US is primary TIPS surveillance tool
CTA or MRA indicated if US is technically compromised or equivocal
•
Inferior vena cava occlusion
•
Stenosis is usually secondary to intimal fibroplasia within hepatic vein or TIPS itself
•
Associated abnormalities
Hepatic encephalopathy as portal flow bypasses liver
•
Maintaining TIPS patency is the major problem
•
Consider TIPS malfunction if shunt velocity is < 90 cm/s or portal vein velocity is < 35 cm/s
•
Image interpretation pearls
Low flow is difficult to detect with US
Confirm occlusion angiographically (CTA, MRA, DSA)
•
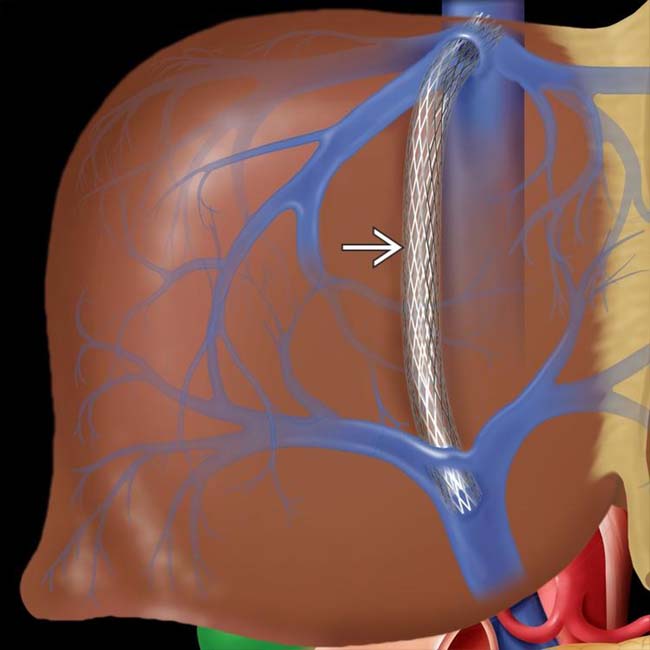
Transjugular intrahepatic portocaval shunt (TIPS)
•
Shunt between main portal vein (PV) and hepatic vein (HV) created with balloon-expandable metallic stent
•
Hepatopetal blood flow: Toward liver
•
Hepatofugal blood flow: Away from liver
•
Location
Most common route: Right HV → right PV → main PV
•
Size
10-12 mm in diameter
•
Morphology
Typically follows curved course through hepatic parenchyma
Portal end slightly proximal to main PV bifurcation
Hepatic end located at, or slightly cephalad to, junction of HV and inferior vena cava (IVC)
•
Grayscale ultrasound
Echogenic stent easily seen on grayscale images but does not block sound transmission
–
Fabric-covered stent may cause acoustic shadowing soon after placement
Probably due to gas bubbles trapped in fabric
May preclude US evaluation of TIPS patency for a few days
Usually resolves, allowing subsequent US surveillance for TIPS stenosis
Stent is typically curved but not kinked
Normally uniform stent caliber
Hepatic and portal ends “squarely” within veins (best seen on grayscale US)
•
Pulsed Doppler
Portal vein, satisfactory function
–
Hepatopetal flow toward heart
–
Flow toward shunt in right and left portal branches (occasionally away in left branch)
Shunt malfunction
–
Hepatofugal or bidirectional flow within TIPS
–
Peak velocity in portal vein < 35 cm/s
–
Flow away from shunt (hepatopetal) in right and left portal branches
Within shunt, satisfactory function
–
Flow slightly turbulent, slight pulsatility, possible slight respiratory variation
–
Peak velocity at any location, at least 90 cm/s
–
Similar velocity throughout shunt; not > 50 cm/s point-to-point variation
–
Similar velocity temporally; not > 50 cm/s change, study-to-study
Within shunt, malfunction
–
Continuous flow (no pulsatility or respiratory change)
–
Shunt velocity < 90 or > 250 cm/s at any point
–
Temporal drop in velocity ≥ 50 cm/s
–
Point-to-point increase in velocity ≥ 50 cm/s indicates focal stenosis
–
Focal severe turbulence (post stenosis)
–
Absence of flow: Occlusion
Always confirm angiographically
•
Color Doppler
PV/splenic vein (SV), satisfactory function
–
Widely patent, with hepatopetal flow
–
Flow toward shunt in right and left portal branches (occasionally away in left branch)
Within shunt, satisfactory function
–
Color flow extends to stent margins
–
Uniform, velocity (color scale) throughout shunt
Within shunt, malfunction
–
Visible stenosis, focal or diffuse
–
Focal color change indicates high velocity
–
Focal severe flow disturbance (post stenosis)
–
Absence of flow: Occlusion
Check with spectral Doppler (more sensitive); always confirm angiographically
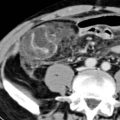
 extends to the right portal vein, adjacent to its junction with the main portal vein.
extends to the right portal vein, adjacent to its junction with the main portal vein.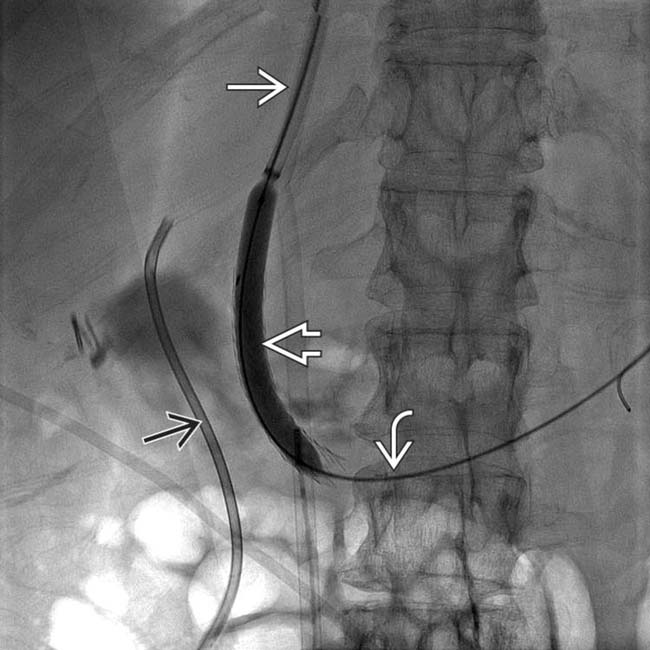
 proceeding down the IVC, then penetrating the liver parenchyma to enter the portal vein
proceeding down the IVC, then penetrating the liver parenchyma to enter the portal vein  . The intraparenchymal tract is dilated with a balloon
. The intraparenchymal tract is dilated with a balloon  . Incidentally noted is a plastic biliary stent
. Incidentally noted is a plastic biliary stent  .
.
 deployed with its distal end in the hepatic vein
deployed with its distal end in the hepatic vein  and its proximal end in the main portal vein
and its proximal end in the main portal vein  .
.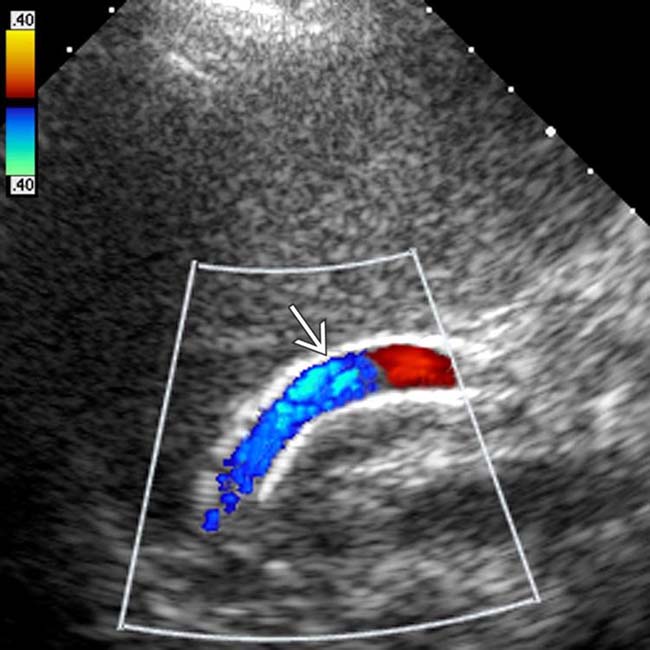
 . Although the stent is highly echogenic, it does not obstruct sonographic visualization. Color Doppler indicates brisk flow toward the heart, the expected finding.
. Although the stent is highly echogenic, it does not obstruct sonographic visualization. Color Doppler indicates brisk flow toward the heart, the expected finding.