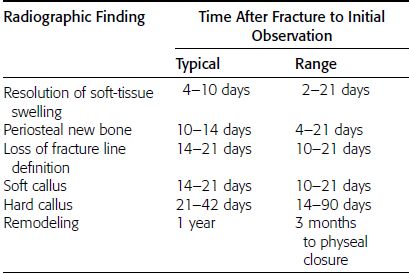
CHAPTER 5 Fractures in children are not the same as fractures in adults because of differences in anatomy, biomechanics, and exposure to trauma. The incidence, type, and age distribution of children’s fractures vary across countries and regions because of cultural and environmental differences. Fractures in children are first seen at childbirth, from birth trauma. They become more prevalent with walking (and falling) in toddlers and peak in incidence in girls at approximately 11 years of age and in boys at approximately 14 years of age. By 16 years of age, 42% of boys and 27% of girls will have sustained at least one fracture. In the United States, most fractures in children are the result of accidents while playing and sports-related injuries. Fractures are more common in boys than in girls by a ratio of nearly 2:1. The upper extremity is fractured more commonly than the lower extremity, and the left upper extremity is fractured more frequently than the right. After the first year of life, trauma is the leading cause of death in children, accounting for 50% of all deaths in children between 1 and 14 years of age. As with fractures, boys are at greater risk of dying from trauma than girls. Most trauma deaths in children are the result of head injuries. The immature, growing skeleton has cartilaginous growth plates, cartilaginous epiphyses, and a thick, strong periosteum. Immature bone is more porous than adult bone and functions less as a single mechanical unit and more as an aggregate of smaller units. Children’s bone is less stiff and more malleable (ductile) than adult bone. Fracture lines do not propagate as far, and a loaded bone is more likely to bend and deform than to break and splinter. There are five general types of children’s fractures: buckle fractures, plastic deformation, greenstick fractures, complete fractures, and growth plate fractures. Cortical bone in children can fail under compressive as well as tensile loading. Failure of bone under compressive loading results in a buckle fracture. Buckle fractures (also called torus fractures) are incomplete impaction fractures in which the cortex around all or part of the circumference of the bone is buckled (Fig. 5.1). They occur at the metaphysis, where the porosity of the bone is greatest, and are most common in preschool-aged children. On radiographs, buckle fractures can be recognized by a focal, angular protrusion of the cortex with a modest angulation of the shaft and overlying soft-tissue swelling. FIGURE 5.1. Buckle fracture (arrows) of the distal radial metaphysis. A: Lateral radiograph; B: PA radiograph. With angular loading, elastic and then plastic bowing occurs (see Fig. 5.15). Traumatic plastic bowing results in a permanent bend caused by a series of microscopic shear fractures on the concave aspect without gross disruption of the cortex or trabeculae. Elastic recoil allows a bent bone to recover part of its normal shape. Plastic bowing is most often seen at the ulna, in association with fractures of the radius, and at the fibula, in association with fractures of the tibia. On radiographs, plastic bowing may be recognized by an abnormal bend in the affected bone. When a bone is angulated beyond the limits of bowing, the convex side fails in tension and the concave side bends, resulting in an angulated, incomplete transverse fracture. Such a fracture is called a greenstick fracture (see Fig. 5.15). Elastic recoil usually decreases the degree of angulation; muscle pull may increase it. The periosteum is intact on the concave side of the bend but not on the convex side, leaving a periosteal hinge. Greenstick fractures are seen most often in children of elementary school age. The only anatomic sites where greenstick fractures are common are the shafts of the radius and ulna. On radiographs, greenstick fractures may be recognized by the bowing deformity of the affected bone with a transverse fracture extending through the cortex on the convex side of the bow. Complete fractures through the bone in children resemble adult fractures. However, the displacement of complete fractures depends on whether or not the periosteum is torn. A periosteal hinge usually is present on one side, allowing angulation but not much displacement. Children’s fractures are rarely comminuted. As with adult bones, the direction of loading determines the configuration of the fracture line. The cartilage of the growth plate absorbs and dissipates some of the energy of loading, reducing the likelihood of a fracture. The growth plate is attached to the metaphysis internally by the interdigitation of the bone with the zone of calcified cartilage and externally by the periosteum. The growth plate is relatively weak compared with the capsule and ligaments of adjacent joints, and mechanisms of injury that tend to result in ligamentous joint injuries in adults typically result in growth plate fractures in children. The growth plate is particularly vulnerable to injury when loaded in torsion or shear but is relatively resistant to tension and compression. When the epiphysis is separated from the metaphysis, the plane of separation through the growth plate is in the zone of cartilage transformation between the calcified and uncalcified layers of cartilage, leaving the germinal cell layers with the epiphysis and the calcified cartilage with the metaphysis. Displacement does not occur unless the periosteum is also torn. Injuries to the growth plate represent approximately one third of skeletal injuries in children. The most common sites of growth plate fractures are the wrist and ankle. Growth plate fractures are more common in boys than in girls. The peak incidence in boys is at 14 years of age, but the peak incidence in girls is at 11 and 12 years of age. The difference can be accounted for by the differences in the rate of skeletal maturation between boys and girls. Sometimes, a normal growth plate may be mistaken for a fracture. Keats and Smith’s Atlas of Normal Developmental Roentgen Anatomy is a handy reference for reviewing the radiologic appearance of the skeleton at various ages; in some circumstances, it may be necessary to radiograph the contralateral body part for comparison. Salter and Harris described five types of growth plate fractures (Fig. 5.2). Their classification should be used in describing fractures of the growth plate. The most common type of growth plate fracture is a Salter type II fracture. There are many other systems of classifying growth plate injuries of varying complexity, but the Salter-Harris system is universally understood. FIGURE 5.2. Salter-Harris classification of fractures of the growth plate. A Salter type I fracture extends through the growth plate without involving the bone (Fig. 5.3). This type is usually caused by shearing, torsion, or avulsion. Because Salter type I fractures do not displace unless the periosteum is torn, they may be difficult to demonstrate radiologically without stress views. The most common sites of Salter type I fractures are the lateral malleolus of the ankle and the distal radius. FIGURE 5.3. Salter type I fracture of the distal radius. The radial growth plate appears wide (arrow) compared with that of the ulna. In Salter type II fractures, the plane of the fracture passes through much of the growth plate but includes a piece of metaphyseal bone on one side (Fig. 5.4). The periosteum is intact on the side with the metaphyseal fragment but torn on the opposite side. The most common sites of Salter type II fractures are the phalanges of the fingers and the distal radius. FIGURE 5.4. Salter type II fracture of the distal phalanx. A: Lateral view shows the fracture passing through the growth plate (arrow) and including a small piece of the metaphysis (arrowhead). B: The PA view shows widening of the growth plate (arrows). Salter type III fractures include a piece of the epiphysis and are intra-articular. Salter type III fractures are most common when the growth plate is partially closed, so they tend to occur in teenagers. Most Salter type III fractures are avulsion fractures that occur at sites of ligamentous or tendinous attachment. The most common sites of Salter type III fractures are the phalanges of the fingers and thumb (Fig. 5.5) and the medial malleolus of the ankle. FIGURE 5.5. Salter type III fracture of the distal femur. A: AP radiograph shows fracture (arrow) through the intercondylar portion of the epiphysis. B: Oblique radiograph shows widening (arrow) of the lateral femoral growth plate. Salter type IV fractures involve both metaphysis and epiphysis and are intra-articular. The most common sites of Salter type IV fractures are the lateral condyle of the elbow and the medial malleolus of the ankle (Fig. 5.6). Because displacement of the fracture fragment is likely to result in premature closure of the growth plate, Salter type IV fractures have a worse prognosis than Salter type I or II fractures. Open reduction and internal fixation may be required for the treatment of these fractures. FIGURE 5.6. Salter type IV fracture of distal femoral growth plate. Intercondylar fracture lines extend through the metaphysis, physis, and epiphysis. A Salter type V injury is a crush injury of the growth plate from axial loading. These injuries are exceedingly rare and are absent from many large series of growth plate fractures. Almost by definition, these injuries may not be recognized until the cessation of growth is noticed (Fig. 5.7). FIGURE 5.7. Salter type V fracture of the distal tibial growth plate. A: Lateral ankle radiograph 1 year after injury shows a growth deformity (arrow). B: Coronal proton density fat suppressed MR imaging shows the prematurely closed portion of the growth plate (arrow). The growth plate is surrounded by a perichondrial ring that appears to regulate its diameter. Displacement of the perichondrial ring allows growth away from the plate laterally, resulting in a posttraumatic osteochondroma (see Chapter 9). Removal of a segment of the ring, for example, by a lawn mower blade injury, permits a bony bridge (physeal bar) to develop across the growth plate, tethering it and leading to angular deformity as growth proceeds (Fig. 5.8). FIGURE 5.8. Coronal CT of proximal tibia shows physeal bar (arrow) caused by a boat propeller injury of the proximal tibial growth plate. Asymmetric growth with angular deformity has resulted. Fractures of the epiphysis in children without involvement of the growth plate may occur as osteochondral fractures or avulsion fractures (Fig. 5.9). When the fractures involve only the cartilage, they may be unrecognized. These injuries were not included in the original Salter-Harris classification. FIGURE 5.9. Tibial epiphyseal fracture (arrow). Apophyses are bony prominences that typically accept traction from an attached tendon or muscle, and fractures involving apophyses are almost always avulsion fractures. Fractures of the apophyses are Salter type I or III injuries. Common sites for apophyseal avulsion injuries include, in the upper extremity, the medial epicondyle, the olecronon process, the coronoid process, and the coracoid process, and in the lower extremity, the anterior tibial tubercle, the femoral trochanters, and the calcaneus. There are multiple sites around the pelvis that may be avulsed. Open fractures in children are typically the result of accidents, many of which are preventable (Fig. 5.10). Open fractures account for approximately 3% of fractures in children. On radiographs, open fractures may be recognized by the presence of gas within the fracture site, a soft-tissue wound extending to the fracture site, protrusion of bone through the soft tissues, missing fragments of bone, or penetration of foreign bodies to the bone. FIGURE 5.10. Lawnmower accident in a child with open fractures (arrows) of the lateral foot. Fracture healing in children is rapid (Table 5.1). The younger the child and the greater the remaining growth potential of the fractured bone, the faster and more complete are the healing and remodeling. Fracture remodeling is a process of bone resorption and periosteal deposition. Fracture remodeling can round off protruding edges by bone resorption and fill in concavities by periosteal new bone. However, varus, valgus, and rotary misalignments do not improve by this process (Fig. 5.11). As growth proceeds and the bone enlarges, asymmetric activity at the growth plate and at the periosteum may tend to correct angular misalignment. Hyperemia from fracture healing may lead to overgrowth, so that a reduction may be left intentionally shorter than anatomic in anticipation of overgrowth. Nonunion of children’s fractures is rare unless the fractures are intra-articular. Most fractures in children are treated by closed means, but open reduction and internal fixation by pins, wires, plates, screws, and rods are sometimes necessary. TABLE 5.1 Radiographic Timetable of Fracture Healing in Children Source: Kleinman PK. Diagnostic Imaging of Child Abuse. 2nd Ed. St. Louis, MO: Mosby–Year Book; 1998. FIGURE 5.11. Healing spiral femoral shaft fracture. A: Acute fracture. B: Follow-up after 8 weeks. In fractures of the growth plate, the production of growing cartilage may not be interrupted by the fracture if the blood supply to the separated epiphysis remains intact. After a fracture, the growth plate becomes wider until the normal zone of cartilage transformation is reestablished and then the plate returns to normal (Fig. 5.12). The healing process for Salter I and II fractures is much more rapid than that of a fracture through bone and may leave no scar. FIGURE 5.12. Healing distal radius growth plate fracture (Salter type I) with widening and irregularity of the zone of provisional calcification (arrow). Bruises and contusions are common in children and usually are inconsequential. Bruises around the head and neck or chest and abdomen may suggest more severe underlying injuries of the central nervous system or viscera, respectively. Unexplained multiple bruises of different ages may suggest child abuse. Because a child’s bones and growth plates are usually weaker than the tendons and ligaments, strains and sprains in children are uncommon until adolescence, when adult patterns of injury begin to emerge as the growth plates close. Fractures of the hand account for approximately 20% of all fractures of the extremities in children. The most common fractures in the hand are crush injuries of the distal phalanx and growth plate fractures of the proximal phalanx. The index and little fingers are the most likely to be fractured. Distal phalanges are most commonly injured by closing doors and falling objects. These are generally extra-articular fractures that do not involve the growth plate and may have a transverse, longitudinal, or comminuted morphology. Forced flexion may result in fractures of the distal phalanx that involve the growth plate. Because the extensor tendon inserts at the epiphysis of the distal phalanx, and the flexor digitorum profundus tendon inserts along the metaphysis, these fractures may become angulated or displaced and assume a fixed position in flexion (mallet finger equivalent). These mallet finger–equivalent injuries may represent Salter type I or II fractures with displacement or angulation at the fracture site or Salter type III or IV fractures with retraction of the fragment by the extensor tendon and unopposed flexion by the flexor digitorum profundus. In young children, proximal phalangeal fractures are typically Salter type I or II fractures. In adolescents, Salter type III fractures occur with avulsion of a portion of the articular surface by an attached tendon or ligament. Such fractures occur commonly at the thumb and are the children’s equivalent of a gamekeeper’s fracture (Fig. 5.13). Salter type III avulsion fractures may also occur at other phalanges of the fingers. FIGURE 5.13. Salter 3 fracture (arrow) at the base of the proximal phalanx of the thumb (gamekeeper’s fracture). The most common metacarpal fracture in children is the boxer’s fracture, a volarly angulated fracture of the fifth (or sometimes fourth) metacarpal neck. Fractures and dislocations involving the carpal bones are rare in children. A fracture of the scaphoid is the most common of these rare injuries. Similar to the fractures in adults, fractures across the scaphoid waist may lead to osteonecrosis of the proximal pole. Ligamentous injuries of the wrist in children are rarer than fractures of the carpal bones. Fractures of the distal radius account for approximately 23% of all fractures of the extremities in children, making it the most common site of children’s fractures. These injuries are most commonly sustained in falls onto an outstretched, dorsiflexed hand. The severity of the fracture depends on the energy involved in the fall, ranging from gravity falls from standing height, to falls in which the body has significant momentum (e.g., in roller skating), to falls from a great height. Simple buckle fractures are common in preschool-aged children with simple gravity falls (see Fig. 5.1). Buckle fractures are usually located 2 to 3cm proximal to the growth plate. Complete fractures are seen in higher-energy injuries. When displaced, the fragments are most often displaced dorsally, resulting in a bayonet deformity. The distal radius is the most common location for growth plate fractures in children. These are most often Salter type I or II fractures (Fig. 5.14), and the epiphysis may be displaced. FIGURE 5.14. Displaced Salter II fracture of the distal radius. Injuries to shafts of the radius and ulna may be plastic bowing deformities, greenstick fractures, or complete fractures (Fig. 5.15), depending on the magnitude and direction of loading and the maturity of the patient. Rotational deformity is usually present and evident as angulated fractures of both bones at different levels. Because the radius has a normal bowing curve and a pear-shaped cross section, interruption of the smooth curve of the radius or an apparent change in shaft diameter across the fracture site indicates radial malrotation. The bicipital tuberosity may serve as a guide to the rotation of the proximal radius. The position of the proximal fragments in complete fractures depends on the direction of muscle pull. FIGURE 5.15. Forearm fractures. A: Complete fracture (arrow) of the radius with plastic bowing deformity (arrowheads) of the ulna. B: Greenstick fractures of the radius and ulna. C: Complete fractures of both the radius and ulna.
Trauma in Children
 EPIDEMIOLOGY
EPIDEMIOLOGY
 BIOMECHANICS
BIOMECHANICS


 GROWTH PLATE INJURIES
GROWTH PLATE INJURIES





 OPEN FRACTURES
OPEN FRACTURES
 FRACTURE HEALING AND TREATMENT
FRACTURE HEALING AND TREATMENT



 SOFT-TISSUE INJURIES
SOFT-TISSUE INJURIES
 HAND AND FOREARM
HAND AND FOREARM





Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree