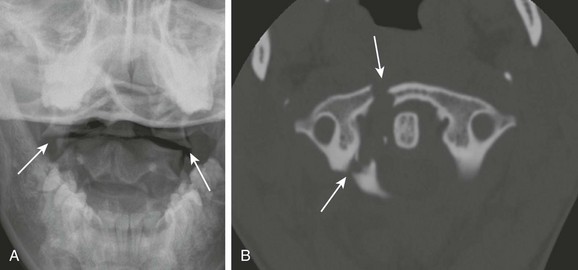
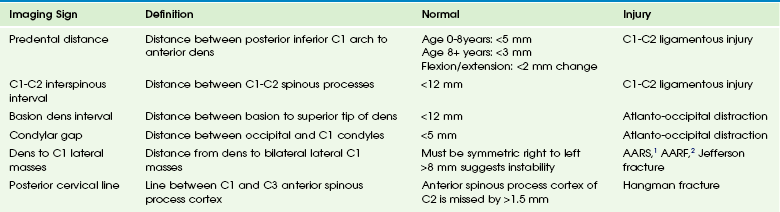
Chapter 47 Mortality of spine-related trauma in children is higher than in adults and is estimated at 25% to 32%.1 Fortunately, children with incomplete neurologic lesions fare better compared with adults, with up to 90% having partial recovery and 60% having full recovery.1,2 Motor vehicle accidents (MVAs), followed by falls and sports injuries, are the most common causes of pediatric spinal trauma. Young athletes are at higher risk for developing stress-related injuries than are adult athletes.3 Gunshot injuries accounted for 22% of injuries in one study of 277 pediatric patients with spinal trauma.4 Congenital spine anomalies such as os odontoideum, block vertebrae, Klippel-Feil syndrome, and Down syndrome increase the risk of cervical spinal injury. Nerve root avulsion with pseudomeningocele formation may result from birth trauma, MVAs, or less often, penetrating injury (Fig. 47-1).5 Figure 47-1 Avulsed nerve roots in a 13-year-old girl unable to use her left arm after an all-terrain vehicle accident. Younger children are more susceptible to upper cervical injuries compared with adults because of their relatively large-sized, heavy craniums and weaker neck muscles.6 This anatomy causes a more cranial fulcrum of movement at C2-C3 in younger children versus C5-C6 in older children and adults.1 Injuries in younger children, especially those under 8 years, differ from those in older children. Because of greater mobility and laxity of ligaments in the cervical spine of younger children, they tend to have higher cervical injuries (occiput to C3). These injuries are more likely associated with a neurologic deficit and to extend through synchondroses.7 The unique biomechanical properties of young children, including their large-sized heads and higher fulcrum of motion, causes increased occurrence of spinal cord injury without radiographic abnormality (SCIWORA). The acronym SCIWORA was popularized in the early 1980s to describe children with clinical symptoms of cervical cord trauma and normal radiographs.8 With the introduction of magnetic resonance imaging (MRI), injuries in children with SCIWORA could be visualized and the general prognosis predicted on the basis of the findings.9,10 MRI allows for the diagnosis of SCIWORA by easily showing the findings of cord contusion, including hypointensity on T1-weighted imaging and hyperintensity on T2-weighted imaging, cord hemorrhage, or cord transaction (Fig. 47-2).11 The presence of normal cord signal suggests the child will make a complete recovery, whereas intramedullary hemorrhage and transection portend a poor prognosis.8 Figure 47-2 Spinal cord injury without radiographic abnormality (SCIWORA) in a 6-year-old boy with paraplegia after a fall from a horse and normal cervical spine radiographs. Because of their relatively small occipital condyles and more horizontal atlanto-occipital joint orientation, young children are at increased risk for atlanto-occipital disassociation.2,9,12 Devastating spinal cord injury often occurs, and many cases are fatal. A diagnosis is made by measuring a condylar gap greater than 5 mm (Kaufman condylar gap) or a basion to axis interval (BAI) of greater than 12 mm (Fig. 47-3).2 One pitfall is that in children younger than 13 years, the BAI is less reliable.12 Some helpful measurements to evaluate pediatric cervical spine trauma are listed in Table 47-1.13 Atlanto-occipital dissassociation requires urgent stabilization. Table 47-1 Cervical Spine Measurements Useful in Evaluation of Pediatric Trauma AARS, atlantoaxial rotatory subluxation; AARF, atlantoaxial rotatory fixation. Figure 47-3 Atlantoaxial disassociation in a 5-year-old unrestrained girl after a motor vehicle accident. Compression loading forces on the cervical spine can result in a C1 burst fracture, or Jefferson fracture. This injury is most common in adolescents from MVAs and diving accidents. Jefferson fractures show between one and four defects in the C1 ring. The fracture may be stable or unstable, depending on whether or not the transverse ligament is intact or ruptured, respectively. A single defect in the ring is typically stable, whereas three or four defects are typically unstable.9 A dens to C1 lateral mass distance of greater than 8 mm suggests instability. Forty percent of Jefferson fractures have an associated C2 fracture.12 Lateral cervical spine radiographs are of little value, and the diagnosis is made on the open-mouth odontoid view by showing offset of the lateral masses of C1 on C2 (Fig. 47-4).13 Pitfalls to avoid include rotation of the head on the open-mouth view that may cause the lateral mass to appear slightly laterally displaced, hypermobility in young children that may lead to minimal normal lateral displacement of C1 on C2 and finally, the normal developmental bilateral offset of the C1 lateral masses that may occur in children under 2 years of age because of the differential growth of C1 versus C2.9
Trauma
Etiology
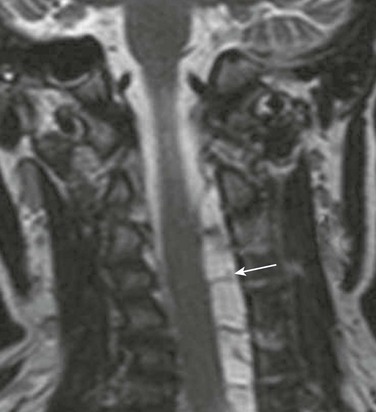
A coronal T2-weighted magnetic resonance image shows an extensive intradural cerebral spinal fluid collection (arrow) shifting the spinal cord (C) to the right due to C2 to T1 nerve root avulsions.
SCIWORA
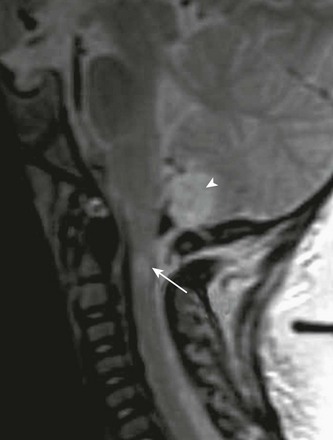
Sagittal magnetic resonance image of the craniocervical junction reveals hyperintense T2 contusions within the cervical spinal cord (arrow) and the inferior cervical vermis (arrowhead). Note T2 dark hemorrhage in the cerebral spinal fluid at the level of the foramen magnum just below the vermian contusion.
Atlanto-Occipital Disassociation

Lateral cervical spine radiograph demonstrates abnormally increased basion to dens distance of 15 mm (white line). The C1-C2 interspinous distance is also increased at greater than 12 mm (arrow).
Atlas or Jefferson Fracture
Radiology Key
Fastest Radiology Insight Engine