, Carlos Capuñay1, Carlos E. Sueldo2 and Juan Mariano Baronio3
(1)
Diagnóstico Maipú, Buenos Aires, Argentina
(2)
University of California, San Francisco, CA, USA
(3)
CEGYR, Buenos Aires, Argentina
Tubal factor is one of leading causes associated to infertility in women. There exist diverse pathological conditions that affect the Fallopian tubes and, henceforth, interfere with normal transport of the ovule through them. The most frequent process is pelvic inflammatory disease, which represents a wide spectrum that includes salpingitis, piosalpinx and the tube-ovary abscess. Other frequent entities, and some more rare, can compromise the Fallopian tubes. The differential diagnosis with other pelvic entities is of the utmost importance for treating the patients. There exist diverse diagnostic methods that are utilized in the study of uterine tubes. Hysterosalpingography is the modality which has traditionally been used to investigate the tuboperitoneal factor. Ultrasound and Magnetic Resonance Imaging (MRI) present limitations to the direct visualization of tubes. In the last years enhancements in these methods have been developed, like the sono-hysterosalpingography and the MR-hysterosalpingography, but they still have not reached an adequate resolution for the diagnosis of the tubal pathology. Laparoscopy is the method of reference and is reserved for the confirmation of the radiologic findings and for therapeutic procedures.
Virtual hysterosalpingography (VHSG) is a new diagnostic modality that utilizes a similar procedure as the conventional study based on computed tomography studies. Volumetric images of high spatial resolution are obtained through the opacification of the uterine cavity and Fallopian tubes, which allows achieving high quality images and virtual endoscopic navigation [1].
The increasing use of diagnostic imaging forces the familiarization with an extensive pathological process that affects uterine tubes. The knowledge of the diseases of uterine tubes and their appearance in images of normal and abnormal conditions is crucial for optimal diagnosis and treatment. In this chapter the anatomical fundaments will be presented, as well as the spectrum of typical and pathological findings in the uterine tubes and in VHSG studies.
Uterine Tubes Study
Hysterosalpingography is the study which has been utilized for the initial evaluation of patients with infertility. Besides offering a morphological assessment of uterine cavity, hysterosalpingography provides important information about the anatomy of the Fallopian tubes and tubal patency (Fig. 9.1). The distribution of contrast material into pelvic cavity can be documented and a possible peritoneal factor inferred indirectly. Nevertheless, the results for the diagnosis of the tubal occlusion (sensibility of 65 % and specificity of 83 %) are limited when compared with laparoscopy [2]. For this reason, other techniques were, and are, being constantly tested for the evaluation of the tubal patency. In routine ultrasound, Fallopian tubes cannot be visualized unless they are dilated or when a sufficient amount of fluid exists in the pelvic cavity that allows individualization within the wide ligament [3]. Another technique consists in carrying out a sonographic evaluation after an injection of saline solution into the pelvic cavity. In these cases, the tubal patency is not evaluated, but only tubal diameters. A modified technique is denominated sonohysterosalpingography, in which saline solution is injected through the cervical canal and distention of uterine cavity is under control by ultrasound [4, 5]. This technique does not allow the evaluation of the tubal anatomy. Nuclear medicine was also used in the assessment of tubal patency with radionuclide detection in the peritoneal cavity that had previously been placed at the end of the vagina. This technique is denominated nuclear hysterogram, which has limitations in the morphologic evaluation of the tubes and in the detection of unilateral tubal obstructions [6]. Recently, different experiences in the evaluation of uterine tubes with MRI were published [7–9]. Although the results are promising, limitations exist with regards to spatial resolution and, henceforth, in the complete visualization of tubes and intratubal anatomy. Definite diagnosis and treatment of tubal disease is carried out with surgical intervention either with a laparoscopy or a laparatomy. When combining the direct visualization of the tubes with the blue methylene injection via hysteroscopy, the patency is proven. The internal evaluation of tubes can be achieved by introduction of the laparoscope through a tiny incision done by the surgeon. In this way the fold and mucus pattern can be visualized, especially in the ampullar or dilated region of the tubes. This technique is called falloscopy. A complete internal visualization can also be accessed through the canulization of a microhysteroscope, known as a salpingography. In recent years, the selective salpingography guided by fluoroscopy was developed, an interventionist procedure for patients with proximal tubal occlusion [10]. The success rates of repermeabilization and visualization of the distal anatomy of the tube were of 76–95 %. However, reocclusion was observed in 15–30 % of the cases and there was a prevalence of 10 % of ectopic pregnancies after the procedure. All novel techniques described still require an adequate evaluation with large controlled and randomized studies in search of high levels of scientific evidence [11].
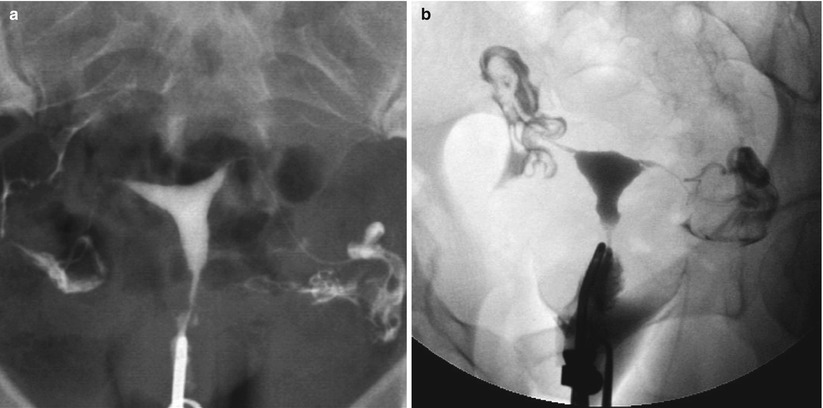
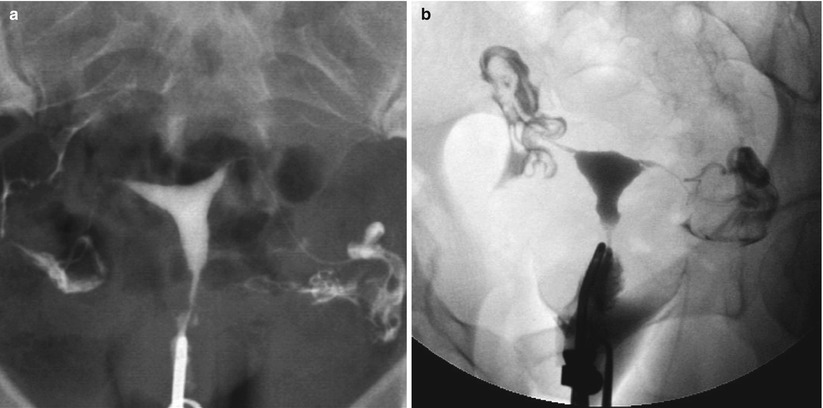
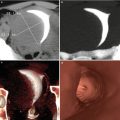
Fig. 9.1
(a) HSG showing the normal anatomy of the uterine tubes and the bilateral spillage of contrast into peritoneum. (b) HSG with inverted window, where the normal tubal morphology and patency are appreciated
Radiological Approach
Tubal pathology is classified from the radiological point of view in those that affect tubal visualization, caliber, filling defects and their morphology. Partial or absent tubal visualization may be due to a variety of technical factors or pathologic processes. Hence, this finding is nonspecific and can be related to an insufficient amount of contrast, cornual spasms or mucous plugs [12]. During the VHSG study, these circumstances are avoided with an adequate preparation of the patient and a protocol procedure [13]. The administration of oral antispasmodics an hour before the exam prevents cornual spasms and the presence of mucosal plugging within the tubes [14]. While employing a controlled administration of the contrast medium with an injector pump, the exact moment of the image acquisition is calculated, verifying a volume of contrast that is enough for the complete opacification of the uterine cavity and of the tubes. An excessive quantity would be non productive for the tubal visualization due to the fact that the contrast material poured into the peritoneal cavity could hide the tubes. Hence, the calculation of the moment of the image acquisition becomes of vital importance for the success of the study; it avoids rescan which means an increase in the radiation dose. Pathological obstructions can occur at any level. Inflammatory obstruction typically affects the ampullary portion (Fig. 9.2). On the other hand, when the occlusion is post-surgery (salpingectomy or tubal ligation), in general the visualization is partial and the obstruction is at the level os the isthmus (Fig. 9.3).
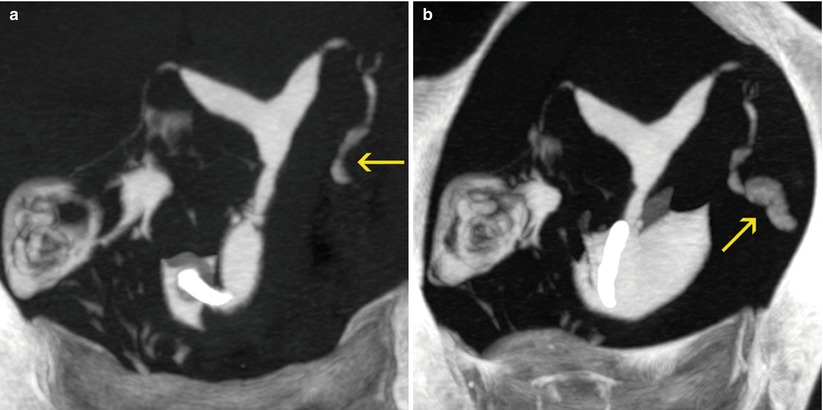
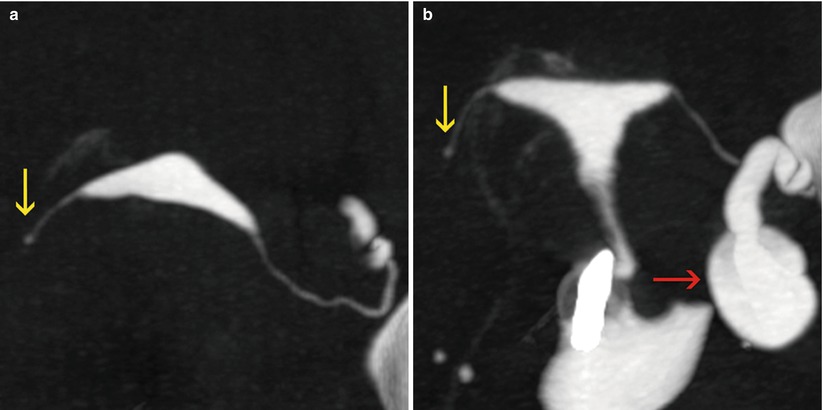
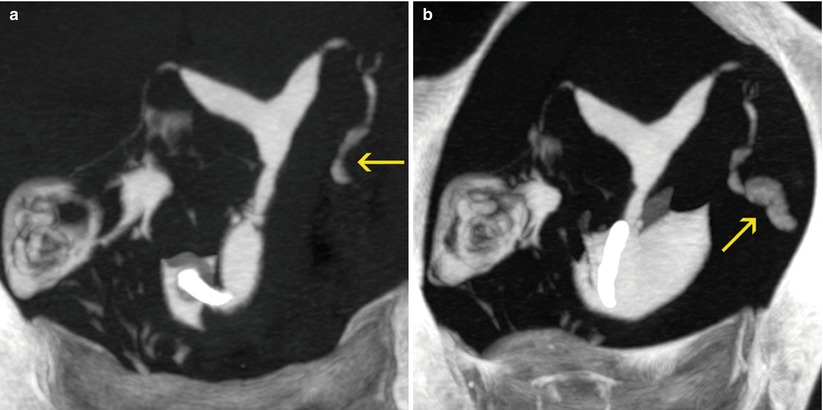
Fig. 9.2
Distal tubal obstruction. (a, b) Coronal oblique maximum intensity projection images showing absence of the contrast spillage into the peritoneal cavity through the left tube, which is opacified up to its distal portion (arrows)
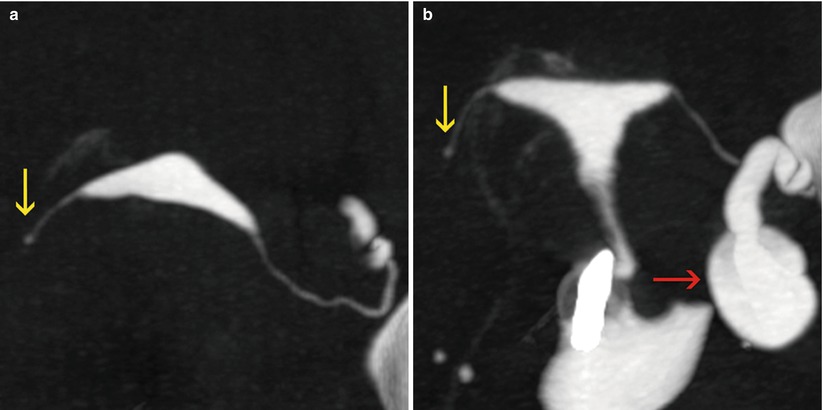
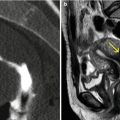
Fig. 9.3
Post-surgery tubal obstruction. (a, b) Axial and coronal maximum intensity projection images showing opacification of proximal portion of right uterine tube (yellow arrow), in a patient with a history of ectopic pregnancy and right salpingectomy. Note that the left tube is dilated (red arrow)
The tubal dilatations are due usually to inflammatory pelvic diseases or endometriosis (Fig. 9.4). Dilatation may be associated with complete obstruction (hydrosalpinx) or with some peritoneal spillage (Fig. 9.5).
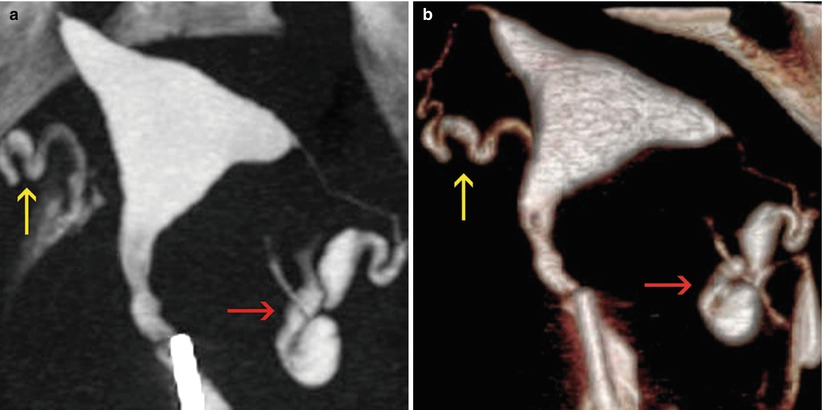
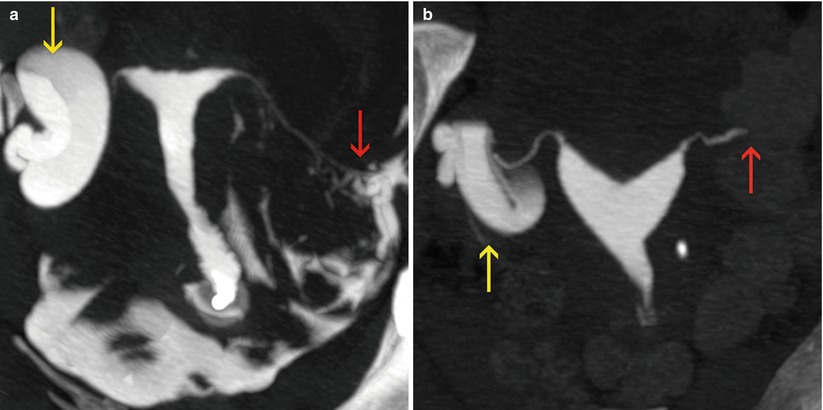
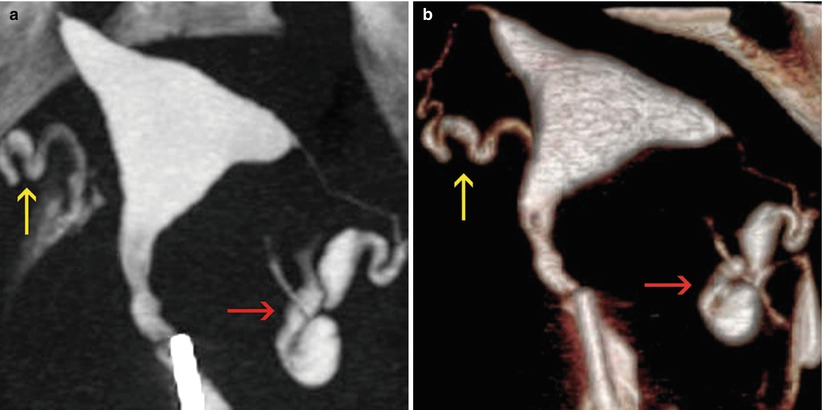
Fig. 9.4
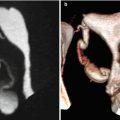
Tubal dilatation. Mild ampullary dilatation of the left uterine tube, with scarce passage of contrast into the peritoneal cavity (red arrow). The right tube is normal in caliber (yellow arrow). (a) Maximum intensity projection image. (b) 3D volume rendering image
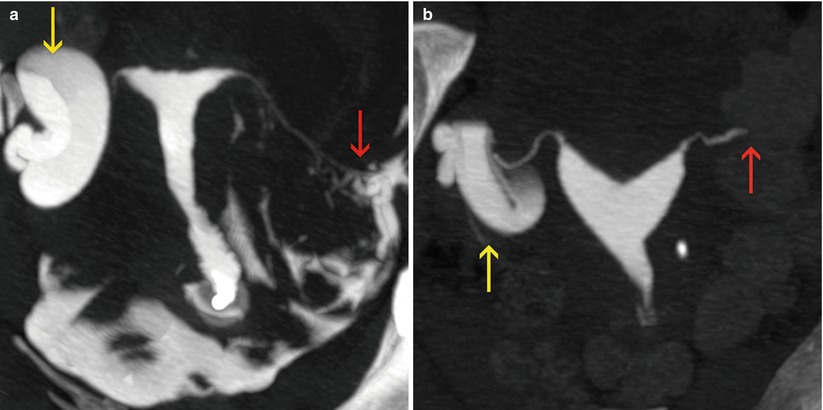
Fig. 9.5
Hydrosalpinx. (a) Maximum intensity projection image showing a severe dilatation of the right uterine tube (yellow arrow), without passage of contrast to the peritoneal cavity. On the other hand, the left tube is visualized with normal caliber and ample passage of contrast to the peritoneal cavity (red arrow). (b) Another case of right unilateral hydrosalpinx (yellow arrow). The left tube shows only opacification of the interstitial portion due to salpingectomy (red arrow)
The filling defects within the tubes are rare and can be visualized as elevated endoluminal lesions in the virtual endoscopic images. The presence of air bubbles introduced during the procedure of the study is easily identified due to its density, and should not be considered pathological (Fig. 9.6). The tubal polyps are the most frequently observed in the proximal region to the tubes (Fig. 9.7). On the other hand, in the ampullar region, linear and irregular filling defects that correspond to intratubal synechiae are observed more frequently, in general related to inflammatory processes (Fig. 9.8).
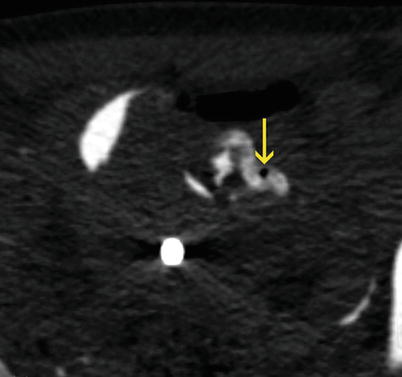
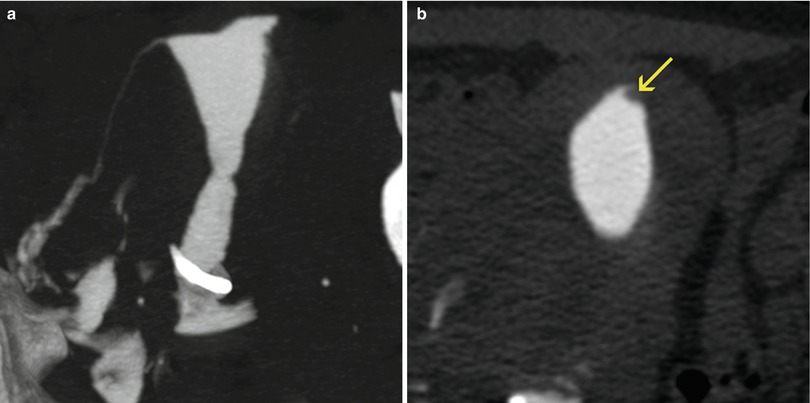
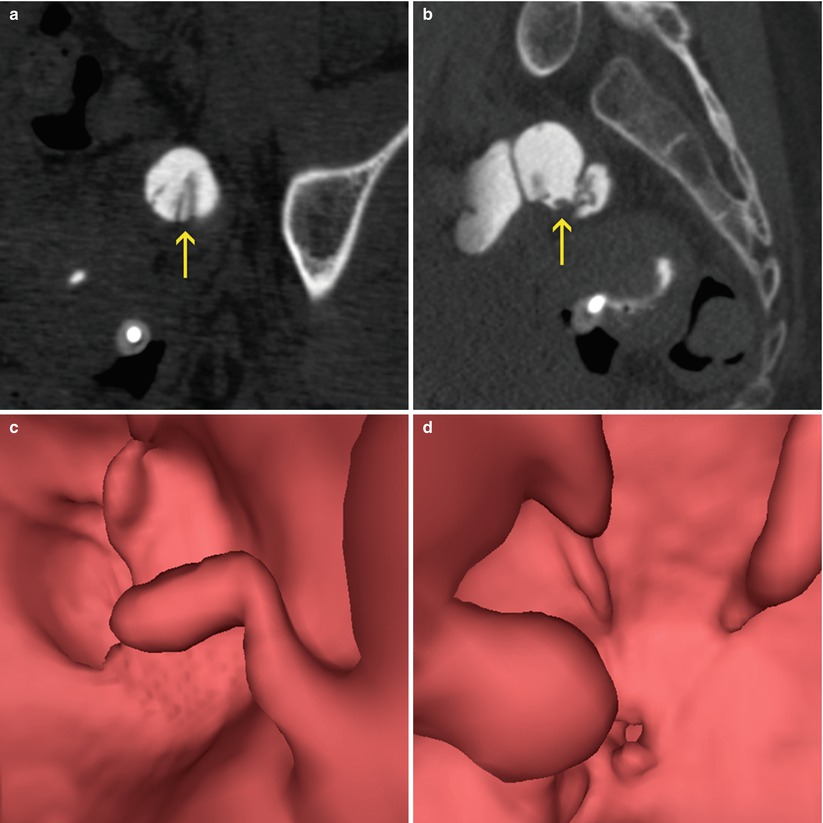
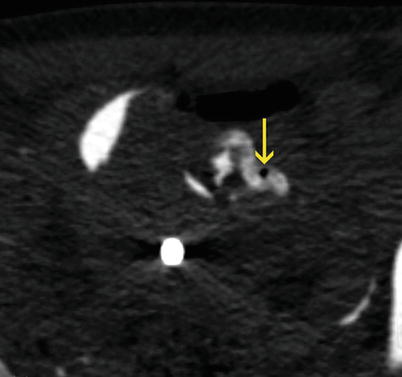
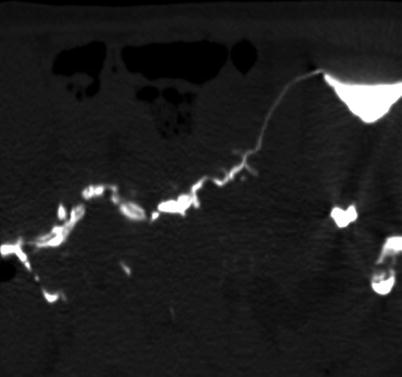
Fig. 9.6
Air bubble. Axial CT image showing a focal filling defect of low density in the ampullary region of the left tube (arrow) corresponding to an air bubble
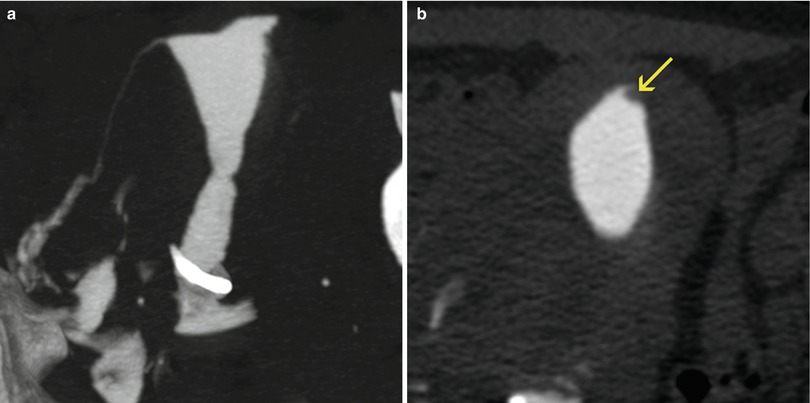
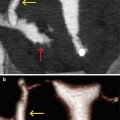
Fig. 9.7
Tubal polyp. (a) Maximum intensity projection image where absence of opacification of the left uterine tube is evidenced. (b) Amplified axial CT image of the left cornual region showing an elevated 3-mm lesion projecting into the intramural portion of the left uterine tube (arrow), causing the tubal obstruction
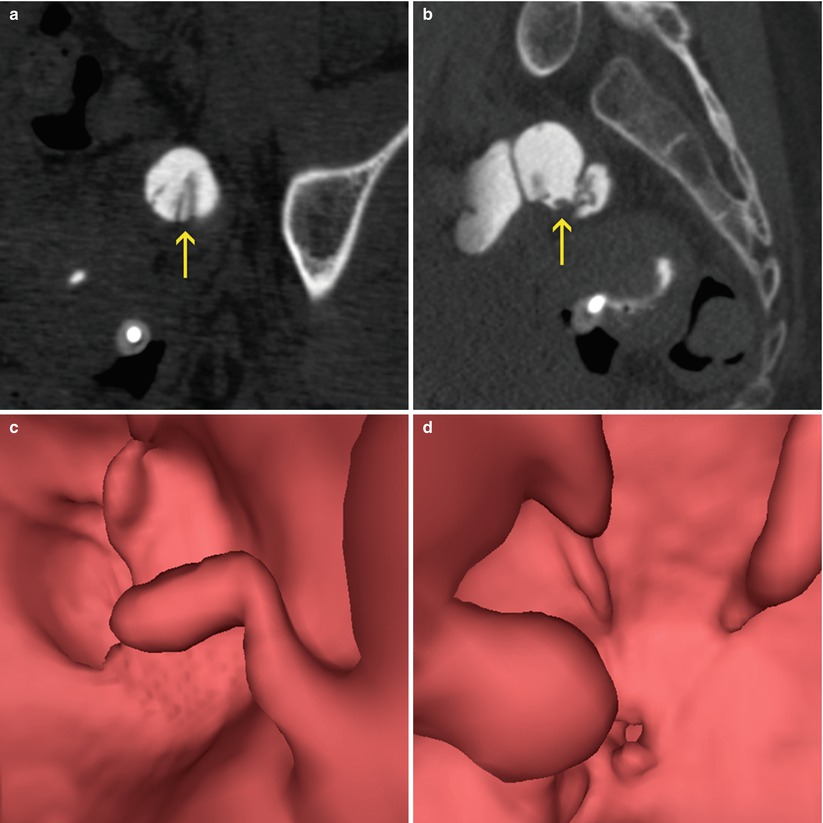
Fig. 9.8
Intra-tubal synechiae. (a, b) Axial and sagittal CT images at the level of the left uterine tube, which is dilated and has lineal and irregular filling defect in its interior (arrows). (c, d) Virtual endoscopy images confirming the presence of intra-tubal synechiae
The alterations of the tubal morphology manifest themselves as irregularities of their edges or with a beaded pattern that alternates stenosis and segmental dilatations. The salpingitis isthmica nodosa is presented as multiple and small pseudodiverticula dilatations of the tubes that generally compromise the isthmic portion (Fig. 9.9). Other inflammatory processes and postsurgical changes can alter the tubal outline and simulate a salpingitis isthmica nodosa, although the most usual presentation form is the beaded pattern (Figs. 9.10 and 9.11) [15].