Fig. 15.1
Leiomyoma of the flexor compartment of the right arm in a 56-year-old woman. (a) Ultrasound, axial plane. Ultrasound shows a well-circumscribed, oval, and slightly hypoechoic mass within the biceps muscle. (b) Axial T1-WI. The well-defined mass is hyperintense to muscle on T1-WI. (c) Axial T2-WI. The well-defined mass shows an inhomogeneous, stippled high signal on T2-WI. (d) Axial T1-WI after IV administration of gadolinium contrast. Inhomogeneous enhancement is seen
15.2.1.2 Leiomyosarcoma (Excluding Skin)
Definition and Clinical Findings
Leiomyosarcoma is a malignant neoplasm showing pure smooth muscle differentiation ([12], Fourth revision). Extrauterine leiomyosarcomata typically occur in adults [8].
There are four main subtypes, including cutaneous, subcutaneous, deep soft tissue, and vascular leiomyosarcoma. Cutaneous leiomyosarcoma has a far better prognosis than the subcutaneous type.
Deep soft tissue leiomyosarcomata mostly occur in the retroperitoneum (usually in the perirenal space) and only in 12–41 % in the extremities (particularly in the thigh) [7, 32, 38]. Of note, bone leiomyosarcoma is a distinct and rare entity, which is not addressed in the WHO classification of soft tissue tumors and bone ([12], Fourth revision). Deep soft tissue leiomyosarcomata in the retroperitoneum present at a more advanced stage than vascular leiomyosarcomata, which is likely because first mentioned have more space to grow before causing symptoms [7].
Vascular leiomyosarcomata arise in large vessels, most commonly in the inferior vena cava or lower extremity veins. The clinical findings depend on the involved part of the vein and the extent of the lesion. In the inferior vena cava, upper-segment involvement may manifest as Budd-Chiari syndrome, middle-segment involvement as nephrotic syndrome, and infrarenal involvement as edema in the lower extremity [34]. The lesions may cause vascular obstruction and thrombosis [4, 23].
Imaging
Cutaneous and subcutaneous leiomyosarcomata usually present as well-defined, relatively small, homogeneously enhancing tumors, often associated with fascial edema [16] (Fig. 15.2). Deep soft tissue and vascular leiomyosarcomata show similar imaging features [7, 16] and mostly present as large, heterogeneous masses with variable signal intensities, central necrosis, and marked peripheral and septal enhancement [44] (Figs. 15.3, 15.4, 15.5, and 15.6). Intralesional calcifications may be detected in a minority of leiomyosarcomata [5]. Secondary bone involvement is seen in up to 10 % [41, 44] (Fig. 15.6). Vascular leiomyosarcomata exhibit three main growth patterns: extraluminal (62 %), intraluminal (5 %), and combined extra- and intraluminal (33 %) [19]. Leiomyosarcoma of the inferior vena cava can be classified into three groups according to level affected: segment I, infrarenal; segment II, inter- and supra-renal up to but not including the main suprahepatic veins; and segment III, suprahepatic with possible intracardiac extension [22]. Intravascular leiomyosarcoma may be confused with deep vein thrombosis at US [8]. Both MR imaging and CT are useful for differentiating intravascular leiomyosarcoma of the inferior vena cava from a simple thrombus and for staging [34].
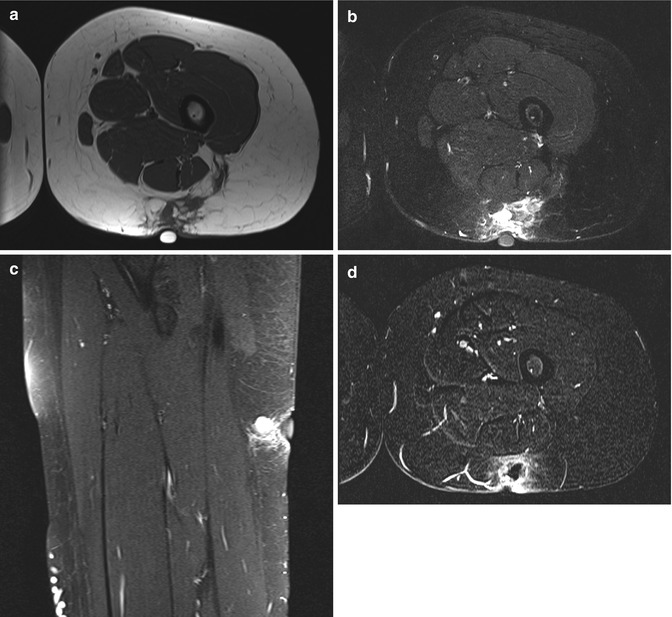
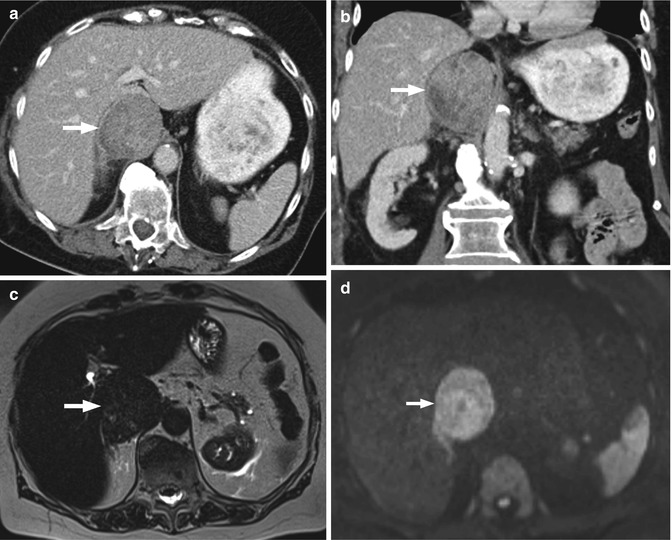
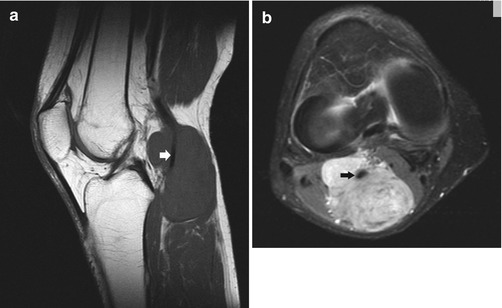

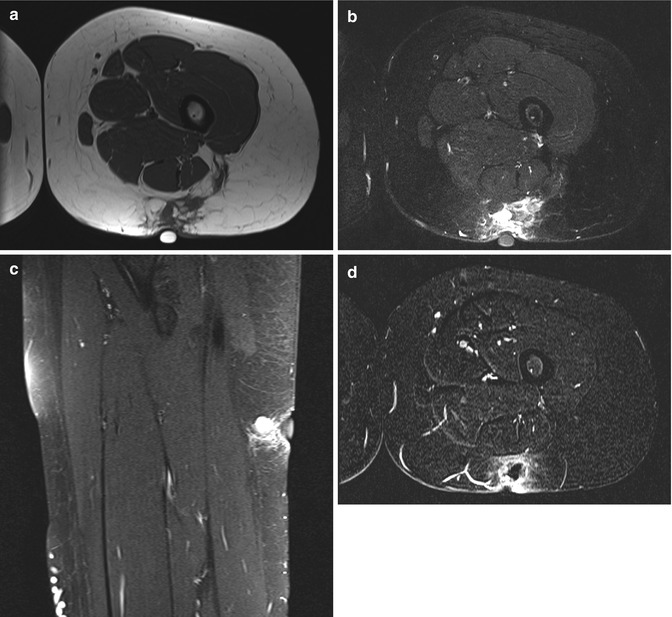
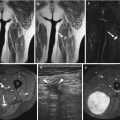
Fig. 15.2
Subcutaneous leiomyosarcoma of the thigh in a 39-year-old woman. (a) Axial T1-WI. (b) Axial FS T2-WI. (c) Sagittal FS T2-WI. Ill-defined, subcutaneously located mass on the dorsal side of the thigh with an intermediate signal intensity on T1-WI and hyperintense signal intensity on FS T2-WI. (d) Axial T1-WI after IV administration of gadolinium contrast. Inhomogeneous, mainly peripheral enhancement is seen
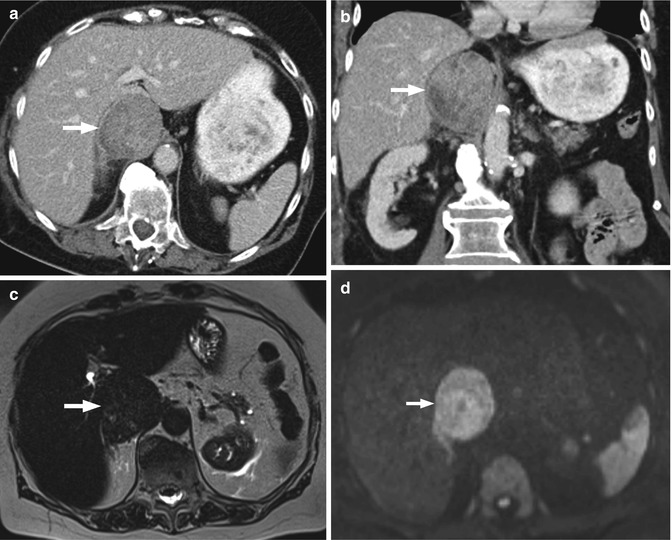
Fig. 15.3
Leiomyosarcoma of the inferior vena cava in an 84-year-old woman. (a) Axial contrast-enhanced CT image. (b) Coronal reformatted contrast-enhanced CT image. Well-delineated retroperitoneal mass with heterogeneous enhancement embedded in the inferior vena cava located between the renal veins and the confluence of the hepatic veins (i.e., middle segment). (c) Axial T2-WI. Heterogeneous mass slightly hyperintense signal compared to the liver parenchyma. (d) Axial diffusion-weighted image. Restricted diffusion in the largest part of the mass, with a small focus of absent diffusion restriction (Used with permission from Peters et al. Leiomyosarcoma of the inferior vena cava. Eurorad: radiological case database (2015), URL: http://www.eurorad.org/case.php?id=12591, DOI: 10.1594/EURORAD/CASE.12591)
Fig. 15.4
High-grade leiomyosarcoma in the left thigh. (a) Coronal reformatted CT image. Large subcutaneous soft tissue mass abutting the adductor muscles. Note the intimate relationship with an adjacent subcutaneous vein (white arrow). (b) Axial T1-WI. (c) Coronal FS T2-WI. The mass is of inhomogeneous signal intensity on both pulse sequences. (d) Coronal FS T1-WI after IV administration of gadolinium contrast. There is marked inhomogeneous enhancement of the lesion. An intimate relationship with an adjacent subcutaneous vein is present (white arrow) (Color figure online)
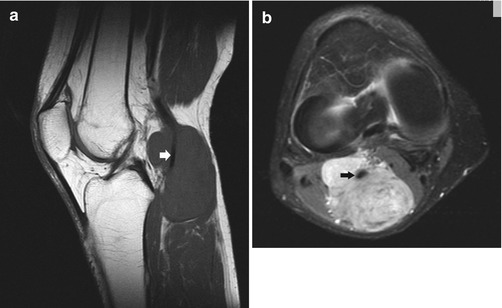
Fig. 15.5
Leiomyosarcoma of the right knee. (a) Sagittal T1-WI. (b) Axial FS T2-WI. Huge mass encasing the popliteal vessels (arrows)

Fig. 15.6
Leiomyosarcoma of the right thigh in a 26-year-old woman with secondary bone involvement. (a) Plain radiograph. Plain radiograph demonstrates an indistinct soft tissue swelling with extensive mottled bone involvement and a pathological fracture of the femoral neck. (b) Axial CT. CT confirms areas of bone erosions and patchy sclerosis. (c) Axial T2-WI. (d) Coronal T1-WI. A soft tissue mass surrounds the hip and extends towards the midline. The infiltrating mass has a heterogeneous high signal intensity on T2-WI and an intermediate signal intensity on T1-WI (e) Coronal FS T1-WI after IV administration of gadolinium contrast. There is marked inhomogeneous enhancement of the lesion
15.2.2 Skeletal Muscle Tumors
15.2.2.1 Extracardiac Rhabdomyoma
Definition and Clinical Findings
Rhabdomyoma is a rare benign tumor composed of striated muscle cells [8]. There are two broad categories, cardiac and extracardiac rhabdomyoma. Cardiac rhabdomyoma is associated with the tuberous sclerosis complex. Extracardiac rhabdomyoma is further subdivided in adult, fetal, and genital subtypes.
Adult rhabdomyoma is a benign soft tissue neoplasm showing mature skeletal muscle differentiation ([12], Fourth revision). The adult subtype is a slowly growing painless mass most typically seen in the neck and rarely in the somatic skeletal muscle [27].
Fetal rhabdomyoma is a benign rhabdomyoblastic tumor with myotube-like differentiation ([12], Fourth revision). The less frequent fetal subtype has a predilection for the postauricular region ([12], Fourth revision). The median age of presentation is 4 years [8, 27].
Imaging
Cardiac rhabdomyoma are usually detected on echocardiography as solitary or multiple hyperechoic mass(es) within the myocardium. Reports of both US and MR imaging features of extracardiac rhabdomyoma are scarce. Maglio et al. [28] reported a case of nonspecific oval hypoechoic mass in the neck of an adult patient. MR imaging reveals a well-delineated mass isointense or hyperintense compared to skeletal muscle on T1- and T2-weighted images (Fig. 15.7). Central necrosis and hemorrhage are rarely seen. After administration of intravenous gadolinium contrast, there is marked homogeneous or heterogeneous enhancement [8, 27] (Fig. 15.7).
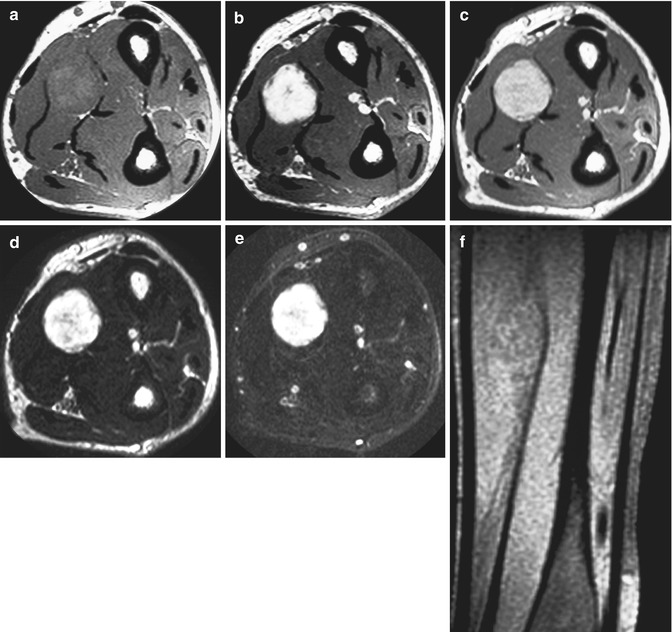
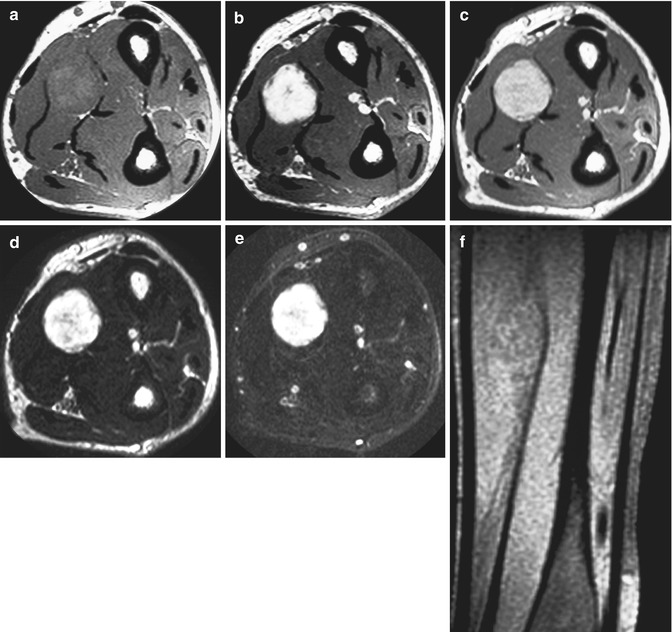
Fig. 15.7
Adult rhabdomyoma of the forearm in a 76-year-old man. (a) Axial T1-WI. A round mass lesion is seen between the superficial and deep flexor digitorum muscles. The lesion is inhomogeneous and has a higher signal than the adjacent normal muscle. (b) Axial FS T1-WI after IV administration of gadolinium contrast. There is marked inhomogeneous enhancement of the lesion. (c) Axial PD. (d) Axial T2-WI. (e) Axial FS T2-WI. (f) Sagittal T1-WI. The lesion has a high signal intensity on PD and T2-WI. The lesion remains hyperintense on T2-WI with fat suppression. On T2-WI with fat suppression and T1-WI with fat suppression, fatty components can be excluded
15.2.2.2 Rhabdomyosarcoma
Definition and Clinical Findings
Rhabdomyosarcoma is the most common soft tissue tumor in children, accounting for 5–8 % of all childhood cancers [18, 35]. It is very rare in adults.
There are four main histological subtypes: embryonal, alveolar, pleomorphic, and spindle cell/sclerosing; each corresponding with a different prognosis. The embryonal subtype is most common in children, whereas the alveolar subtype is most common in young adults and adolescents [36].
Embryonal rhabdomyosarcoma is a primitive, malignant soft tissue tumor with phenotypical and biological features of embryonic skeletal muscle cells ([12], Fourth revision). Embryonal rhabdomyosarcomata are most frequent in the head and neck (47 %) and the genitourinary system (28 %) and only rarely involve the extremities (6 %). There is an increased incidence in Beckwith-Wiedemann syndrome [33].
Alveolar rhabdomyosarcoma is a highly cellular, malignant neoplasm containing a monomorphous population of primitive cells with round nuclei and features if arrested myogenesis ([12], Fourth revision). Alveolar rhabdomyosarcoma is more aggressive than embryonal rhabdomyosarcoma and has a poorer prognosis. The outcome is also affected by age, stage, and location. Tumors located in the extremities have a poorer prognosis ([12], Fourth revision).
Pleomorphic rhabdomyosarcoma is a high-grade sarcoma composed of bizarre polygonal, round, and spindle cells that display skeletal muscle differentiation without embryonal or alveolar components ([12], Fourth revision). Pleomorphic rhabdomyosarcoma occurs almost exclusively in adults, typically in the deep soft tissues of the extremities, particularly the thigh [1]. The prognosis is poor.
Spindle cell/sclerosing rhabdomyosarcoma is an uncommon variant that has spindle cell morphology ([12], Fourth revision). Spindle cell/sclerosing rhabdomyosarcomata occur both in children and in adults with a male predilection. Tumors with spindle cell morphology occur predominantly in the paratesticular region in children and in the deep soft tissues of the head and neck in adults. Lesions with sclerosing morphology are most common in the limbs in both age groups. In children, tumors with spindle cell morphology are usually diagnosed at an early stage, with limited disease burden and a 95 % survival rate at 5 years ([12], Fourth revision). In adults the outcome of spindle cell/sclerosing rhabdomyosarcoma is significantly worse with a recurrence rate and metastasis of approximately 40–50 % ([12], Fourth revision).
Imaging
Plain radiographs and CT may show local bone invasion, which is seen in about 25 % of cases. Bone metastases may occur and are usually lytic and more rarely mixed [8, 27].
US findings of rhabdomyosarcoma are nonspecific [49].
MR imaging features are also nonspecific; isointense to muscle on T1-weighted images and heterogeneous hyperintense on T2-weighted images, often with necrotic foci, may be seen. Marked enhancement is the rule, particularly in the alveolar subtype which has a prominent vascularity [1] (Figs. 15.8, 15.9, 15.10, 15.11, 15.12, and 15.13).
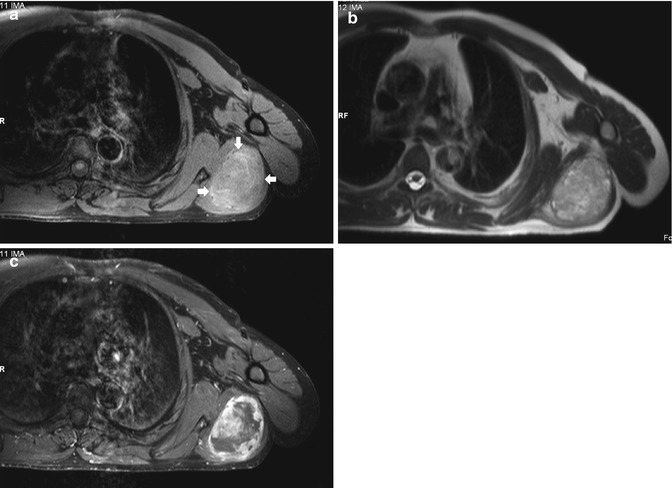
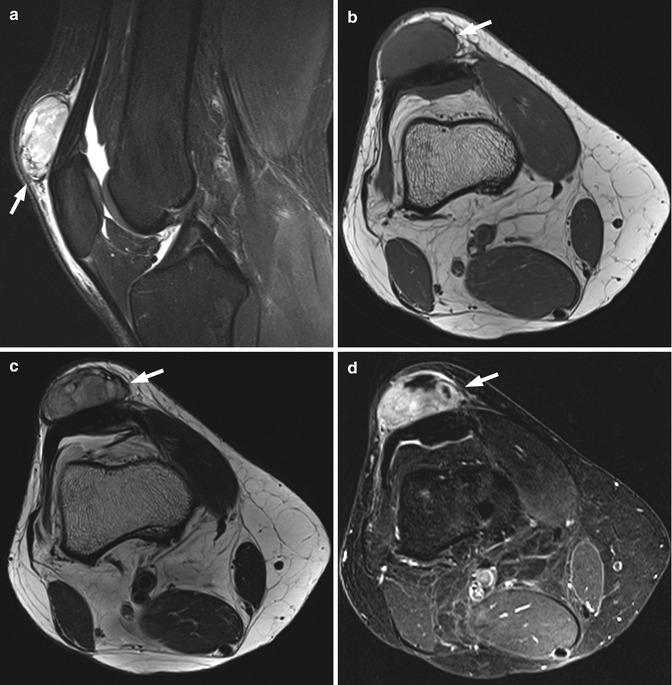
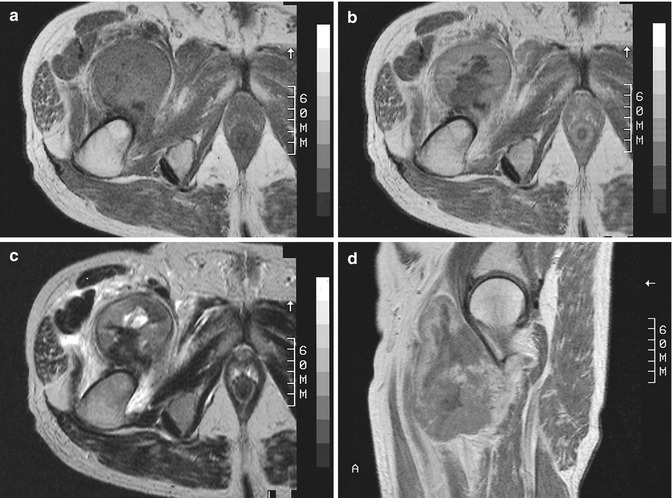
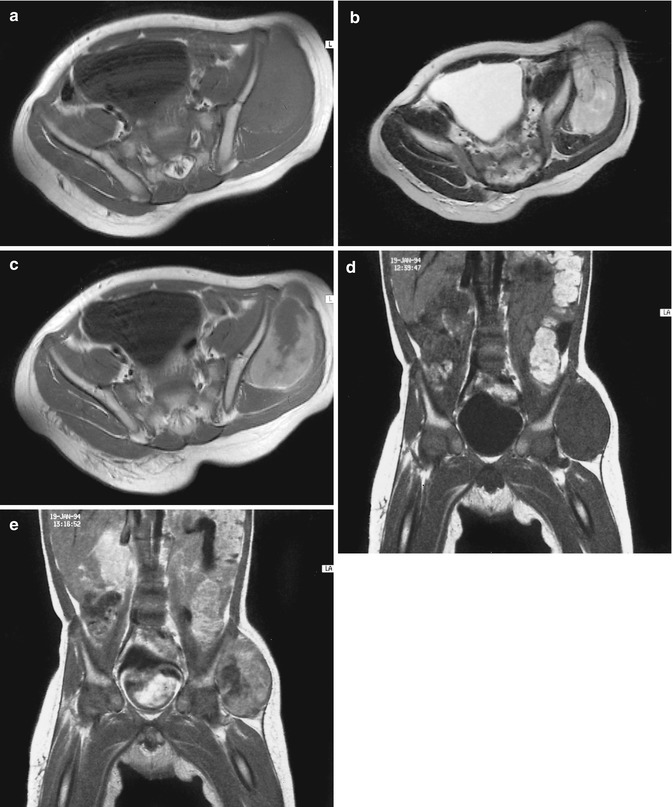
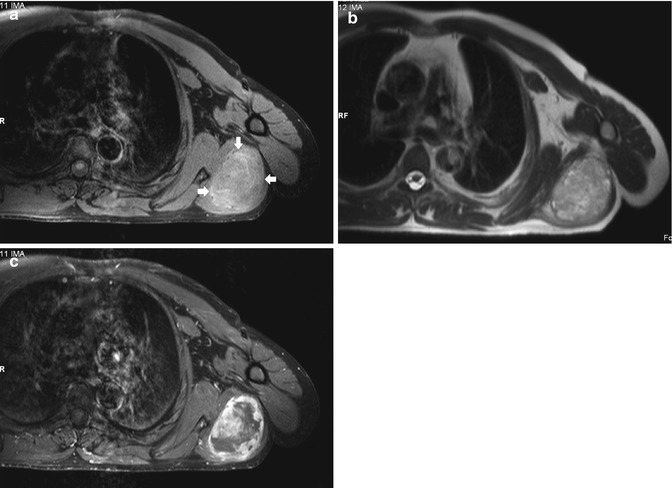
Fig. 15.8
Pleomorphic rhabdomyosarcoma in the left deltoid muscle. (a) Axial FS T1-WI. (b) Axial FS T2-HASTE. Large inhomogeneous mass on both pulse sequences. (c) Axial FS T1-WI after IV administration of gadolinium contrast. There is marked heterogeneous enhancement
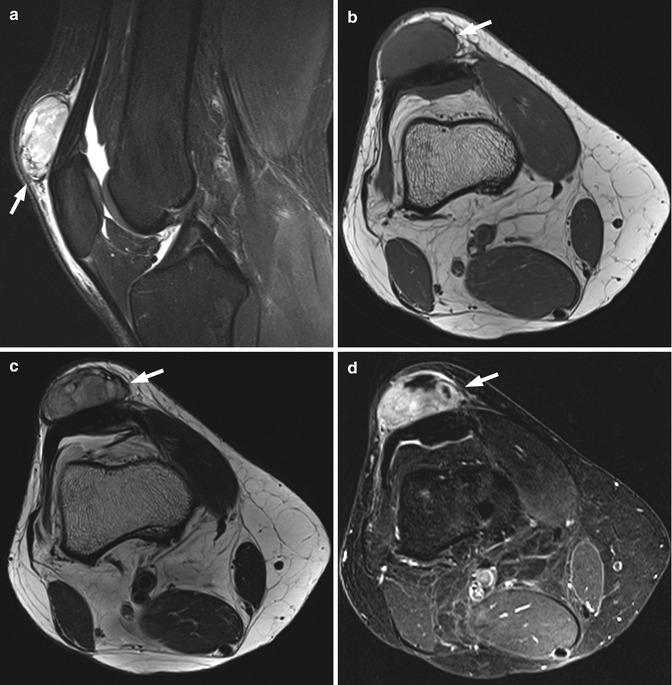
Fig. 15.9
Pleomorphic rhabdomyosarcoma of the knee. (a) Sagittal FS T2-WI. (b) Axial T1-WI. (c) Axial T2-WI. Ellipsoid, inhomogeneous mass on all pulse sequences located in the soft tissues ventral to the patella. (d) Axial FS T1-WI after IV administration of gadolinium contrast. There is marked heterogeneous enhancement
Fig. 15.10
Alveolar rhabdomyosarcoma of the left hypothenar in an 11-year-old girl, presenting with a painless swelling for 6 months. (a) Axial T1-WI. A large mass within the hypothenar muscles (abductor digiti minimi) with inhomogeneous, slightly hyperintense signal intensity compared to adjacent normal muscle. (b) Axial FS T2-WI. The lesion is ill-defined with a predominantly high signal intensity on T2-WI. Presence of inhomogeneity with a central scar-like component of low signal intensity. (c) Coronal FS T2-WI. The lesion has a fusiform shape. (d) Axial T1-WI after IV administration of gadolinium contrast. The lesion shows septal and central enhancement
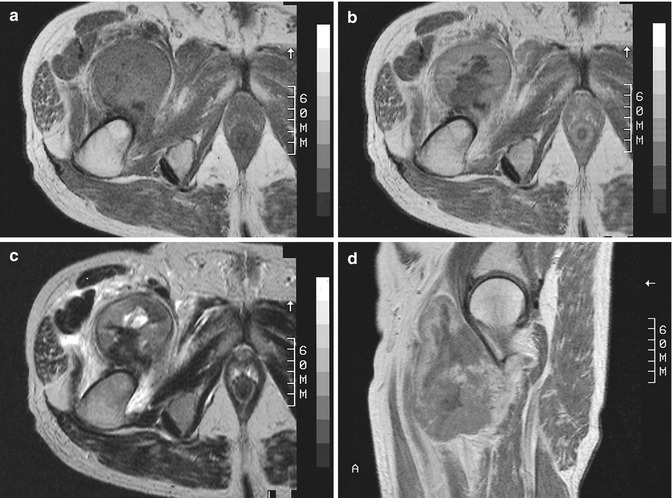
Fig. 15.11
Pleomorphic rhabdomyosarcoma of the right thigh in a 63-year-old man. (a) Axial T1-WI. (b) Axial T1-WI after IV administration of gadolinium contrast. (c) Axial T2-WI. (d) Sagittal T1-WI after IV administration of gadolinium contrast. Rounded, well-circumscribed mass with inhomogeneous intermediate signal intensity on T1-WI (a). The mass is even more inhomogeneous on T2-WI with the presence of a central fluid collection anterior to an area of low signal intensity (c). There is inhomogeneous, predominantly peripheral enhancement (b, d). A malignant tumor is suggested by the inhomogeneous appearance in all sequences, location, and volume of the lesion
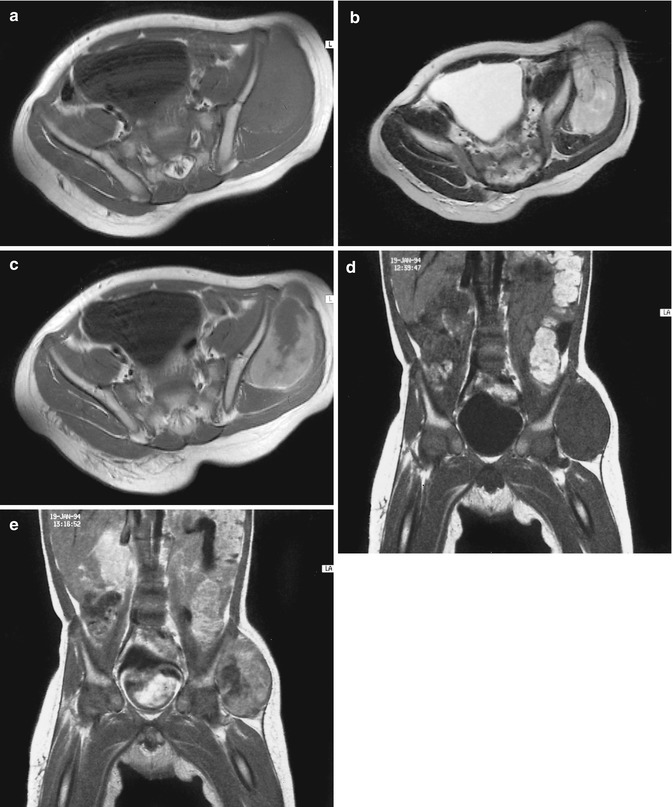
Fig. 15.12
Embryonal rhabdomyosarcoma of the left buttock in a 22-month-old boy. (a) Axial T1-WI. (b) Axial T2-WI. (c) Axial T1-WI after IV administration of gadolinium contrast. A large tumor arising in a gluteus muscle with a hypointense to isointense signal intensity compared to normal muscle on T1-WI and a high signal intensity with some internal strands of low signal intensity on T2-WI. There is evident enhancement of some parts of the tumor, but large areas do not enhance at all. No necrosis is seen. Comparable signal patterns are seen on a follow-up MR study 2 months later (d, e). (d) Coronal T1-WI 2 months later. (e) Coronal T1-WI after IV administration of gadolinium contrast 2 months later
Fig. 15.13
Rhabdomyosarcoma of the adductor region of the right thigh in a 78-year-old woman. (a) Arteriography with direct retrograde femoral artery injection. Arteriography reveals the presence of neovascularity and of a tumoral blush. (b) Coronal T1-WI. (c) Axial T2-WI. (d) Coronal T1-WI after IV administration of gadolinium contrast. MR shows a large inhomogeneous, intramuscular mass with multiple central areas with a hypointense signal on T1-WI which become hyperintense on T2-WI corresponding to intralesional necrotic areas. Strong enhancement at the periphery of the lesion is seen around the necrotic areas
15.3 WHO Classification of Pericytic (Perivascular) Tumors
Since imaging techniques lack specificity, it is not possible to classify tumors by their radiological appearance. For this reason we will classify the pericytic (perivascular) tumors on the basis of histology according to the WHO classification of soft tissue tumors ([12], Fourth revision).
Glomus Tumors (And Variants)
Benign
Glomus tumor
Glomangiomatosis

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree