Fig. 1
Pathogenesis of Tuberculosis
From the infected lymph nodes, bacilli can travel via the lymphatics or bloodstream to many parts of the body, such as the liver, spleen, kidneys, bone metaphysis, brain and other organs, or return to the lungs causing secondary lung lesions. Infants and young children have poor cell-mediated immunity, so when infected, they show a higher incidence of TB than adults or older children.
In children, the disease usually develops soon after the primary infection (primary TB disease) but the bacilli can also lie dormant in tissue macrophages for many years, only to develop the disease some decades later (secondary or reactivation TB). Complete eradication of the bacillus by the immune system never occurs, and it is still very difficult even with the use of effective antituberculosis therapy (Ehlers 1999). Calcified lesions are sterile in 85 % and fibrotic lesions in 86 %. In contrast, solid caseous lesions are sterile in only 50 % (Moulding 1999).
4 Clinical Aspects
Humans display a wide spectrum of immunologic response to TB, reflected in the diverse clinical manifestation ranging from asymptomatic infection to hematogenous dissemination with severe fatal disease. Numerous factors determine an individual’s risk of developing disease once infected including malnutrition, recently acquired infection, immune suppression including human immunodeficiency (HIV) infection, and age. Children < 5 years of age infected with TB are at a higher risk of developing TB disease. Among infants (age < 1 year), 43 % of those infected will develop disease compared to 24 % in children aged 1–5 years, 15 % of adolescents, and 5–10 % of adults over a lifetime (Nelson and Wells 2004).
Most infants and children who become infected with M. tuberculosis will have LTBI. These children have a reactive TST, normal or minimal chest radiograph findings, no clinical evidence of TB, and presumed with low numbers of viable tubercle bacilli that are dormant. Recently, new diagnostic techniques have been developed to diagnose TB infection in vitro: the IGRA to quantify the IFN-γ released by sensitized T cells stimulated with specific M. tuberculosis antigens (Dominguez et al. 2009). Those children who are symptomatic demonstrate few symptoms or signs of pulmonary disease at the outset. Fewer than half develop non-specific symptoms such as fever, anorexia, and weight loss. Most develop cough and many wheeze. If untreated, symptoms and signs of pulmonary bronchopneumonia and extrapulmonary disease may become apparent. Children with LTBI should be treated because of the high risk of disease progression, more years of developing active disease later in life, and the potential of spreading the disease (Mandalakas and Starke 2005). Disease progression is usually indicated by persistent, non-remitting symptoms, although the rate of progression is variable. In a majority of cases (>90 %), disease occurs within a year after primary infection, with the youngest children at greatest risk of progression (Marais et al. 2004a).
For the absolute diagnosis of TB, the demonstration on culture of M. tuberculosis in secretions or tissue of the patient is required. A positive TST demonstrates that the individual has been infected with M. tuberculosis but it cannot tell whether the bacilli are living in a quiescent latent state or actively replicating and causing disease. When the pathology is virtually confined to the lungs, as is usually the case in adults with pulmonary TB, it is relatively easy to confirm the diagnosis by sputum culture. When the principal focus of infection is the intrathoracic lymph nodes, as often is the situation in infants and young children, the organisms are inaccessible and it becomes difficult to prove that the patient has TB. Furthermore, children produce little sputum, which, in addition, contains few microorganisms, and they generally swallow it. Because of these factors and the difficulties associated with obtaining adequate samples of swallowed sputum from the stomach, the diagnosis of TB is confirmed bacteriologically in considerably less than half (range 10–75 %) of infants and young children who are treated for TB (Klein and Iseman 1999; Marais 2008). Thus, the triad of a positive TST, abnormal chest radiographs and a history of exposure to an adult with TB remains the most effective method for diagnosing TB in children.
Primary TB has been used to describe pediatric pulmonary disease that arises as a complication of the TB infection. In children, disease frequently complicates the initial infection immediately, making the distinction between the two stages impossible. Miliary and meningeal TB can develop any time, but they are more likely to occur during the initial 3 months following the primary infection. Endobronchial TB can also develop at this time. Tuberculosis of the pleura and peritoneum characteristically occurs 3–7 months after demonstration of a positive skin test (Inselman 1996).
5 Imaging Techniques
Imaging methods such as chest X-ray, chest US, and chest CT are extremely important tools for the diagnosis of pediatric pulmonary TB. In some instances, particularly in difficult cases, they offer the only way to reach a correct diagnosis and a thorough evaluation of the extent of the disease.
5.1 Chest X-Ray
Chest radiography remains the first and most widely used imaging technique for the evaluation of pulmonary TB in children. Although it has low sensitivity and specificity (Smuts et al. 1994; Swingler et al. 2005) and the radiographic findings vary, pronounced lymphadenopathy with or without airway compression is suggestive of TB. Both anterior and lateral views are required for optimal lymph node visualization, although it may remain difficult to visualize enlarged lymph nodes with certainty (De Villiers et al. 2004). A normal chest X-ray in a patient suspected with TB could be misleading because a subtle primary lesion maybe small, diffuse, or obscured by normal structures (Andronikou et al. 2004). An apparently normal chest X-ray cannot exclude presence of pulmonary TB, but when positive, the X-ray findings although not specific, closely reflect the pathological changes of the disease (Lamont et al. 1986).
5.2 Computed Tomography
CT is the examination of choice in unusual, complicated, or disseminated presentations of the disease. It is also helpful for the evaluation of infants with positive skin test and normal chest X-rays, and for older children with either a history of recent exposure to TB or a positive skin test and inconclusive chest X-ray findings. In small children with disseminated or miliary TB, head CT should always be performed as well. Recognition of brain lesions, which commonly occur in these patients, can influence therapy.
CT scan is very good in the assessment of subtle lung parenchymal disease as well as lymph nodes, which may not be apparent on radiographs (Swaminathan et al. 2005). The advantages of CT over conventional radiographs in defining the extent of the disease and its possible complications (bronchial, pleural, pericardiac, and chest wall involvement) have been well documented in the literature (Kim et al. 1997). Since the search for lymph nodes is crucial in the study of chest TB in children, contrast-enhanced scans are preferred. Unenhanced scans are not routinely obtained. Multiplanar and 3D reconstructions are also helpful in some cases, particularly in the evaluation of tracheobronchial disease.
CT scans cannot be routinely recommended because of the high cost, and risks associated with intravenous contrast administration. Another important issue is the radiation-associated risks, so therefore a clear indication for the procedure has to be present. Radiation dose reduction measures including the use of automatic dose modulation techniques and the adaption of weight-based pediatric CT protocols are recommended.
5.3 Magnetic Resonance Imaging
MRI is an excellent method for detecting mediastinal lymph node, pleural disease, and pericardial involvement. MRI also has the advantage of multiplanar imaging capability. However, high cost, need for sedation in most cases and poor visualization of the lung parenchyma limits its use.
5.4 Ultrasound
US is an easy to use, inexpensive, non-aggressive technique that is useful for identifying mediastinal lymph nodes (Bosch-Marcet et al. 2004) and differentiating them from a large normal thymus in patients who present mediastinal widening. It is also helpful for detecting pleural and pericardial effusion. Ultrasound is also an excellent tool for image-guided interventions.
6 Imaging Features of Intrathoracic Tuberculosis
6.1 Infection: The Primary Complex
Infection will result in pathologic changes and associated clinical disease. The tubercle bacilli that reach the terminal airway induce a local inflammatory process referred to as parenchymal focus (Ghon focus). Bacilli originating from the focus drain via local lymphatics to the regional lymph nodes. The triad of the Ghon focus, local tuberculous lymphangitis and involved regional lymph nodes is referred to as “primary complex” (Fig. 2). Bacilli located in the regional lymph nodes may enter the systemic circulation directly or via the lymphatic duct, which may disseminate bacilli to a variety of target organs, where the bacilli may survive for decades (Mandalakas and Starke 2005). Of infected children, 95 % will be subclinical and will not develop disease. The primary focus becomes encapsulated, and perifocal inflammation increases and manifests as a granuloma. The pathologic events associated include caseous necrosis, fibrosis, and healing of the primary complex components with or without calcification depending on the degree of necrosis and caseation. Although these sequences of events occur in LTBI, the resolution may not be complete and viable TB bacilli may persist for many years, potentially reactivating and causing TB disease months to years later (Feja and Saiman 2005).
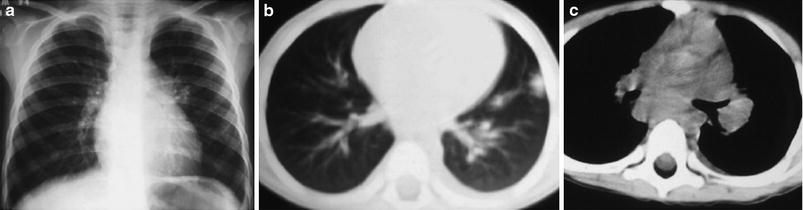
Fig. 2
a Chest X-ray of an 8-year-old boy shows slight enlargement of the left hilum. b Unenhanced CT of the same patient demonstrates peripheral pulmonary focus in the left lower lobe and lymphangitis. c Mediastinal window shows left hilar adenopathy
Lymphadenopathy (present in 92 %) with or without a visible Ghon focus is the radiographic hallmark of TB infection. Typically, it involves the hilar and paratracheal regions (Leung et al. 1992). The right side is more commonly affected than the left because of the usual pattern of lymphatic circulation within the lungs (Fig. 3). A left-sided parenchymal focus often leads to bilateral hilar adenopathy, whereas a right-sided focus is usually associated only with right-sided lymphadenitis (Starke 1999). With serial radiographs, 40 % of these lesions cleared within 6 months, a further 30 % within 1 year, and the remainder persisted for up to 4 years. Calcification, an indication of clinical quiescence, which usually occurs between 12 and 14 months, developed in 20–50 % of children with visible lymph node involvement (Marais et al. 2004a). Lateral views are particularly useful in detecting hilar lymphadenopathy, and both frontal and lateral views should be obtained (Fig. 4).
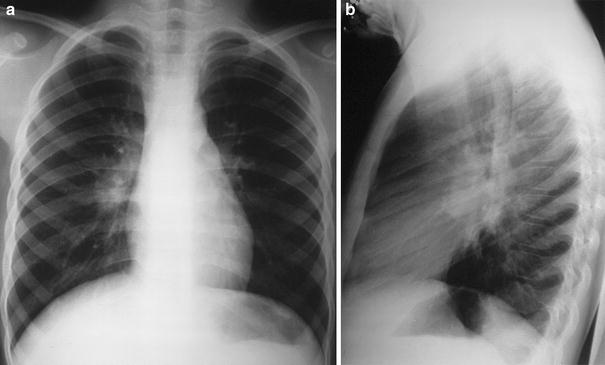
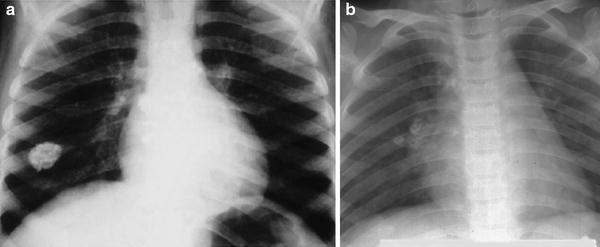
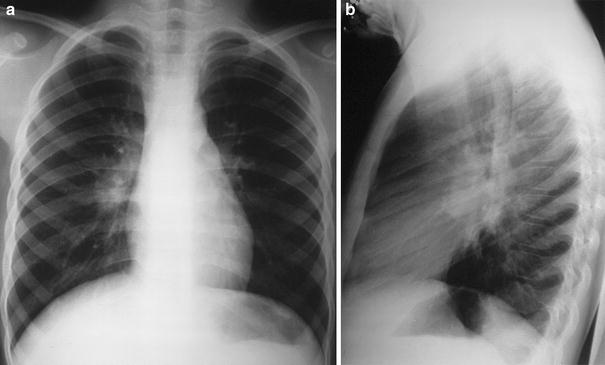
Fig. 3
a Frontal view Chest X-ray of a 7-year-old girl with positive tuberculin skin test shows a prominent right perihilar shadow compatible with lymphadenopathy. No appreciable lung parenchymal abnormality is seen. b Lateral view confirms the lymphadenopathy superimposed on the mediastinal vessels
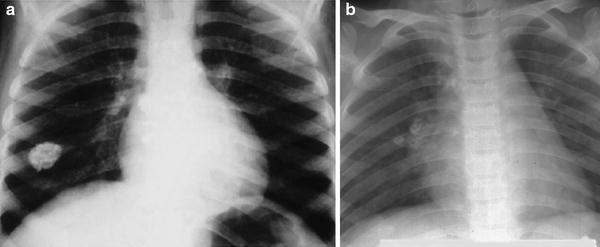
Fig. 4
a Primary complex with calcified pulmonary focus in a 6-year-old child. b Calcified right hilar lymph nodes in a 5-year-old boy with latent tuberculosis infection
The Ghon foci may be too small to be radiographically visible but can also undergo caseation and calcify. There is no predilection for any specific part of the lung but a right-sided predominant distribution is well recognized (Leung et al. 1992) and approximately 70 % of the primary foci are subpleural in location (Mandalakas and Starke 2005).
6.2 Primary Pulmonary Tuberculosis: Spectrum of Disease Progression
6.2.1 Progressive Ghon Focus
Disease progression may occur at the site of the organism deposition (Ghon focus), within the regional lymph nodes, or following disease spread. Ghon focus represents the first site of possible disease progression and is a sign of poor disease containment. Parenchymal involvement in primary pulmonary TB most commonly appears as homogeneous consolidation, although it can appear patchy, linear, nodular, and mass like (Fig. 5). Caseation necrosis, liquefaction, or calcifications can be seen within the consolidation and can progress into extensive lung damage (Fig. 6). Discharge of the caseated material from a Ghon focus into a bronchus results in the formation of a parenchymal cavity and infants and the immunocompromised are most vulnerable (Marais et al. 2004a) (Fig. 7). Another rare complication is the appearance of bullous or cystic lesions in the lung (Fig. 8). These have been reported to occur during treatment (Matsaniotis et al. 1967), but they were also observed before therapy was initiated. Occasionally peripheral bullous lesions will lead to pneumothorax.
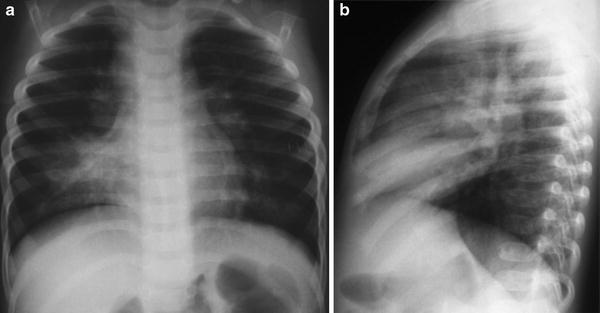
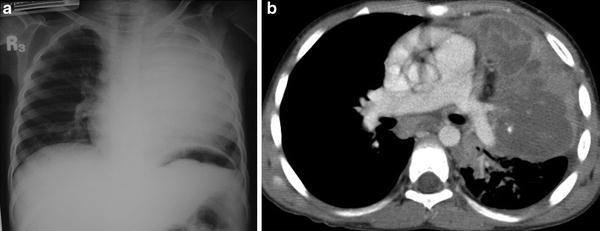


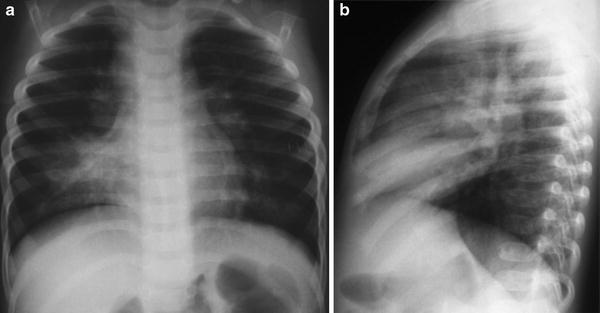
Fig. 5
a Frontal and b lateral views of the chest on a 3-year-old child with chronic cough, fever, and positive tuberculin skin test showing right middle lobe opacity compatible with Ghon focus progression. Bilateral perihilar fullness represents concomitant lymphadenopathy
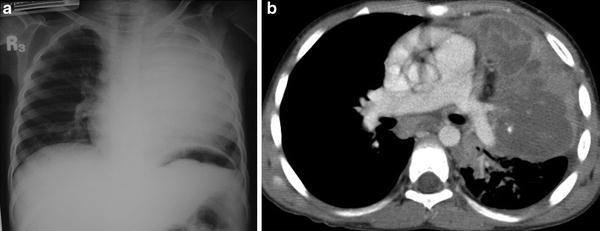
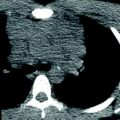
Fig. 6
a Chest X-ray reveals complete opacification of the left upper lobe in this 9-year-old malnourished boy with TB disease. b Contrast-enhanced CT scan in axial view demonstrates consolidation of the left upper lobe with low density areas of non-enhancement compatible with necrosis and early liquefaction. Prominent lymph nodes are seen in the subcarinal region

Fig. 7
Completely opacified right lung with a large cavity communicating with the right bronchus

Fig. 8
A large peripherally located cyst in the left hemithorax in a 3-year-old diagnosed with TB disease
Parenchymal lesions can be uni or multi-focal and are usually seen in areas of greatest ventilation: the middle lobe, the lower lobes, and the anterior segments of upper lobes. This pattern differs from the reactivation TB in adults, which is typically in the apical and posterior segments of the upper lobes (Kim et al. 1997). Parenchymal opacities occur in association with and affect the same side as the nodal enlargement (Leung et al. 1992).
6.2.2 Progressive Lymph Node Disease
Another possible site of disease progression is within the regional lymph nodes, which enlarges due to central caseation and surrounding inflammatory edema. Children 0–3 years of age had higher prevalence of lymphadenopathy (Leung et al. 1992). The small airway size makes children most vulnerable to development of lymphobronchial TB that refers to a spectrum of airways involvement and associated complications that may arise following lymph node disease (Marais 2008). Enlarged and edematous hilar, paratracheal, and sub-carinal lymph nodes may encroach upon the regional bronchus. Intraluminal obstruction results from the granulomatous tissue that develops secondary to inflammatory changes in the bronchial wall, or from caseous material deposited on the eruption of caseated lymph node into the airway. This compression can cause bronchial stenosis and lead to hyperinflation in the distal lung secondary to air trapping, or completely occlude an airway and produce lung collapse.
On chest plain films lymphadenopathy usually presents as asymmetrically distributed paratracheal, hilar and/or sub-carinal lobulated nodes with sharp or ill-defined borders. The enlarged lymph nodes can compress and stretch the bronchi, or compress and displace the trachea (Fig. 9). Sub-carinal lymph node involvement can cause splaying of the mainstem bronchi. Shift of the mediastinum may not occur because of the fixed nature of these lymph nodes (Inselman 1996).
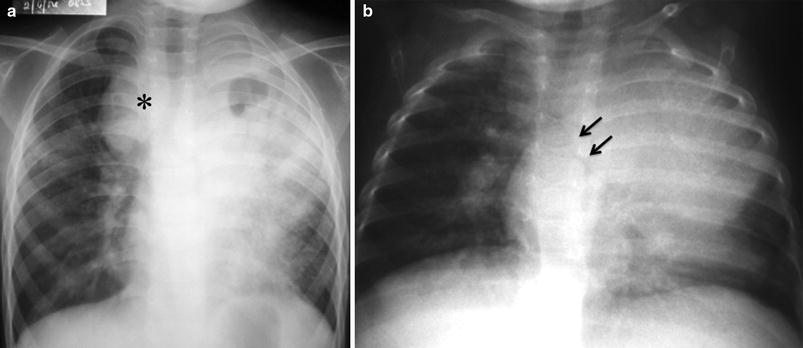
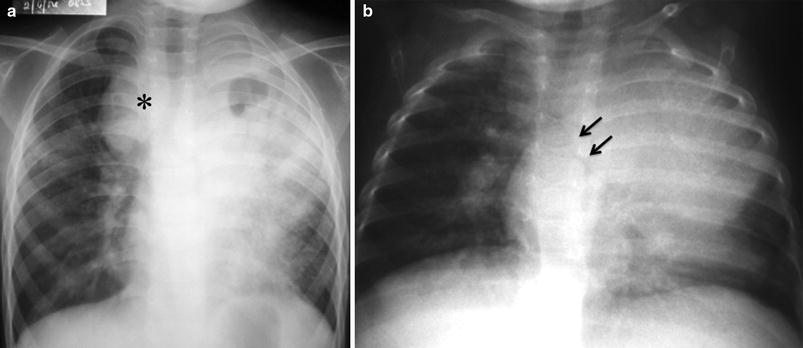
Fig. 9
a Frontal view chest X-ray of a child with primary progressive TB demonstrating significantly enlarged nodes in the right paratracheal region (asterisk) effacing the trachea to the left. There is also progression of lung parenchymal disease with cavitation on the left upper lobe. b Chest X-ray of an 18-month-old boy with enlarged left perihilar lymph nodes effacing the left bronchus (arrows)
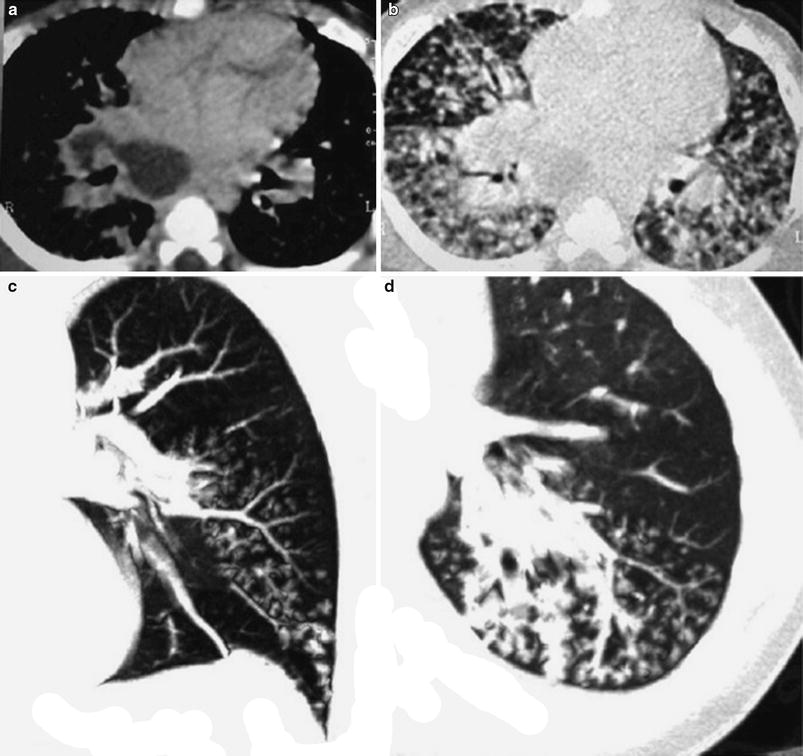
Lymphadenopathy is not always easy to detect on conventional radiographs and CT has a higher sensitivity. On contrast-enhanced CT, TB lymphadenopathy, especially when nodal size exceeds 2 cm in diameter, may have a characteristic appearance consisting of central areas of low attenuation with peripheral rim enhancement and obliteration of perinodal fat. Calcification within the nodes is seen in 15 % (Kim et al. 1997). Another study shows a ghost-like pattern of enhancement of enlarged lymph nodes (Andronikou et al. 2004) (Figs. 10, 11). A study comparing CT and fiberoptic tracheobronchoscopy (FOT) in children with pulmonary TB showed lymph node enlargement resulting in extrinsic compression of the central airways in 86 %. It also showed that CT is 92 % sensitive and 85 % specific in the detection of the degree of airway narrowing as compared to FOT bronchoscopy (Du Plessis et al. 2009) (Fig. 12).
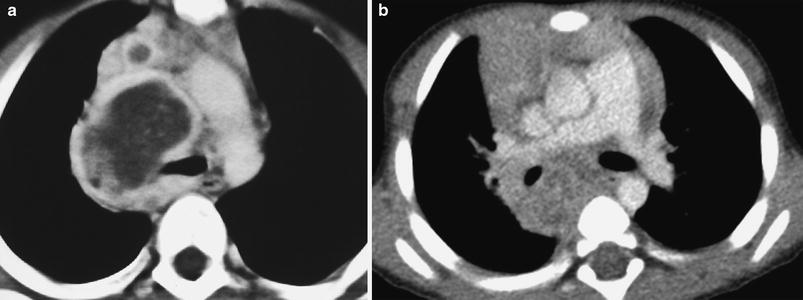
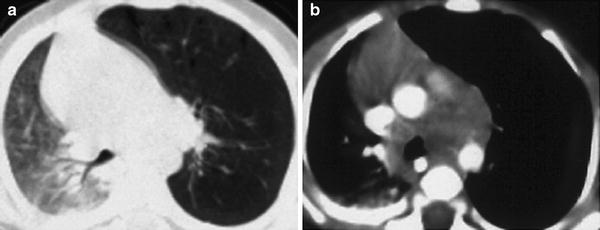
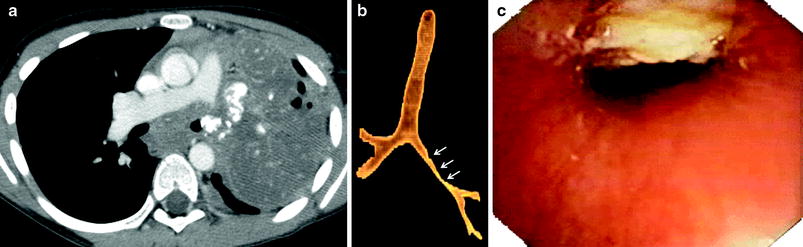
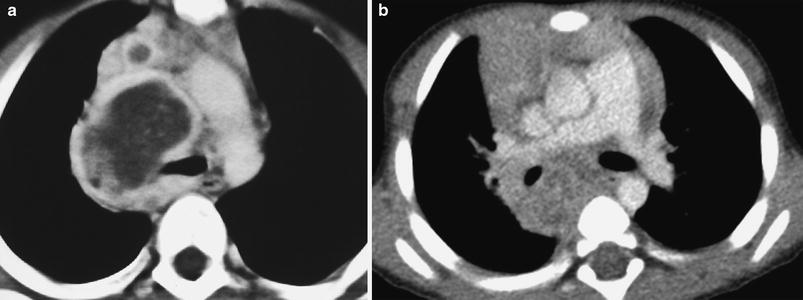
Fig. 10
Contrast-enhanced CT scan demonstrating appearance of TB lymphadenopathy. a Enlarged right perihilar lymph node with central low attenuation and peripheral contrast enhancement. b Enlarged subcarinal lymph nodes widening the carinal angle, displaying a heterogenous ghost-like pattern of enhancement
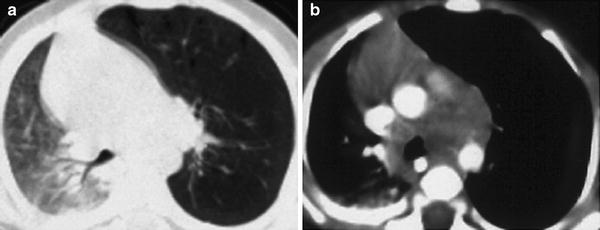
Fig. 11
a, b CT of a 4-month-old boy with obstructive emphysema of the left lung caused by hilar adenopathy
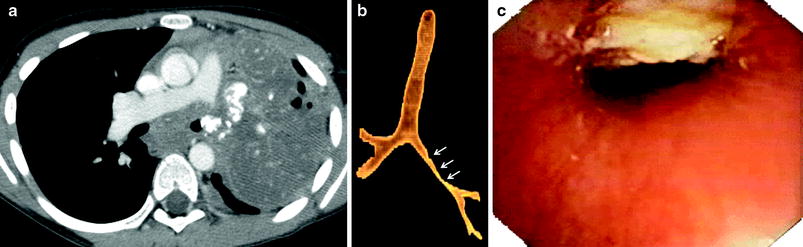
Fig. 12
a Axial CT image showing subcarinal and calcified left hilar adenopathy eroding into the left main bronchus. b CT external surface 3D reconstruction shows irregular narrowing of the left bronchus. c Corresponding image from fiberoptic bronchoscopy shows the caseating lymph node eroding into the bronchus. Courtesy of Dr. Marion O. Sanchez; St. Luke’s Medical Center, Philippines
Bronchopneumonic consolidation could result from intrabronchial spread of a parenchymal cavity with a high organism load or after eruption of a caseated lymph node with variable organism load into the bronchial tree. The radiographic pattern shows large irregular patchy infiltration usually involving more than one lobe of a single lung (Lamont et al. 1986; Marais et al. 2004a). On CT, this will manifest as poorly defined nodules or rosettes of nodules, 2–10 mm in diameter that can be identified as centrilobular or branching centrilobular opacities mimicking the “tree in bud” image. Coalescence of the centrilobular opacities results in focal areas of bronchopneumonia (Webb et al. 1996). Extensive bronchogenic spread can cause other patterns, such as pulmonary consolidation, or multiple nodules throughout the lungs (Fig. 13).