Fig. 8.1
Anatomic view of the upper respiratory system (cadaver model)
Technique of the Upper Airway US Examination
The optimal positioning of the patient for US examination of the upper airway is the “sniffing” position, which includes head extension and neck flexion. If this position is not possible to perform due to reasons such as a cervical spine injury, the mandible needs to be moved into protrusion. This maneuver requires the help of an assistant. Two main planes are usually used for the US examination: horizontal, also called transverse view, and sagittal plane, called longitudinal view. Transverse view is mostly used for the US assessment of the mouth floor, posterior part of the tongue (Fig. 8.2), and supra- and infra-hyoid bone regions. For the US assessment from larynx to the suprasternal notch, both views can be used, depending on the clinical needs. According to the anatomy of the patient, any other plane can be used as long as the structures under the US probe are discerned. Besides the planes where the US probe should be at 90° in relation to skin (e.g., transverse and longitudinal), there are four different movements of the US probe which can be useful to get a better view on the screen:


Fig. 8.2
Tongue ultrasound view—posterior part. White arrow (tongue)
Sliding—longitudinal or transverse US probe movement over the skin surface without changing angle of the US probe in relation with the skin surface.
Rotation—around the vertical axis of the US probe without any lateral movement. Usually used to distinguish muscles, tendons, blood vessels, and nerves from other structures.
Tilting—manipulating the US probe about its horizontal axis thereby changing the angle of the US wave in relation to the skin surface, but without longitudinal or transversal movement across the skin surface. The best US screen view usually appears when the US wave comes at a 90° angle to the skin surface; it nevertheless does not mean that all structures in the neck are parallel with skin. Therefore, tilting is the maneuver which corrects the entrance of the US wave into target organs, intending to get the best US screen view.
Pressure—moderate force applied with the US probe on the underlying tissue at 90° angle to the skin surface. This maneuver can be helpful to differentiate arteries from veins.
A short linear US probe with a frequency of more than 7.5 MHz is appropriate for the upper airway US examination, due to the higher frequency, which gives a better resolution of the superficial organs and tissues. For this examination, the best selected setting on ultrasound apparatus is the small parts or vascular setting.
Image Acquisition and Interpretation
US Anatomy of the Upper Airway
An US probe with a frequency of more than 7.5 MHz is appropriate for the upper airway US examination, due to the higher frequency, which gives a better resolution of the superficial organs and tissues. In spite of the high impedance of air-filled spaces, analysis of the soft tissue and cartilages of the upper airway is possible, including: the floor of the mouth, posterior part of the tongue, supra- and infra-hyoid bone region, larynx, and trachea. The US examination of the floor of the mouth usually includes the posterior part of the tongue and its base, which presents the tongue as an iso- to hypoechoic organ (Fig. 8.2). Epiglottic vallecula is well visualized from both sides of the tongue base, and it is considered to be a margin to hypopharynx (Fig. 8.3). Moving the US probe from the mouth floor caudally (sliding) in the transverse view, the hyoid bone with characteristically inverted U-shaped hyperechoic line (reflection of the US wave) and the acoustic shadow underneath can be assessed (Fig. 8.4). The hyoid bone and nearby laryngeal cartilages are clearly visible due to its bony structure. By further sliding of the US probe caudally, the main laryngeal cartilages (cricoid and thyroid) can be assessed. Although a median approach of the US probe is the best one for the US examination of the upper airway anatomy, para-medial approach would be preferable in the area of the laryngeal prominence, since there is no perfect contact between the US probe and skin. Thyroid and cricoid cartilages are visible as homogeneous, hypoechoic well-defined structures, connected with iso-echoic crico-thyroid ligament. Vocal cords can be assessed by the transverse view by positioning the US probe on the distal part of the thyroid cartilage or on the crico-thyroid membrane caudally and tilting the US probe (Fig. 8.5). Vocal cords are visible as hypoechoic structures and appear as triangle movement during phonation. Approximately half of the length of the trachea is positioned in the neck and is available for US analysis. Caudally from the cricoid cartilage, imperfect tracheal cartilage rings appear and can be assessed by longitudinal and transversal view. Cartilage rings are clearly visible as hypoechoic, well-defined, lens-shaped structures. Between tracheal cartilages and tracheal air-filled space, there is a hyperechoic line, which is called the air-mucosa interface. Sliding in a caudal direction, anterior to the trachea at the level of second to fourth tracheal cartilage, a homogeneous hyperechoic structure (in comparison with adjacent strap muscles) can be seen. This structure serves as a bridge connecting two identical echoic oval structures anterolateral to the trachea, which represent the isthmus and two lobes of the thyroid gland. Transverse view of the trachea is usually used to examine the width of the air space at different levels of the view and also to measure the width of the soft tissue from trachea to the skin surface (Fig. 8.6). The longitudinal view in the median or para-median plane is suitable for showing the line of tracheal cartilages, and their number as well (Fig. 8.7). Via the longitudinal midline view, the distance from the skin surface to the anterior cartilage, as well as the distance from the posterior cartilage to the tracheal air space, can be estimated.




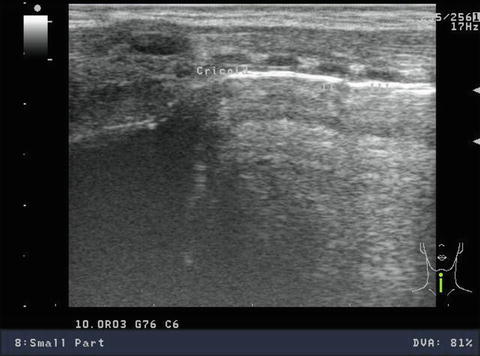

Fig. 8.3
Ultrasound view of the vallecula epiglottica (arrows)

Fig. 8.4
Ultrasound view of the hyoid bone (arrow)

Fig. 8.5
Ultrasound view of the vocal cords (arrows)

Fig. 8.6
The air space of the trachea and the pretracheal soft tissue—transverse view
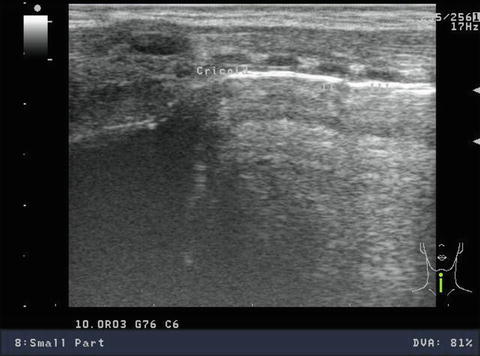
Fig. 8.7
Tracheal cartilage rings—longitudinal view
Verification of Endotracheal and Double-Lumen Tube Position
When focusing on methods of definitive airway protection and control in critically ill patients, endotracheal tube (ETT) insertion persists as the primary one. In order to exclude esophageal or endobronchial intubation, with respect to the Advanced Cardiac Life Support guidelines from 2000, a confirmatory procedure should be undertaken after the insertion of the ETT [5]. Furthermore, the position of the ETT tube must be constantly supervised during patients’ stay in ICU so that incidental endobronchial intubation, with subsequent atelectasis, is forestalled. Even though the physical examination comprising mainly auscultation of the left thoracoabdominal area is advised to be the firsthand and everyday method of ETT positioning confirmation, its sensitivity is nevertheless considerably low, which consequently points out the necessity of a secondary method of confirmation. The end-tidal CO2 detection and esophageal suction device are the most often used bedside ones, but both of these secondary methods are firstly limited in detecting endobronchial intubation, and secondly they do not render direct anatomic evidence of accurate ETT position [6].
On the other hand, US provides indirect but proper dynamic anatomic evidence of the correct physiologic function of the ETT in paralyzed or apneic patients during and after resuscitation; moreover, it effectively and quickly images the movement of the diaphragm and pleura, both of them being the indirect quantitative and qualitative indicators of lung expansion [3, 7]. If the ETT is in the correct position (i.e., trachea), bilateral and equal motions of the diaphragm toward the abdomen are likely to be visible on ultrasound, representing equal bilateral expansion of the lungs [7, 8] (see Chap. 10 for a complete discussion of diaphragm ultrasound imaging). When using the intercostal ultrasonographic view, it is also easy to identify the “sliding lung” sign at the lung-chest wall interface, a sort of “to-and-fro” movements of the hyperechoic pleura synchronized with ventilation (see Chap. 9) [9]. If the aforementioned sign is imaged on the left, or on both sides of the chest, it should correspond to appropriate bilateral lung ventilation, thus verifying correct ETT position. In contrast, if the ETT is in the esophagus, expansion of the lungs will not occur as a result of mechanically delivered breath, but diaphragmatic movement may be seen if the patient continues to spontaneously breathe. Furthermore, when the patient is paralyzed or apneic, an esophageal intubation will result in an immobile diaphragm or paradoxical movement of the diaphragm (due to the instillation of positive pressure into the abdomen). An intercostal view in paralyzed or apneic patients with an intra-esophageal ETT will result in absence of motion of the pleura on both sides of the chest (i.e., absence of “lung sliding”) with assisted ventilation. When the “lung sliding” sign is absent, the vibrations of the pleura will occur in rhythm with the heartbeat, a sign known as the “lung pulse” (see Chap. 9) [10]. Finally, it will be either impossible to see the movements of the left diaphragm—or the movement is significantly minimized—when the tube is in the right main bronchus; the movements of pleura (“lung sliding),” on the other hand, will occur only on the right side of the chest, while the “lung pulse” should be visible on the left side. As an important reminder, the presence of lung sliding indicates lung inflation and the absence of pneumothorax, but, as is evident in these examples, the absence of lung sliding does not necessarily indicate the presence of a pneumothorax.
In adults, successful imaging of the ETT correctly placed in the trachea can be variable (Fig. 8.8). There have been limited reports of additional methods that can augment one’s ability to capture the ETT position with US, such as increasing the echogenicity of the tube by retaining a stylet in the tube or by filling the ETT cuff with fluid and air bubbles. In contrast, in children, and especially in infants, correct anatomic position of ETT can be visualized by bedside US in almost all cases [11]. Furthermore, in emergency settings US is highly useful in detection of the esophageal malposition of ETT, since it is possible to verify esophageal position of ETT in nearly all patients within just a few seconds [12].


Fig. 8.8
Endotracheal tube placement in the trachea
In the case of a thoracic procedure or one-lung ventilation, the purpose of using double-lumen tubes (DLT) is to both isolate and/or collapse a given lung. The placement of a DLT must always be accurate in order to prevent injury to a patient or endangerment of the procedure. The current methods used to confirm the DLT placement are auscultation and fiberoptic bronchoscopy (FOB)—neither of which is optimal. Auscultation is not fully dependable and appropriate to confirm the correct position of the DLT, and FOB is not always available in clinical practice, particularly for the narrow DLTs used for children or small stature patients. Moreover, blood or mucus in the airway and anatomical distortion complicate the confirmation of DLT position, making visualization more difficult or even impossible. In these, albeit rare, cases, the FOB fails to guarantee success and positioning problems and severe complications can occur; therefore, US is a new and highly useful tool for confirming the proper DLT placement. The utility of US in confirming the proper DLT position is identical to the verification of endotracheal position of ETT. Movements of the right diaphragm will not be visible or will be significantly reduced if the left DLT has been placed in the correct position (i.e., left main bronchus). The pleural movements (“lung sliding”) will be seen only on the left side of the chest, while the “lung pulse” will be visible on the right. If the DLT is placed in the trachea, bilateral equal movements of the diaphragm toward the abdomen and bilateral “lung sliding” can be observed [13].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree