Fig. 37.1
The laparoscopic ICG fluorescent imaging system (Karl Storz GmbH & Co. KG, Tuttlingen, Germany)
(a) High-end full high-definition camera system (IMAGE 1 SPIESTM, Karl Storz)
(b) Laparoscope (HOPKINS®II ICG telescope, Karl Storz)
(c) Foot switch
37.3 Role of ICG Fluorescence Imaging in Laparoscopic Liver Resection
37.3.1 Identification of Anatomic Domain in the Liver
37.3.1.1 Background
Systemic removal of a segment-oriented territory confined by tumor-bearing portal tributaries was reported to be essential in radical resection of hepatocellular carcinoma (HCC) [16]. Parenchymal-sparing anatomic liver resection is often selected for patients with chronic liver impairment. Identification of the boundaries of hepatic sections or segments is usually done by means of ischemic demarcation followed by selective occlusion of the hepatic portal pedicle, with or without mapping with blue dye staining-guided intraoperative ultrasound [1, 17]. However, these strategies sometimes result in inadequate visualization of the stained domain, especially in cirrhotic liver. Aoki et al. [18] reported that ICG fluorescent mapping identified the stained hepatic domain in more than 90 % of patients undergoing open anatomic liver resection and that the techniques was successful even against the background of liver cirrhosis. A recent report by Sakoda et al. [19] indicated that this technology was useful during LLR.
37.3.1.2 Mechanism
Liver parenchyma fluoresces due to uptake by Kupffer cells within 2–3 min after intravenous injection of 0.5 mg/kg dilute ICG solution, the same dose used for preoperative evaluation of hepatic functional reserve.
37.3.1.3 Method
In anatomically oriented liver resection, the fundamental technique involves selective occlusion of the portal pedicles of the liver parenchyma, using a Glissonean approach or individual isolation of hepatic inflow vessels before hepatic parenchymal transection [1, 20]. ICG is administered intravenously after selective vascular occlusion is achieved. Consequently, the inflow-preserved liver area is fluorescent, and ischemic area is discolored as counterstaining fashion.
37.3.1.4 Case Presentation
Case description: Hepatocellular carcinoma and liver cirrhosis in segment 6 in a 56-year-old male. The patient underwent LLR of segment 6. The Glissonean sheath to segment 6 was isolated and ligated before liver parenchymal transection. After administration of ICG, the fluorescent imaging system allowed clear identification of the territory of the Glissonean sheath to segment 6 as an ischemic area (Fig. 37.2a–b). Liver resection was performed along the fluorescence boundary on the liver surface and parenchyma (Fig. 37.2c). After hepatic parenchymal transection, the entire resection plane was visualized as a fluorescence-emitting plane (Fig. 37.2d).
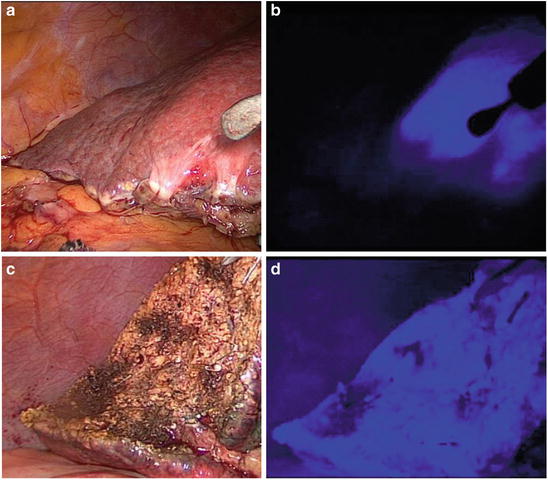
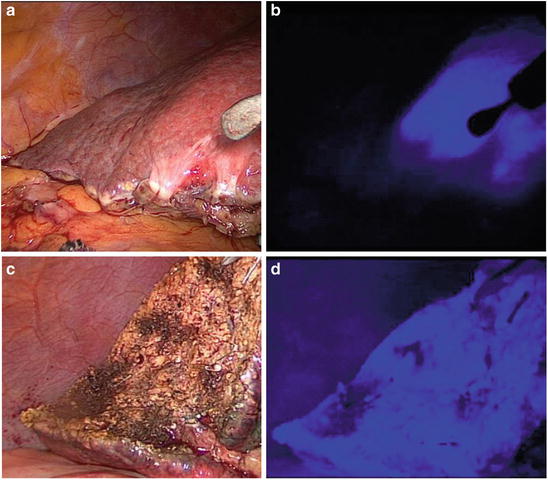
Fig. 37.2
Identification of anatomic domain in the liver
(a) After ligation of the Glissonean sheath to segment 6, the demarcation area is observed under white light
(b) After ICG administration, the territory of the Glissonean sheath of segment 6 is clearly visualized, after counterstaining, by the fluorescent imaging system
(c) LLR of segment 6 was performed along the fluorescence boundary on the liver surface and interior
(d) After hepatic parenchymal transection, the entire plane of resection is visualized as a fluorescence-emitting plane
37.3.1.5 Assessment
The inflow-occluded area usually appears as an ischemic demarcation on the liver surface but is not always clearly visible during surgery, especially in cases of liver cirrhosis associated with portal hypertension, which leads to turbulent portal flow [21]. Similarly, the inflow-occluded area on the liver surface may also be indistinct after adhesiolysis. In our experience, these trends are obvious when visible white light is used during conventional endoscopy. Thus, ICG fluorescent imaging may be beneficial and sensitive in identifying anatomic segmentation in the liver surface achieved by a control portal pedicle in the laparoscopic setting. The distribution of ICG fluorescence can be identified even inside the liver. In our experience, navigation using the ICG system would make easier to reveal the orientation of anatomic boundaries within the liver parenchyma, compared with observation of ischemic discoloration or dye staining. Thus, ICG fluorescence staining could help address the main limitation of LLR—its difficulty in determining anatomic orientation due to its reliance on a two-dimensional magnified view.
37.3.2 Detection of Liver Tumors
37.3.2.1 Background
In open liver surgery, the location and extent of tumors are usually determined by visualization and surgical palpation, with ultrasound assistance. However, macroscopically unidentifiable, small, subcapsular lesions might be missed even in open procedures. Ishizawa et al. reported that ICG fluorescent imaging, with preoperative ICG administration, enables highly sensitive detection of small and grossly unidentifiable liver cancers near the liver surface, through visualization of uptake and abnormalities in biliary excretion of ICG in cancer and noncancerous liver tissues. They concluded that this technology enhanced the accuracy of liver resection and operative staging [13].
A disadvantage of laparoscopic surgery is the limited ability to palpate the tumor. The recent development of laparoscopic ICG fluorescence imaging may compensate for this limitation in the diagnosis of hepatic malignancy during LLR. Satou et al. [22] reported that extrahepatic metastases from HCC emitted fluorescence on ICG fluorescent imaging. As compared with open procedures, inspection of the whole abdomen is often easier when done laparoscopically. Therefore, ICG fluorescence imaging should be more often utilized in laparoscopic surgery.
37.3.2.2 Mechanism
Although the precise mechanism of ICG accumulation in liver tumors is unknown, Ishizawa et al. found that well-differentiated HCC tissues take up ICG during preoperative administration, although biliary excretion of ICG is impaired in HCC because of morphologic or functional abnormalities. In contrast, poorly differentiated HCC and metastatic liver cancers do not take up ICG. However, such tumors can be visualized as rings of fluorescence, which result from impaired bile excretion in surrounding nontumorous tissues that are compressed by tumors [13, 23]. Using a fluorescence microscope, they also noted ICG fluorescence in the cytoplasm and pseudoglands of well-differentiated HCCs. Fluorescence was also seen in nontumorous liver tissue compressed by tumors in cases of poorly differentiated HCC and colorectal cancer metastases, as in the abovementioned macroscopic findings [24]. This variation in enhancement pattern may be caused by varied expression of organic anion-transporting polypeptide 8 [25].
37.3.2.3 Method
Within the 2 weeks before surgery, 0.5 mg/kg of ICG (Diagnogreen; Daiichi Sankyo, Tokyo, Japan) is administered intravenously for preoperative evaluation of hepatic functional reserve. The entire abdomen, including the liver, is inspected with the ICG fluorescence imaging system during surgery.
37.3.2.4 Case Presentation
Case description: Multiple recurrent HCC in the left lateral section, 3 years after partial resection of segment 3 for initial HCC, in a 79-year-old female with Child B liver cirrhosis. Macroscopic cirrhosis with multiple regenerative nodules was observed with the visible white light mode of the laparoscope; however, no tumors were clearly visible on the liver surface (Fig. 37.3a). After introduction of the fluorescence imaging, multiple subcapsular tumors were resected (Fig. 37.3b). No other emission-suspected extrahepatic metastasis was seen in the abdomen. Laparoscopic left lateral sectionectomy was performed. Pathologic analysis of the specimen showed well-differentiated HCC.
Fig. 37.3
Detection of liver tumors
(a) Macroscopic cirrhosis with multiple regenerative nodules as visualized in visible white light mode. The tumors are not clearly visible from the liver surface
(b) Fluorescence imaging reveals multiple subcapsular tumors, which were later resected
37.3.2.5 Assessment
Kudo et al. [26] described the sensitivity of laparoscopic ICG fluorescence imaging in 12 HCCs (75 %) and 11 liver metastases (69 %) on the liver surface, which were distributed over Couinaud segments 1–8, including tumors unidentifiable by white light. However, inability to visualize tumors ≥8 mm from the liver surface is a major limitation of ICG fluorescence imaging in open and laparoscopic procedures [13]. Therefore, intraoperative ultrasound remains an indispensable diagnostic tool for assessment of liver tumor, including deep lesions.
False-positive emission is another concern in the detection of liver malignancies. Morita et al. reported and noted very small emission spots on the liver surface and cut plane. Pathologic examination showed that these emissions were derived from a dysplastic nodule, liver parenchyma, bile plug, and cyst [27]. Tanaka et al. suggested that ICG might accumulate in regenerative nodules [28]. The many false-positive emissions are believed to be due to severe liver function disorder and biliary excretion disorders [13, 28–30], which are frequently seen in cirrhotic liver.
Ishizawa et al. demonstrated that the signal intensity of noncancerous liver parenchyma was higher in patients with an unfavorable ICG retention rate and in patients who had received an ICG injection within the 24 h before surgery [13]. They proposed that an interval longer than 2 days might be necessary in order to obtain good lesion-to-liver contrast, especially in patients with advanced cirrhosis [31].
37.3.3 Visualization of Biliary Leakage
37.3.3.1 Background
Postoperative bile leak is a common complication (up to 10 % of cases) [32–34] and can worsen outcomes after liver surgery, even in the modern era [32, 33]. For the best outcome, bile leakage should be detected intraoperatively; however, a randomized trial found that use of a bile leak test requiring injection of saline solution through the cystic duct offered no advantage [34], probably because of the transparency of saline. Intrabiliary injection of dyes such as methylene blue [35] and ICG [33, 36] has also been attempted, but these dyes can densely stain tissue and complicate repeat inspection. A randomized control trial [14] found that ICG fluorescent cholangiography was useful in detecting bile leakage not detected on a leak test using saline. Sakaguchi et al. [15] reported that ICG fluorescent cholangiography was sufficiently sensitive to identify bile leakage.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree