may be the more probable diagnosis when MR imaging shows the ovary as unilocular or with minimally separate cystic lesions with the signal intensity of water and containing multiple papillary projections.
Focus Points
Serous borderline tumor should be considered when an ovarian cystic tumor with papillary projections is seen in younger patients.
Serous Surface Papillary Borderline Tumor
General Considerations for Serous Surface Papillary Borderline Tumor
Serous benign tumors include cystadenomas, adenofibromas, cystadenofibromas, and surface papillomas. Serous surface papillomas are benign tumors that grow exophytically on the ovarian surface. Such tumors that demonstrate little or no involvement of the serous borderline tumor are termed serous surface papillary borderline tumor [20] and generally manifest as an entirely solid mass without necrosis or hemorrhage or as a solid mass with cyst [20, 21]. Serous surface papillary borderline tumor may be a precursor of low-grade serous surface papillary carcinoma in the adenoma–carcinoma sequence because the two entities can coexist [8].
Imaging Appearances of Serous Surface Papillary Borderline Tumor
On CT, serous surface papillary borderline tumors demonstrate varying proportions of solid components on the ovarian cystic surface (Fig. 6a). The CT findings are similar to the malignant ovarian tumor with peritoneal dissemination. The limited soft-tissue contrast of the CT did not permit visualization of the normal ovaries inside the masses, but the good soft-tissue contrast of MRI allowed our observation of the characteristic ovarian features of this tumor. On MR imaging, a T2-weighted image showed papillary architecture with high signal intensity and a hypointense branch-like structure on the surface of the normal ovary, findings resembling a sea anemone that suggest serous surface papillary borderline tumor (Fig. 6b) [20, 21]. Histologically, this papillary architecture correlates with epithelial multilayering, and the branching structure is a thick fibrous stalk [20]. After gadolinium administration, the papillary architecture on the T2-weighted image showed strong high signal intensity, and the low signal intensity of the branch-like structure was weakly enhanced.
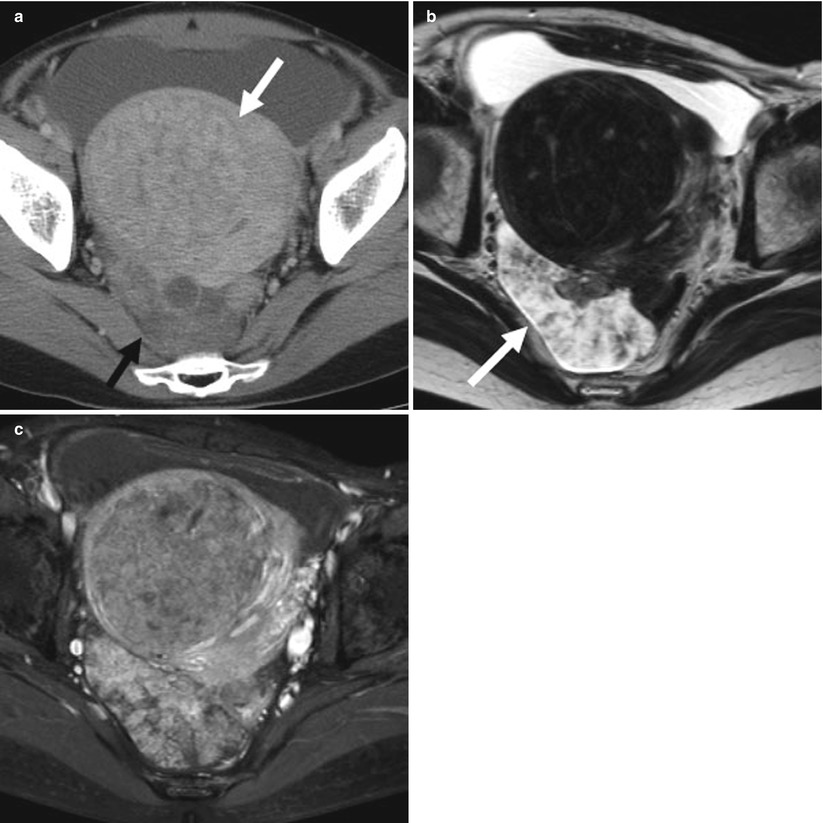
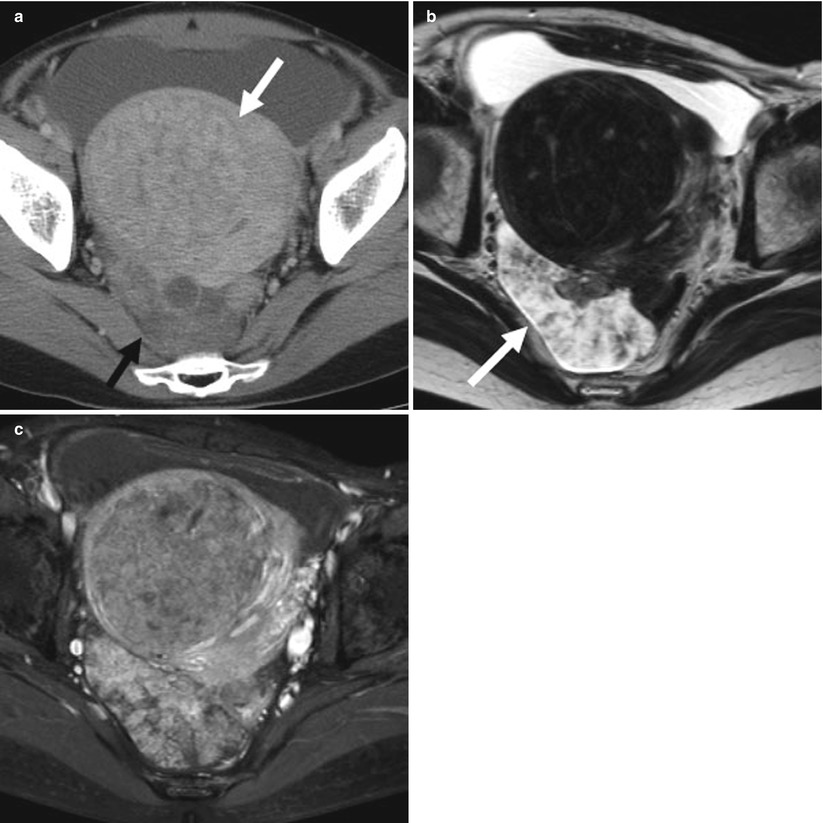
Fig. 6
(a) A 41-year-old woman with serous surface papillary borderline tumor. Contrast-enhanced computed tomography (CT) shows a heterogeneous enhanced mass posterior to the uterus (black arrow). White arrow is uterine leiomyoma. (b) Axial T2-weighted image shows an entirely solid lobulated mass with hyperintense papillary architecture on the surface and hypointense branch-like structure within it (white arrow). (c) Axial fat-saturated T1-weighted image shows an entirely solid lobulated mass; the papillary architecture shows high signal intensity after administration of gadolinium diethylenetriaminepentaacetic acid (DTPA)
Differential Diagnosis of Serous Surface Papillary Borderline Tumor
On diagnostic MRI and CT, ovarian tumors with a rich solid component are considered malignant. However, serous surface papillary borderline tumors have many solid components and so resemble malignant ovarian tumors, and they sometimes show multiple solid components with cystic lesion that may mimic peritoneal dissemination and malignant ovarian tumor (Fig. 7a–c). Accurate diagnosis requires evaluation of images of different direction and detection of the high signal intensity of papillary architecture and low intensity of branch-like structures on the ovarian surface that resemble sea anemone-like masses on T2-weighted images (Fig. 7b, c).
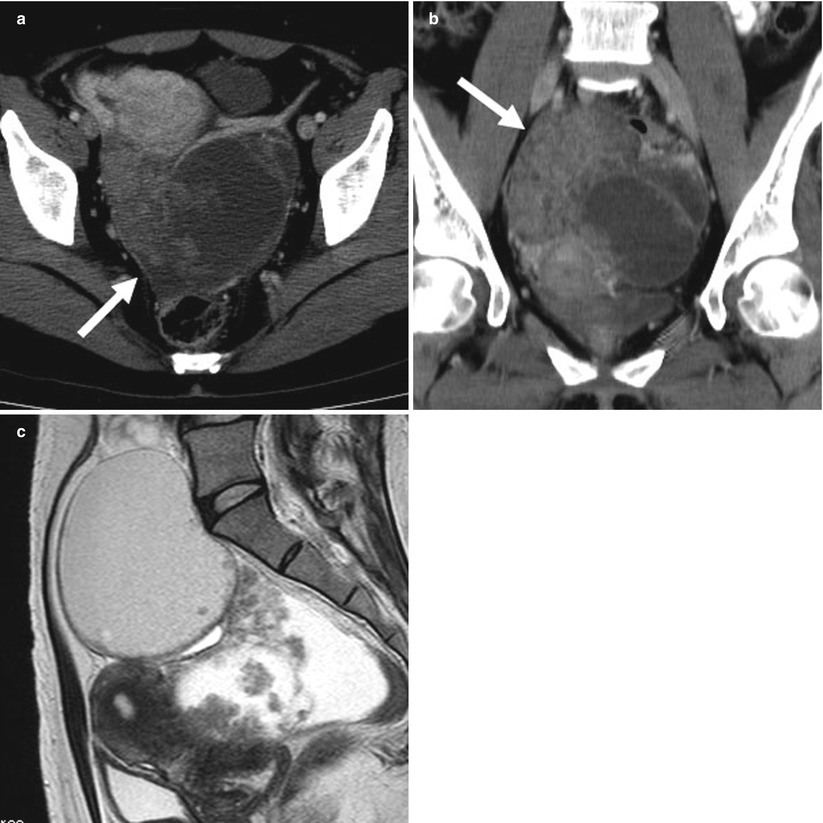
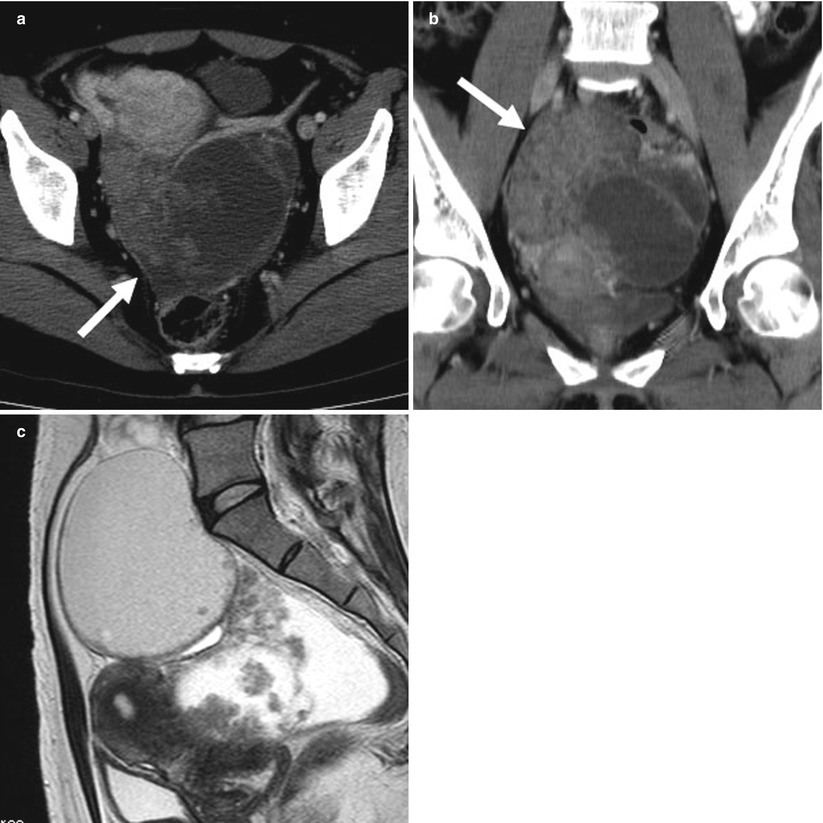
Fig. 7
(a) A 37-year-old woman with serous surface papillary borderline tumor. Contrast-enhanced axial computed tomography (CT) shows a cystic and solid mass (arrow) posterior to the uterus in the pelvis. The axial CT image is similar to that of peritoneal dissemination posterior to the uterus. (b) Contrast-enhanced coronal CT shows cystic masses superior-right lateral to solid components (arrow) in the pelvis. (c) Sagittal T2-weighted image shows that hyperintense papillary architecture on the surface and hypointense branch-like structure within the mass on the surface of cystic lesion
Focus Points
Serous surface papillary borderline tumor should be considered when an ovarian solid mass shows papillary architecture with high signal intensity and branch-like structures on the surface of the ovary with low intensity on T2-weighted image.
Mucinous Borderline Ovarian Tumor
General Considerations for Mucinous Borderline Ovarian Tumor
Mucinous borderline ovarian tumors account for approximately 10 % of mucinous ovarian tumors and 30–50 % of ovarian epithelial borderline tumors [19]. They are classified as either intestinal or endocervical type [19], which show very different pathologic and imaging features.
Intestinal Type Mucinous Borderline Tumor
Intestinal type mucinous ovarian borderline tumors represent about 90 % of mucinous borderline tumors. Mean age of patients is 45–50 years [22]. The average size of these tumors is about 20 cm, and they are usually unilateral, occurring bilaterally in only about 5 % of cases. The tumors are rarely associated with ipsilateral ovarian endometriosis [22] and are reported to coexist with pseudomyxoma peritonei in up to 17 % of cases [19].
Imaging Appearances of Intestinal Type Mucinous Borderline Tumor
On CT and MR imaging, intestinal type mucinous borderline ovarian tumor may be twice the size of serous borderline ovarian tumors and manifest as either uni- or multilocular cystic masses (Fig. 8a–c) [16], though a unilocular cystic mass is usually a serous borderline tumor. Mucinous borderline ovarian tumors commonly appear as multilocular cystic masses with numerous septa and contain fluids of different signal intensities on T1– or T2-weighted MR images (Fig. 9a–c) [8]. The variable signal intensities of the loculi and daughter cysts on both T1– and T2-weighted images is described as having a “stained-glass” appearance. These variable signal intensities depend on the viscosity of the materials present, such as mucin, blood products, or debris, and these findings suggest mucinous cystic tumor [23–25].
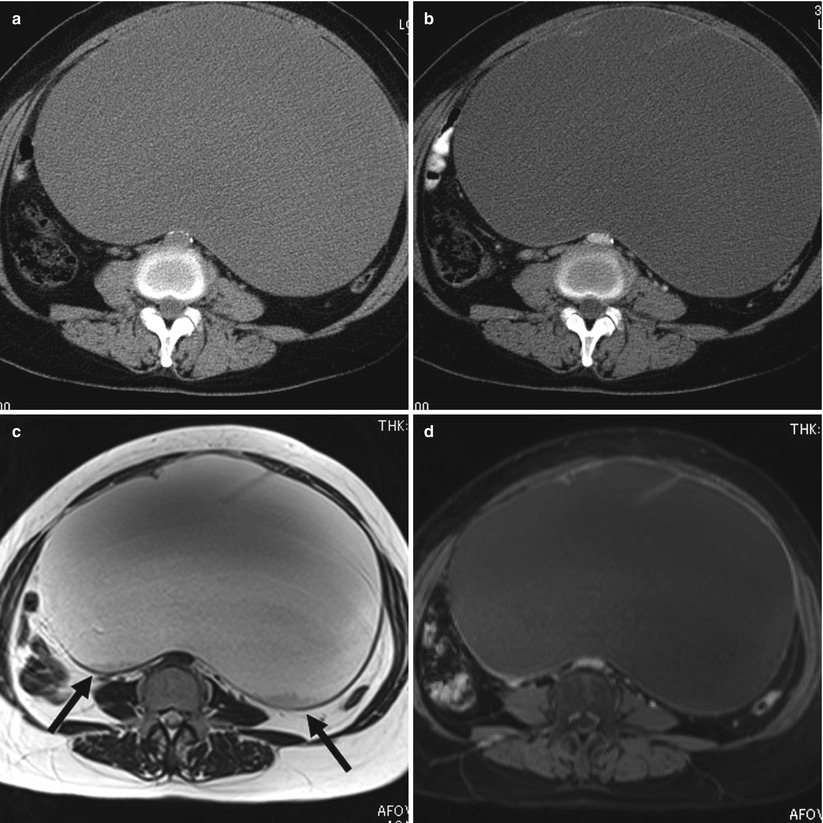
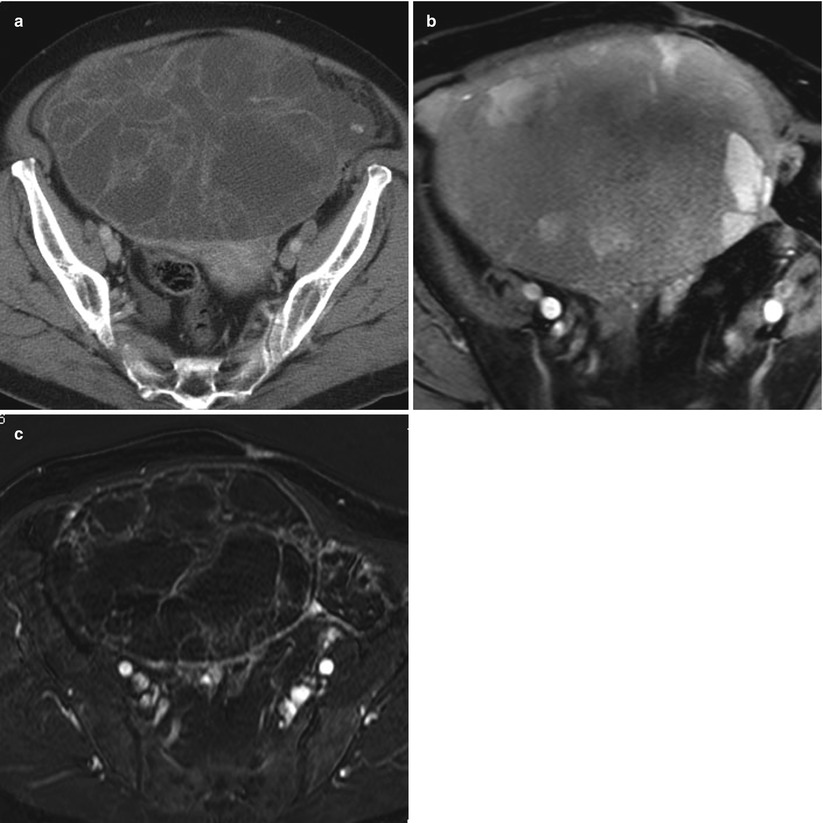
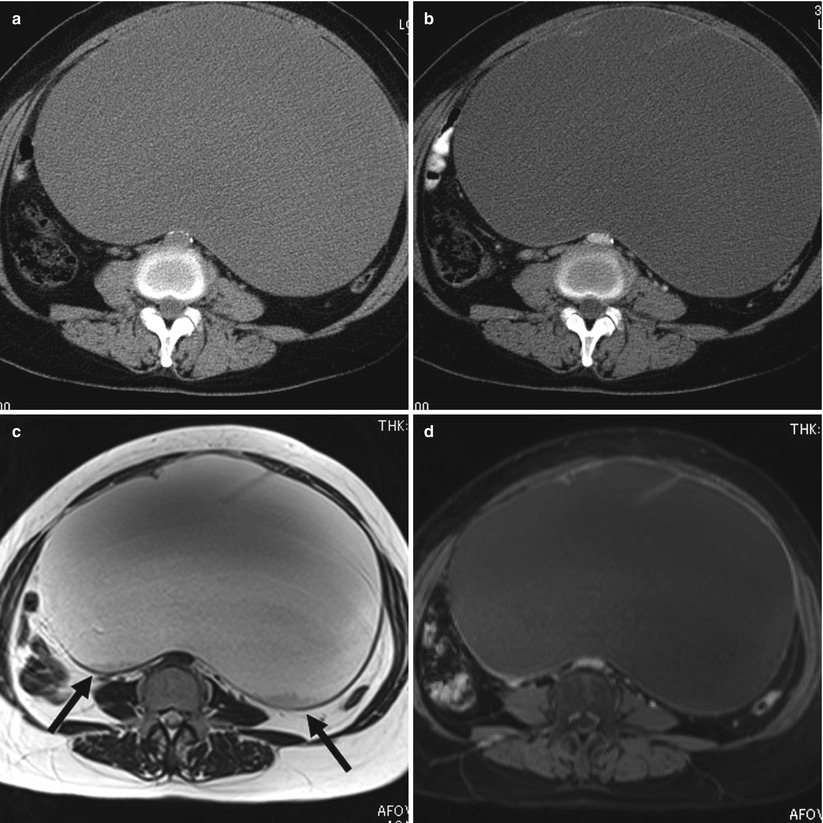
Fig. 8
(a) A 59-year-old woman with mucinous borderline tumor of intestinal type. Axial plain computed tomographic (CT) image shows large cystic mass and homogeneous density. (b) Axial contrast-enhanced CT image shows large cystic mass with thick septa and wall. (c) Axial T2-weighted magnetic resonance (MR) image shows a large cystic lesion with thick septa and globules of intermediate signal in the dorsal aspect (black arrows). (d) Axial fat-saturated contrast-enhanced T1-weighted MR image shows a large cystic lesion with thick septa. The globules in the (c) do not demonstrate contrast enhancement
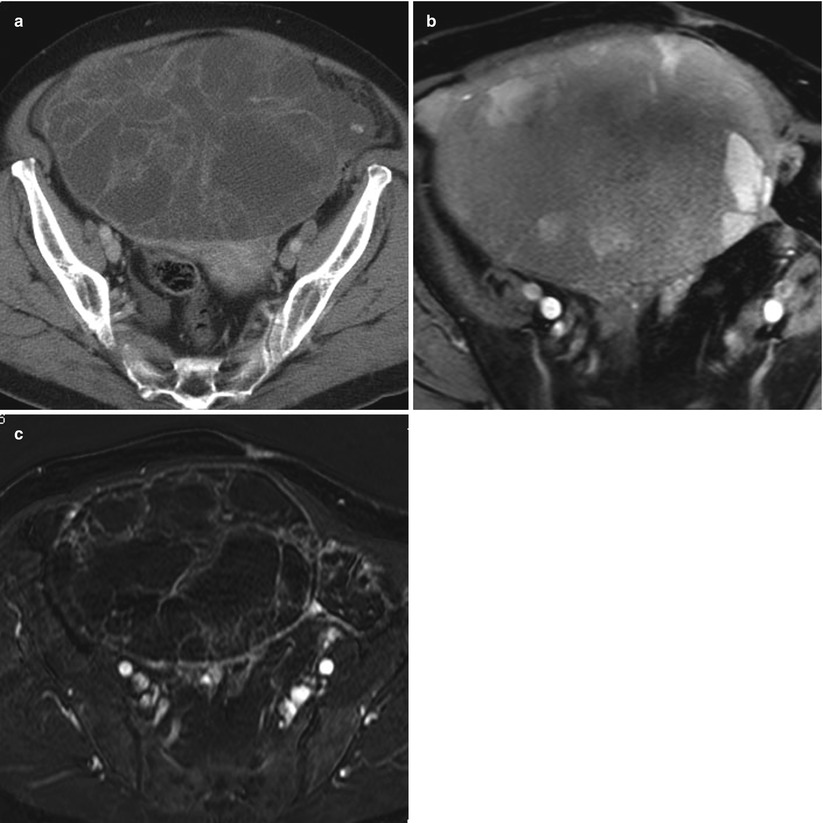
Fig. 9
(a) A 76-year-old woman with mucinous borderline tumor of intestinal type. Contrast-enhanced computed tomographic (CT) scan shows a large multilocular cystic mass with smooth contour, honeycomb appearance, and heterogeneous attenuation in the locules. Some septa are thickened. (b) Axial fat-saturated contrast-enhanced T1-weighted magnetic resonance (MR) image shows a large multilocular mass with heterogeneous high signal intensity but with variable signal intensity in the locules. Some septa are thickened. (c) Axial 3-dimensional (3D) fat-saturated contrast-enhanced T1-weighted MR subtraction image shows a large multilocular mass and several small solid components
Diagnosis of serous ovarian tumors on CT requires the detection of psammomatous calcifications. Mucinous cystic ovarian tumors that contain mucinous borderline tumors can also contain calcifications, but they differ from psammomatous calcifications and appear as curved lines in the cystic wall of ovarian tumors (Fig. 10a, b) [26].
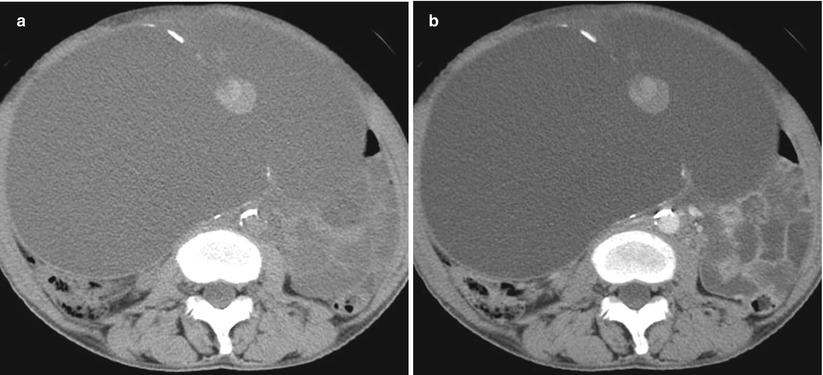
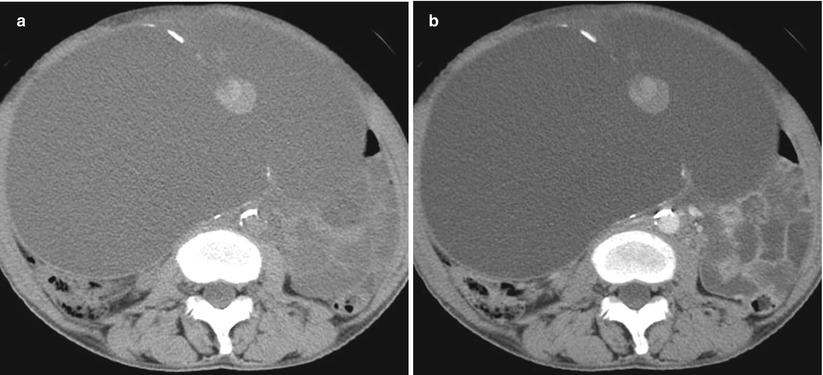
Fig. 10
(a) A 61-year-old woman with mucinous borderline tumor of intestinal type. Non-contrast axial computed tomographic (CT) scan shows a linear curve-shaped calcification in the cyst wall and septum. A mucinous component is seen along the septum. (b) Contrast contrast-enhanced CT scan shows linear curve-shaped calcification in the cyst wall and septum. A mucinous component along the septum shows no enhancement
Differential Diagnosis of Intestinal Type Mucinous Borderline Tumor
The MR findings of intestinal type mucinous borderline tumors herein identified resemble those reported for mucinous cystadenoma and mucinous carcinoma. Mucinous cystadenoma consists of a few solid components and mucinous carcinoma of many solid components that show strong contrast enhancement [8]. MR imaging findings of a solid component in the tumor generally suggest primary malignant ovarian epithelial tumor. Furthermore, mucinous cystadenocarcinomas or mucinous borderline ovarian tumors tend to show numerous fine loculi in larger numbers than in mucinous cystadenoma. Some mucinous borderline ovarian tumors appear as multilocular cystic masses with large solid components that result from the accumulation of small cystic components that contain mucinous fluid (Fig. 11a–d) [27]. MR findings overlap considerably between intestinal type mucinous borderline tumor and mucinous adenocarcinoma.
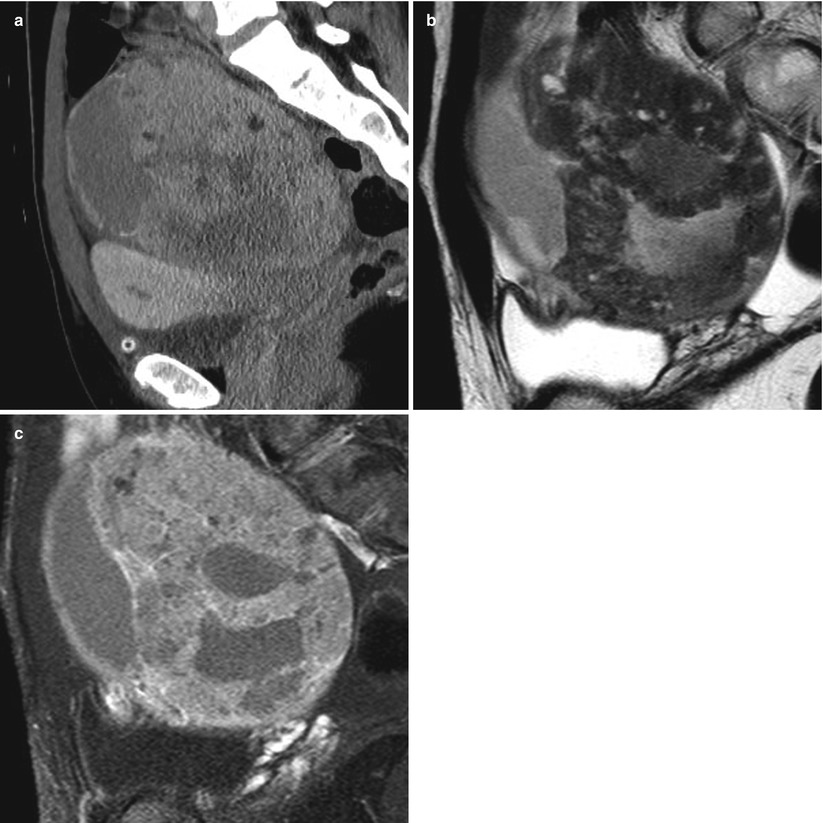
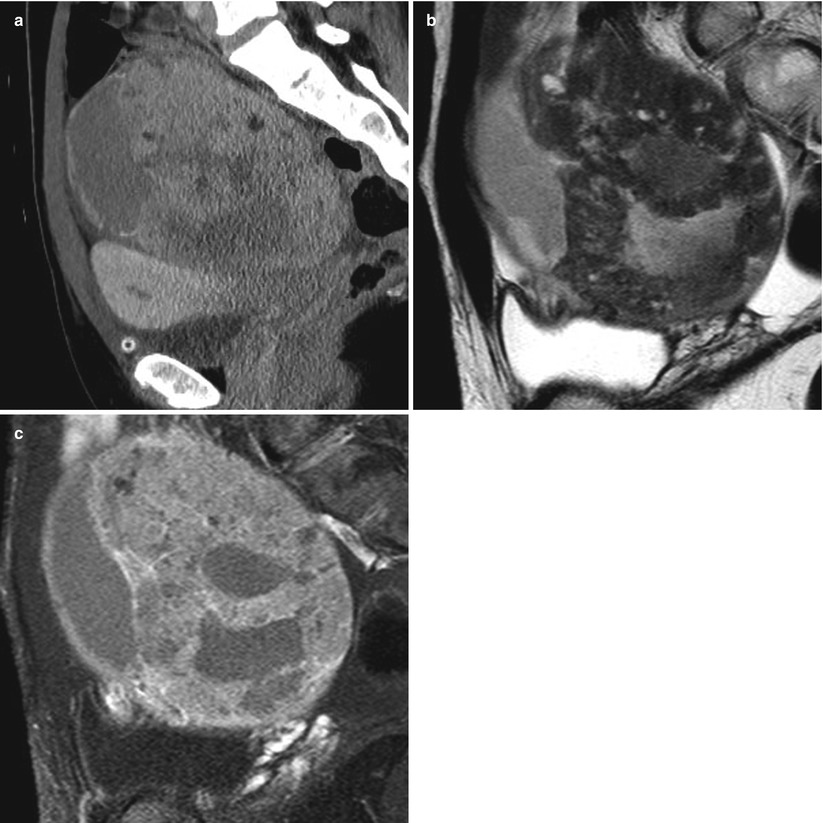
Fig. 11
(a) A 39-year-old woman with mucinous borderline tumor of intestinal type. Reconstruction image of contrast-enhanced computed tomographic (CT) scan shows a large solid mass with cystic parts in the pelvic space. (b) Sagittal T2-weighted magnetic resonance (MR) image shows the solid component of the mass with cystic parts. The signal of the solid component was slightly hypointense and contained markedly small areas of hyperintensity. (c) Sagittal fat-saturated contrast-enhanced T1-weighted MR image shows heterogeneous enhancement of the tumor in the solid component
Differentiating borderline mucinous tumor and ovarian metastasis from gastrointestinal tumor can be difficult. Ovarian metastasis sometimes demonstrates a stained-glass pattern on T1– and T2-weighted images, and the solid components are small in size. When both ovaries demonstrate multilocular cystic masses and mucinous tumor is suspected, gastrointestinal study or evaluation of tumor marker is necessary [28].
The imaging findings of mucinous borderline ovarian tumor are indistinguishable from other borderline ovarian tumors, such as serous, endometrioid, clear cell, and transitional cell tumors, except for the serous surface papillary borderline tumor. However, MR spectroscopy has recently been reported useful for differentiating mucinous and nonmucinous tumors. Takeuchi and colleagues showed a peak of N-acetylmucinous compounds of 2 ppm in mucinous tumors on MR spectroscopy [29]. The peaks of these compounds on MR spectroscopy could help distinguish mucinous and nonmucinous tumors for more reliable diagnosis of borderline tumors.
Focus Points
On MR imaging, mucinous borderline ovarian tumors commonly appear as multilocular cystic masses with numerous septa and contain fluids of different signal intensities, but they can contain a large solid component that results from the accumulation of small cystic components that contain mucinous fluid.
Müllerian Type Mucinous Borderline Tumor
General Considerations for Müllerian Mucinous Borderline Tumor
Rutgers and Scully described müllerian type mucinous borderline tumor in 1988 [30]. These tumors manifest at a younger age than intestinal type tumors. The average tumor diameter is 9 cm, and about 70 % are unilocular or have only a few locules. Most tumors show grossly visible intracystic papillae. Approximately 30 % are bilateral at diagnosis. The tumors coexist with ovarian or pelvic endometriosis in 20–30 % of cases as do several types of malignant ovarian tumors that arise from endometriotic cysts [30]; few other borderline tumors coexist with endometriosis. Müllerian mucinous borderline ovarian tumors do not coexist with pseudomyxoma peritone. The tumors somewhat mimic serous borderline ovarian tumors and are also termed “seromucinous borderline ovarian tumors.” These tumors may be associated with abdominal or pelvic implants, which may be invasive.
Imaging Findings of Müllerian Mucinous Borderline Tumor
Clues to müllerian mucinous borderline ovarian tumors may be bilaterality and association with endometriosis. The tumors are typically uni- or paucilocular cystic masses with mural nodules (Fig. 12a–d). The fluid component shows high intensity on both T1– and T2-weighted images, and the mural nodule shows prominent high intensity on T2-weighted images (Fig. 12b, c) [30] that reflects stromal edema. The fluid component may show high signal intensity on both T2– and T1-weighted image that results from intraluminal mucinous material.


Fig. 12
(a) A 34-year-old woman with mucinous borderline tumor of endocervical type. Contrast-enhanced axial computed tomographic (CT) scan shows a large cystic mass anterior to the uterus in the pelvic space (black arrow). A solid part in the cystic lesion is unclear. Normal functional cyst is seen in the right adnexal region (white arrow). (b) Axial fat-saturated T1-weighted image shows a large cystic mass anterior to the uterus in the pelvic space. A solid part in the cystic lesion is seen in the left frontal region. The fluid shows high signal intensity that reflects hemorrhage. (c) Sagittal T2-weighted image shows a large cystic mass anterior to the uterus in the pelvic space. Solid parts in the cystic lesion are seen as areas of high signal intensity along the cystic wall, and thickening of the cystic wall appears with low signal intensity. These changes may reflect changes from endometriosis. (d) Sagittal fat-saturated contrast-enhanced T1-weighted image shows a large cystic mass anterior to the uterus in the pelvic space. A solid part in the cystic lesion is seen in the left frontal region and shows high signal intensity
Differential Diagnosis of Müllerian Mucinous Borderline Tumor
MR findings of the müllerian mucinous borderline tumors identified herein resemble those reported for malignant tumors associated with endometrial cyst, such as clear cell or endometrioid carcinomas. These malignant tumors that arise from endometriotic cysts are frequently present as cystic masses filled with fluid of high signal intensity and nodular solid components [28]. However, differentiation of müllerian mucinous borderline tumors and malignant tumors associated with endometrial cyst is important because the prognosis of patients with the müllerian type is much better. Though definitive diagnosis may be difficult, T2-weighted image findings of prominently high signal intensity of mural nodules mingled with a layer of higher signal intensity around the nodules may suggest a more probable diagnosis of Müllerian mucinous borderline tumor (Fig. 13a–c) [31].