Fig. 13.1
Scar tissue. (a) Transverse view through the calf 6 weeks after interruption of a venous tributary of the small saphenous vein (CHIVA 2). Left, proximal to the scar; right, at the level of the scar. It is obvious that the fascia has been opened and the saphenous fascia is not visible. The “scar cloud” (arrow) reaches the small saphenous vein where the muscle fascia was not opened. (b) Transverse view through the inner thigh 8 weeks after ligation of a venous tributary of the great saphenous vein. Left above, right at the level of the scar where the saphenous fascia is interrupted, but the muscle fascia remains intact. (c) Transverse view through the calf 2 months after stripping of the small saphenous vein up to the interrupted soleus perforating vein (formerly May). Left, empty fascial eye above the scar; centre, scar tissue where both fascias were opened; right, small saphenous vein in the fascial compartment distal from the scar. (d) Four months after stripping of the great saphenous vein. Transverse view through the inner thigh at a skin scar. Left slightly above; middle slightly below; right at the scar. Left, an echo-generating region with a weakened acoustic shadow visible in the intact fascial compartment which may correspond to a suture; middle, distal to the scar the remaining small saphenous vein can be seen in its compartment; right, shows how the scar tissue slowly degenerates and no longer generates as strong an echo as in (a–c) and the recovering connective tissue septa within the region of the scar (MV, muscle vein)
Copyright: [Author]
Recurrences can be detected early in scar tissue (de Maeseneer et al. 2005). It is therefore important to examine this tissue using colour duplex ultrasound (Fig. 13.2).
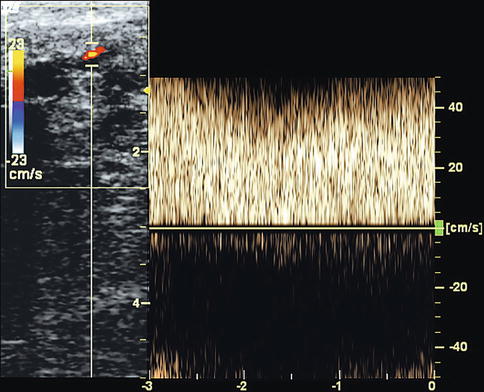
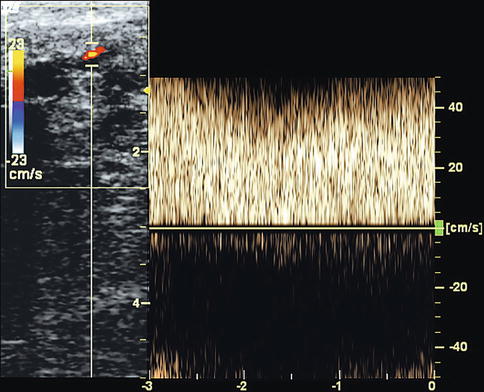
Fig. 13.2
Reflux from a sapheno-femoral junction venous tributary 2 months after crossectomy and stripping of the great saphenous vein in a 45-year-old man. He suffered with pains in the groin region with the appearance of new reticular varices in the outer thigh. A very small sapheno-femoral junction venous tributary is seen with high-velocity reflux in the region of the scar. This fills the anterior accessory saphenous vein which is dilated with very slow flow (see accompanying online material)
Copyright: [Author]
After a time, which may vary between 2 and 6 months in different patients, the original configuration of connective tissue is re-established. In this case this can only be recognised at the site of an operation if non-resorbable sutures or clips were used (Fig. 13.3a). Either an acoustic shadow is identified or the suture material is recognised directly as an echo-generating structure (Figs. 13.3b, d).
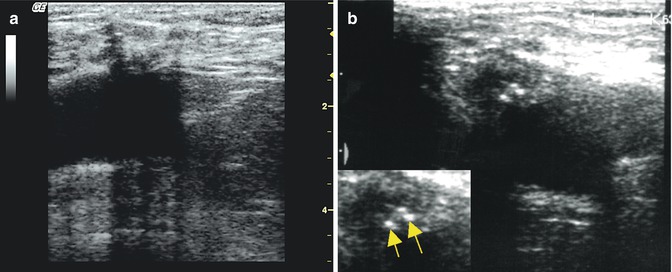
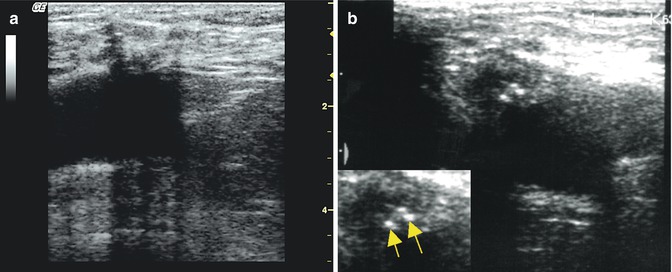
Fig. 13.3
(a) Longitudinal view through the groin 3 years after crossectomy showing the femoral vein and the completely re-established subcutaneous connecting tissue structures. Suture material can be identified indirectly by the resulting acoustic shadow. (b) Transverse view through the left groin 2 years after ligation of the sapheno-femoral junction which is magnified in the lower image. The non-resorbable suture can be recognised as two white points indicated by arrows. Suture material can obscure the colour signal with their sound shadow (see accompanying online material)
Copyright: [Author]
Documentation of the scar at early follow-up serves as proof that the target structure has been treated. This is relevant for CHIVA since with saphenous conservation treatments in the event of recurrence, the suspicion might arise that the vein was never touched (see below).
13.3 Post-intervention Follow-Up
13.3.1 Ultrasound After Stripping
In check-up examinations weeks to months after saphenous stripping, the following should be assessed and documented:
Operation at the junctions:
Is there a stump of great saphenous vein after an incomplete flush ligation (Figs. 13.4 and 13.8d)?
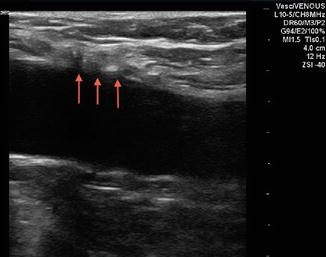
Fig. 13.4
Ultrasound of the sapheno-femoral junction after stripping. Longitudinal view through the groin showing the common femoral vein with the interruption point (arrowed) in the front wall. The front wall of the vein is smooth indicating a flush ligation (online material: image with flow)
Copyright: [Author]
Is there neovascularisation with reflux from deep veins (Fig. 13.2)?
Are there refluxive sapheno-femoral venous tributaries which form a tangle in the groin without necessarily bringing reflux from the deep leg veins? Later, these might reconnect and come into contact with refluxive epifascial veins.
Has the fascia in the popliteal fossa been closed?
Removal of the vein along its course:
Has the saphenous vein been removed between the intervening scars?
Is there a remaining vein within the fascial compartment or is the fascial eye empty (Fig. 13.1c)?
Interruption of perforating veins:
Are the formerly incompetent perforating veins still visible in the image?
Has any flow within these areas been documented using colour duplex?
Venous tributaries (treated or not):
Are areas of thrombosis found in the remaining venous tributaries (Chap. 11)?
Has any flow at the avulsion sites been documented using colour duplex?
13.3.2 Ultrasound After CHIVA
An ultrasound check-up examination is indispensable 6–12 weeks after CHIVA treatment since up to 20 % of patients require a supplementary operation before the treatment can be considered closed. This decision is based on clinical and ultrasound evidence.
Saphenous vein flow and diameter are documented and compared to their pre–operative findings. After ligation of the sapheno-femoral junction, there is a short-term retrograde flow during calf diastole (Fig. 13.5a). This is caused by drainage of the venous tributaries via the saphenous trunk and then into the deep veins through a distal perforating vein. After CHIVA 2 antegrade flow can be measured during calf systole (Fig. 13.5b). In cases of persisting great saphenous vein reflux, retrograde flow may be similar to or less than that documented prior to the operation. In this case a new perforating vein or venous tributary re-entry point must be found, and treatment of the sapheno-femoral junction may be indicated.
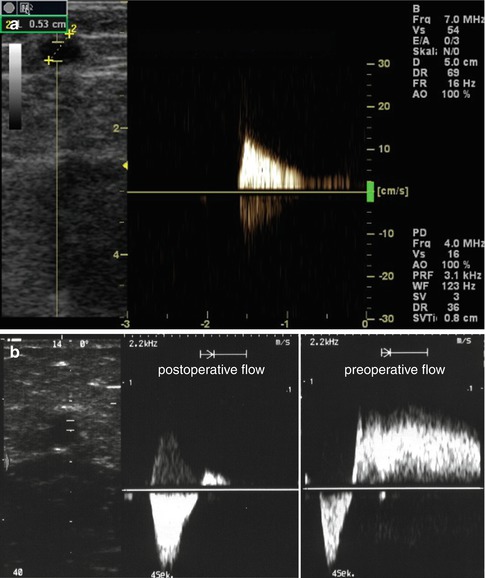
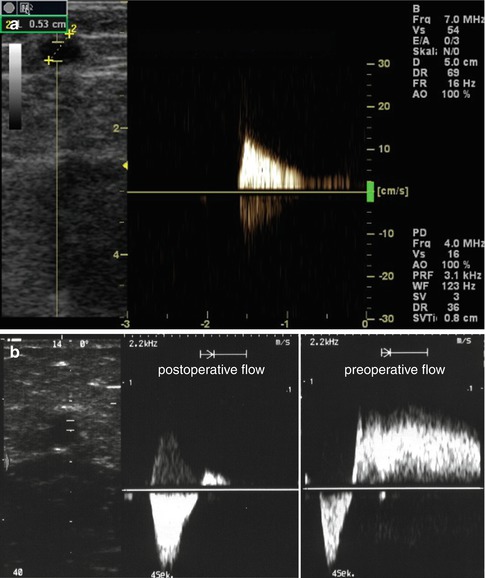
Fig. 13.5
Venous flow after CHIVA. (a) Flow during calf diastole in the great saphenous vein after ligation of the sapheno-femoral junction. The great saphenous vein diameter has reduced from 8.8 mm prior to the operation to 5.3 mm. (b) After CHIVA 2: left velocity profile at a subsequent examination demonstrating antegrade flow during calf systole and a limited short return flow until valve closure lasting approximately 300 ms and right velocity profile demonstrating a pre-operative comparison with antegrade flow during calf systole followed by reflux
Copyright: [Author]
In general, venous tributaries and saphenous veins must be examined for superficial thrombosis. Although this is usually asymptomatic after CHIVA, it delays the volume reduction in the tributaries. That means possible discomfort and a longer time until the final cosmetic result is achieved.
After ligation or crossectomy of the sapheno-femoral junction, post-operative flow in the groin must be monitored with special care and the absence or presence of a stump must be clarified (Fig. 13.6). The problem of a refluxing venous tributary at the sapheno-femoral junction which was not identified pre-operatively has already been discussed in Sect. 12.2 (Fig. 13.6b). A closed sapheno-femoral junction should be documented (Fig. 13.6a). A minimal drainage of the venous tributaries of the sapheno-femoral junction into the great saphenous vein is desirable as it prevents thrombus forming in the saphenous vein. If pre-operative reflux exists in the venous tributaries of the sapheno-femoral junction, this paves the way for a groin recurrence. This occurs through newly formed anastomoses 8 weeks after operation with the development of a long-term pathological reflux from the sapheno-femoral junction venous tributaries into the distal great saphenous vein.
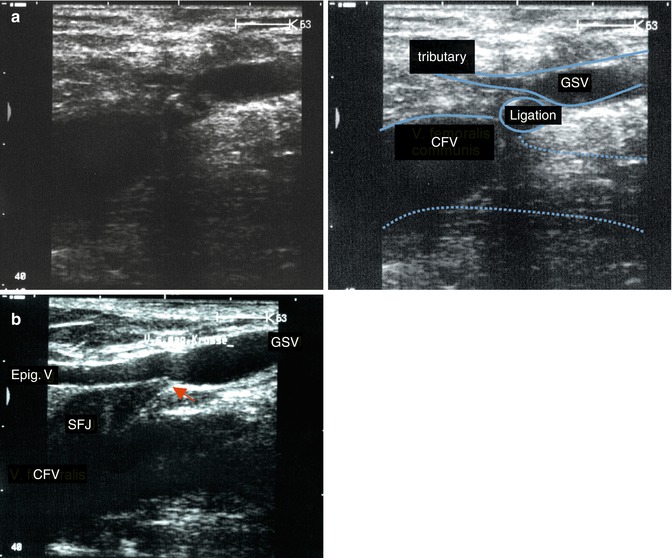
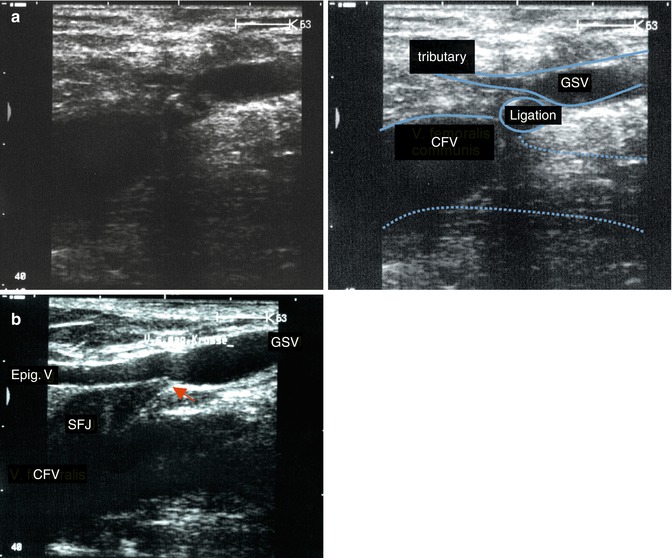
Fig. 13.6
Longitudinal view through the groin after ligation of the sapheno-femoral junction. (a) Correctly carried out double ligation appears as an oval, echo-poor element lying between the common femoral and great saphenous veins. The great saphenous vein receives a minimal antegrade flow from a competent venous tributary of the sapheno-femoral junction (Fig. 13.5a and c.f. Fig. 12.1). (b) Incorrect interruption of the sapheno-femoral junction. A single ligation has been performed directly below the junction of the superficial epigastric vein with the great saphenous vein at a distance of approx. 1 cm from the femoral vein (arrowed). The epigastric vein is pathological with continuous drainage into the great saphenous vein (see online material and c.f. Fig. 12.1)
Copyright: [Author]
After CHIVA 2 with ligation of a venous tributary for flow reversal in the saphenous vein, the operator must decide during post-operative examination whether the treatment has been completed (Sect. 12.2). If reflux persists, the stump must be reexplored. As in conventional sapheno-femoral junction ligation operations, a stump or a venous tributary can lead to recurrence (Fig. 13.7).
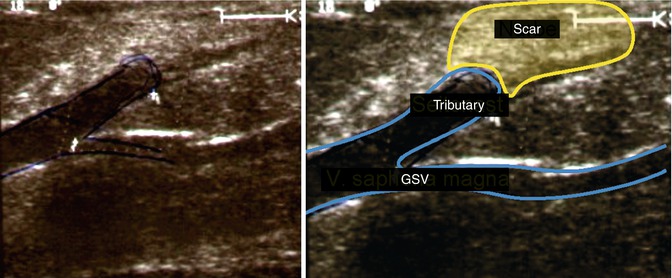
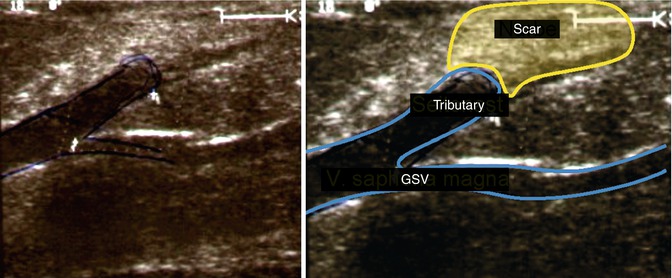
Fig. 13.7
Unsuccessful CHIVA 2 treatment with a great saphenous vein stump 1 cm long. Recanalisation and recurrent reflux are seen at this point (see accompanying online material)
Copyright: [Author]
In post-operative duplex ultrasound evaluations, the venous flow of remaining venous tributaries must be examined. If they present a high-volume, long-lasting reflux, an incompetence point must be sought. If the venous tributaries are only dilated but not refluxive, it may be concluded that the walls lack tone. They can be removed or treated by sclerotherapy.
13.3.3 Ultrasound After Extraluminal Valvuloplasty
Post-operative check-ups serve to ensure that the venous valve in the groin is functional. The check-up should be done between 2 and 4 weeks after surgery. Older valvuloplasty implants returned a strong echo making it impossible to take direct measurements in the confluence area. The image was completely obscured by acoustic shadowing. The new implants, available since 2007, are almost ultrasound neutral and allow haemodynamic measurements to be taken.
As with the old implants, the competence of the new venous valve in or below the groin must be tested using a Valsalva manoeuvre. The diameter of the great saphenous vein is determined at predefined points usually 5 cm below from the junction and 5 cm above the knee joint space. These measurement points were used for follow-up. In most cases the vein regained its competence with a reduction in diameter. In approximately 40 % of valvuloplasties, oscillating flow, backwards and forwards, is observed in the saphenous vein section after calf compression and release. This finding only defines true failure when, in addition, a positive reflux is found at the sapheno-femoral junction during a Valsalva manoeuvre.
13.4 Recurrence After Surgery on Varicose Veins
Recurrence of visible varicose veins after treatment is classically designated as recurrence. The REVAS classification was developed to describe this recurrence (Perrin et al. 2000). The cause of recurrence can be distinguished from the site of recurrence as listed below.
The cause of recurrence may be influenced by:
1.
Technical error
2.
Tactical error
3.
Neovascularisation
4.
Progression of the disease
5.
A combination of two or more of the above
6.
Unclear
The site of recurrence may be:
1.
Remaining stump of the great or small saphenous vein
2.
Pathological perforating veins (regardless of whether these were present previously or were treated)
3.
Remaining incompetent saphenous veins
4.
Development of incompetence in remaining veins which previously were competent
If visible varicose tributaries reoccur in a patient after a varicose vein operation, the diagnosing doctor must find the sources of reflux and treat them if appropriate. Duplex ultrasound is agreed in the international consensus document to be the best method (Nicolaides 2000). The clinically visible vessels must be examined by ultrasound to find the sources of reflux. The hidden course of the veins at the point of visible recurrence should be evaluated, especially in the region of surgical scars.
The work of Carandina et al. 2008 compared 54 legs in which the great saphenous vein was treated by stripping to 70 legs treated with CHIVA. The reflux visible on ultrasound was reported at 10 years and subsequently classified in Table 13.1.
Sources of reflux | Frequency after stripping (%) | Frequency after CHIVA (%) |
|---|---|---|
5.5 | 2.9 | |
Reflux from pelvic veins not connected to the common femoral vein | 3.7 | 1.4 |
Reflux from a perforating vein which was not noticeably refluxive before the treatment | 7.4 | 0 |
Reflux into a venous tributary from the great saphenous vein via the sapheno-femoral junction, a pelvic vein or healthy proximal venous tributaries | 0 | 18.5 |
Reflux into venous tributaries of diameter greater than 5 mm with no connection to a visible source of reflux | 22 | 0 |
Total | 35 | 18.5 |
13.4.1 Recurrence After Sapheno-femoral Junction Surgery
Recurrence at the sapheno-femoral junction can be divided into two groups:
1.
Reflux from deep veins
2.
Reflux from the sapheno-femoral junction venous tributaries without deep vein connections
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree