Vascular Disorders of the Spine and Spinal Cord
Anton Valavanis
Robert W. Hurst
Vascular diseases of the spine and spinal cord comprise a rare but important group of conditions affecting this critical portion of the central nervous system (CNS). Among the group of neurovascular pathologic conditions, the group of vascular disorders of the spine and spinal cord comprises approximately 2% and includes spinal cord ischemia of various etiologies and a spectrum of vascular malformations. In addition, hemangioblastomas of the spinal cord are highly vascularized neoplasms which may mimic morphologically an arteriovenous malformation (AVM) of the spinal cord. Complete evaluation of patients with potential spinal vascular disease is a significant and often difficult task for all physicians involved in the diagnosis and treatment of disease of the spine. Magnetic resonance imaging (MRI) including magnetic resonance angiography (MRA) represents the most important single source of diagnostic information regarding spinal anatomy and pathology and is particularly important in the evaluation of the patient with possible spinal vascular disease. However and despite its invasiveness, spinal digital subtraction angiography (DSA) is an essential, additional tool for the detailed angioarchitectonic evaluation, classification and treatment planning in cases with AVMs of the spinal cord.
A thorough familiarity with the normal vascular anatomy of the spine and spinal cord is essential for complete understanding and proper interpretation of MRI in spinal vascular disease. Just as critical is an appreciation of the varieties of vascular pathology that may afflict the spine and cord and an acquaintance with clinical situations that warrant consideration of these entities. Finally, an understanding of the strengths and limitations of MRI and MRA in spinal vascular disease aids in formulating a diagnostic evaluation plan and assists in determining which patients require additional evaluation including spinal DSA.
Vascular Anatomy
Knowledge of the complex vascularization of the spinal cord and its surrounding tissues including the arterial supply and the venous drainage is essential for the interpretation of spinal MRI and MRA as well as for the performance and diagnostic analysis of spinal DSA when evaluating patients with suspected vascular disease of the spine and/or spinal cord. The supply of the spine and spinal cord is provided by a bilateral, symmetrical, longitudinally arranged segmental system of arteries, that is, the segmental arteries. These segmental arteries originate at the cervical level from the vertebral, ascending, and deep cervical arteries, at the thoracic level from the thoracic aorta as the intercostal arteries, at the lumbar level from the lumbar aorta as the lumbar arteries and at the sacral level from the internal iliac arteries as the iliolumbar arteries. Each segmental artery provides distinct branches for the supply of the vertebral bodies, the paraspinal musculature, the dura, the nerve roots and the spinal cord. The nerve roots, the dura and the cord are supplied from the spinal radicular branch, which courses through the intervertebral foramen.
The spinal cord receives its blood supply from the longitudinal anterior spinal artery (ASA) and the paired posterior spinal arteries (PSAs). The ASA results from the midline fusion of the paired ventral paramedian located longitudinal neural arterial axes, which takes place during embryonic development. The most cranial extent of the ASA originates as separate lateralized branches from the intradural vertebral arteries at the cervicomedullary junction. A single-midline ASA is formed, which courses along the ventral surface of the spinal cord adjacent to the anterior median fissure. The longest artery in the body, the ASA is usually continuous along the entire length of the spinal cord.
Predictable variations in caliber of the ASA occur along the length of the cord reflecting variations in metabolic requirement of the various cord regions. The relatively large amounts of gray matter found within the cervical and lumbar enlargements require a larger blood supply than the white matter tracts of the cord. Consequently, the larger size of the ASA in the lower cervical and lumbosacral regions, often exceeding 1 mm in diameter, reflects this relatively large blood flow requirement. The ASA often narrows to less than 0.5 mm in diameter in the thoracic region between T2 and T9, where the cord is largely composed of white matter tracts and the metabolic demand is correspondingly low (1,2).
Each spinal nerve root receives its blood supply from a radicular artery, which follows the root within the neural foramen. The radicular artery supplies the root sleeve and spinal dura and also gives supply to the vertebra at each level (Fig. 23.1). The majority of the radicular arteries give no supply to the spinal cord itself. At various locations along the length of the cord, however, branches from the radicular arteries contribute to both the ASA and PSA. Radicular artery branches contributing to the ASA are referred to as “radiculomedullary” arteries, and those giving supply to a PSA are known as “radiculopial” arteries (Fig. 23.2).
From six to eight radiculomedullary arteries arise from radicular arteries along the length of the cord. Radiculomedullary arteries follow the nerve root through the neural foramen and bifurcate on the ventral surface of the cord near the midline into ascending and descending branches that join the ASA (3). The locations of radiculomedullary arteries along the cord follow general guidelines based on the cord blood flow requirements at various levels. Nevertheless, considerable individual variation exists in the location of radiculomedullary arteries.
 FIGURE 23.1 Diagram of the intercostal arterial system. (1) Arteries to the vertebral body, (2) anterolateral anastomotic artery, (3,4) pretransverse anastomoses, (5) dorsospinal artery, (6,8) ventral muscular branches, (7) ventral branch, (9,10) dorsal muscular branches, (11) radicular artery, (12,14) epidural anastomoses, (13) dural branch. (From Lasjaunias P, Berenstein A. Surgical Neuroangiography. Volume 3: Functional Vascular Anatomy of Brain, Spinal Cord, and Spine. New York: Springer-Verlag, 1990, with permission.) |
Clinical consideration of the spinal cord blood supply is aided by the concept of three major regions of supply to the ASA axis (4) (Fig. 23.3). The three regions include the cervicothoracic, midthoracic, and thoracolumbar regions. Hemodynamic watershed areas occur at the margins of each region as flow through the ASA in one region encounters opposing ASA flow from the adjacent region. Little net flow normally occurs across the border zone, resulting in relative hemodynamic isolation of the ASA supply of each region from its neighbor. Although the ASA is usually continuous anatomically along the length of the spinal cord, adequate collateral flow across border zones is not always available. This is especially frequent in the midthoracic region, where the ASA may be relatively small. The spinal cord is, therefore, vulnerable to infarction in the event of compromise of a radiculomedullary feeding vessel or of hypotension affecting the ASA (5).
In the cervicothoracic region, radiculomedullary contributions to the ASA may originate from the vertebral artery as well as from branches of the costocervical or thyrocervical trunks. In most cases, the ASA receives a radiculomedullary branch from the vertebral artery at approximately the C3 level. In addition, a relatively constant radiculomedullary vessel, the artery of the cervical enlargement, is usually found accompanying the C6 nerve root.
 FIGURE 23.2 Superficial arteries of the spinal cord: (1) radicular artery, (2) radiculomedullary artery (to anterior spinal artery), (3) radiculopial artery (to posterior spinal artery), (4) anterior spinal artery, (5) posterior spinal artery, (6,7) circumferential pial arterial plexus, (8) sulcocommissural arteries. (From Thron A. Vascular Anatomy of the Spinal Cord. New York: Springer-Verlag, 1988:114, with permission.) |
 FIGURE 23.3 Diagram of the arterial regions of the spinal cord. (I) Superior or cervicothoracic region, (II) intermediate or midthoracic region, (III) lower or thoracolumbar region. (1) Anterior spinal artery, (2) artery of the spinal enlargement (variable), (3) posterior spinal artery, (4) artery of the lumbar enlargement (artery of Adamkiewicz), (5) anastomotic loop of the conus medullaris with continuation of the anterior spinal artery as the artery of the filum terminale. (From Lazorthes G, Gouaze A, Zadeh JO, et al. Arterial vascularization of the spinal cord: recent studies of the anastomotic substitution pathways. J Neurosurg 1971;35:253–262, with permission.) |
The midthoracic region, consisting of the next six or seven cord segments, has a lower metabolic demand and demonstrates a correspondingly smaller blood supply. Often only one radiculomedullary artery, usually accompanying the T4 or T5 root, occurs in this region.
The thoracolumbar region, extending from the T8 segment to the conus medullaris, is provided with a relatively rich blood supply, usually originating from a single large radiculomedullary artery. This vessel, described by Adamkiewicz as the “arteria radicularis anterior magna,” is also known as the artery of Adamkiewicz (Fig. 23.4). In 75% of cases, the artery of the lumbar enlargement enters the spinal canal at a level from T9 through T12, most commonly on the left, whereas in 10%, the vessel accompanies the first or second lumbar nerves. The artery has a high origin in 15%, entering at levels from T5 through T8. Although general guidelines exist for the location of this important radiculomedullary artery, the location in a given patient is variable, ranging from the upper lumbar through midthoracic levels.
Like the ASA, the cranial extent of the paired PSAs usually originates from the intradural vertebral arteries. The PSAs, whose caliber is more uniform and usually smaller than that of the ASA, course on the dorsal surface of the cord adjacent to the dorsal roots. These features of the PSAs reflect their area of spinal cord supply, which includes mostly the dorsal white matter tracts and demonstrates little variation in size or metabolic requirement from one cord level to another.
Frequent intercommunications connect the two PSAs across the dorsal cord surface. In contrast, collaterals around the lateral surface of the cord are infrequent and too attenuated to function reliably as anastomoses between the territories supplied
by the ASA and PSAs. The absence of adequate collaterals results in functional and anatomic isolation between these two major territories of spinal cord vascular supply.
by the ASA and PSAs. The absence of adequate collaterals results in functional and anatomic isolation between these two major territories of spinal cord vascular supply.
 FIGURE 23.4 Variations in the location of the artery of the lumbar enlargement. (1) Ascending branch of the anterior spinal artery, (2) artery of the filum terminale, (3,4) artery of the lumbar enlargement, (5) sacral arteries. Percentages refer to the occurrence of the artery of the lumbar enlargement at specific spinal levels. (From Lazorthes G, Gouaze A, Zadeh JO, et al. Arterial vascularization of the spinal cord: recent studies of the anastomotic substitution pathways. J Neurosurg 1971;35:253–262, with permission.) |
At variable locations along the length of the cord, the PSAs receive contributions from radiculopial branches of the radicular arteries. From 10 to 20 radiculopial arteries may be present, each one joining a PSA but making no contribution to the ASA.
Intrinsic Spinal Cord Supply
Two distinct groups of arteries, the sulcocommissural arteries and the rami perforantes, provide blood supply directly to the neural tissue of the cord (Fig. 23.5). The sulcocommissural arteries, a lateralized, centrally directed system of perforating arteries, originate from the ASA. The sulcocommissural arteries course dorsally within the anterior median fissure before turning left or right to enter the cord in the region of the anterior white commissure (Fig. 23.6). Dense capillary networks from the sulcocommissural arteries originate within the cord substance to supply the gray matter of the anterior, intermediate, and basal dorsal horns as well as most of the white matter within the anterior and lateral funiculi.
A separate system of centripetally directed arteries known as rami perforantes receives its supply mainly via the PSAs. The rami perforantes supply the peripheral structures of the cord including the posterior columns and the apices of the dorsal horns. A minimal amount of gray matter is supplied by the rami perforantes in comparison to that supplied by the sulcocommissural arteries (Fig. 23.7).
The inadequate anastomoses between the ASA and PSA territories result in anatomic and functional separation between the two intrinsic cord vascular distributions. The anterior 60% to 80% of the spinal cord receives supply exclusively from branches of the ASA, whereas the posterior 20% to 30% is fed by rami perforantes originating from the PSA.
The intrinsic veins of the spinal cord collect blood in a radially symmetric pattern. On reaching the surface of the cord, venous blood collects into the longitudinally directed anterior and posterior spinal veins (Fig. 23.8) (6). Both longitudinal venous systems, that is, the anterior and posterior, are interconnected by a circumferential, superficial pial venous network as well as by direct transmedullary venous anastomotic channels. The transition from a median spinal vein into a radicular vein has the same hairpin configuration as the corresponding radiculomedullary artery. At multiple levels, radicular veins drain the anterior and posterior spinal veins into the epidural venous plexus which is connected to the azygos and hemiazygos venous systems.
 FIGURE 23.5 Superficial and intrinsic arteries of the spinal cord. (1) Anterior spinal artery, (2) posterior spinal arteries, (3) sulcocommissural arteries, (4) circumferential pial arterial plexus. (From Lazorthes G, Gouaze A, Zadeh JO, et al. Arterial vascularization of the spinal cord: recent studies of the anastomotic substitution pathways. J Neurosurg 1971;35:253–262, with permission.) |
 FIGURE 23.6 Sulcocommissural branches (4,5,6,7) of the descending branch of the anterior spinal artery (3) penetrate the cord in the anterior median fissure. Both the descending and ascending (2) branches of the anterior spinal artery are supplied by a radiculomedullary artery (1). The axial (8,10,11) and longitudinal (9) distribution of the sulcocommissural arteries is shown. (From Lasjaunias P, Berenstein A. Surgical Neuroangiography. Volume 3: Functional Vascular Anatomy of Brain, Spinal Cord, and Spine. New York: Springer-Verlag, 1990, with permission.) |
 FIGURE 23.8 Intrinsic and extrinsic veins of the cord. (1,2,3) Intrinsic venous anastomoses, (4) sulcal vein, (5) transmedullary anastomoses, (7) ventral spinal cord vein, (6,8,9) extrinsic anastomoses, (10) radial vein. (From Lasjaunias P, Berenstein A. Surgical Neuroangiography. Volume 3: Functional Vascular Anatomy of Brain, Spinal Cord, and Spine. New York: Springer-Verlag, 1990, with permission.) |
Evaluation of Vascular Lesions of the Spine and Spinal Cord
MRI permits noninvasive evaluation of spinal cord anatomy and many types of spine and spinal cord pathology. Although spinal angiography remains the best method for detailed visualization of the spinal vasculature, both MRA and computed tomography angiography (CTA) using multi-detector CT have been able reliably to detect the normal artery of the lumbar enlargement (artery of Adamkiewicz) (1,2,4,7,8,9,10,11,12).
Nijenhuis et al. (11) evaluated 15 patients having suspected spinal cord vascular pathology with both spinal contrast-enhanced MRA (CE-MRA) and selective spinal DSA. Localization and spatial configuration of the artery of Adamkiewicz by CE-MRA agreed with DSA findings in 14 of 15 cases. Comparison of image quality revealed that DSA was superior to CE-MRA concerning vessel continuity, sharpness, and background homogeneity (p < .001). Overall vessel conspicuity and contrast were judged to be similar.
Advances in both MR and CT promise to provide increasingly reliable information on both normal spinal vascular anatomy and spinal vascular pathology. Information from noninvasive imaging is often extremely helpful in planning evaluation and treatment of disorders involving the spinal vasculature. Nevertheless, spinal angiography remains indicated when specific information regarding the vascular supply of the spine, cord, or adjacent tissue is required. Evaluation and endovascular treatment of spinal vascular malformations and some vascular neoplasms are the major indications for spinal angiographic examination. In most cases, MRI findings suggestive or diagnostic of a spinal vascular malformation mandate further evaluation with spinal angiography, particularly for planning surgical or endovascular therapy. In contrast, the role of angiography is limited in the evaluation of infarction or ischemia involving the spine, except in cases of aortic occlusion.
Classification of Spine and Spinal Cord Vascular Lesions
Vascular malformations of the spine and spinal cord comprise a heterogeneous group of abnormalities, which are reported to make up approximately 3% to 16% of spinal mass lesions. The classification or delineation of distinct, relatively homogeneous subgroups of spinal vascular malformations is important to permit useful characterization of the lesions with regard to clinical behavior and therapeutic options. The widespread use of selective angiographic examination and MRI has resulted in improved definition of the angioarchitecture and hemodynamics of spinal vascular lesions, features implicit in useful classification. Additional aspects of spinal vascular lesions important for classification include specific imaging features; anatomic localization with regard to the dura and the spinal cord; the type of shunt-involved fistula or nidus; and potential relationships with genetics, vascular biologic features, and angiogenesis (13).
Various classification systems and eponyms for spinal vascular lesions have been used over the years with resultant confusion and difficulty in comparing and evaluating the various types and subgroups (13,14,15,16). Anson and Spetzler (14) proposed a widely used, relatively simple classification that distinguishes four types of spinal vascular malformations associated with arteriovenous shunting: type I, spinal dural arteriovenous fistulas (SDAVFs); type II, intramedullary glomus AVMs; type III, juvenile or combined AVMs; and type IV, intradural perimedullary AVFs.
Spetzler et al. (17), in a recently proposed modification of this classification system, divided spinal vascular lesions into three primary or broad categories: neoplasms, aneurysms, and arteriovenous lesions. Arteriovenous lesions are further subdivided based on their angioarchitecture into AVFs and AVMs.
TABLE 23.1 Spinal Vascular Malformations | ||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Under the modified classification, AVFs are subdivided into extradural and intradural lesions, with the latter being classified as either “dorsal” or “ventral.” Intradural AVFs occur far more frequently, with the “dorsal” type representing the most common spinal vascular lesion, the (SDAVFs) (type 1). The “ventral” type of intradural AVF, previously referred to as spinal cord AVF or perimedullary AVF (type IV), occurs much less frequently.
Spinal AVMs, characterized by the presence of a nidus as the site of arteriovenous shunting, are divided into extradural–intradural and intradural. Extradural–intradural AVMs, also referred to as “juvenile” arteriovenous confirmations (type III), are uncommon lesions. Intradural AVMs, previously referred to as “glomus” type (type II), have been newly subdivided into intramedullary and intramedullary–extramedullary based on their relationship to the spinal cord. In addition, conus medullaris AVMs comprise a newly proposed category. Table 23.1 relates the terminology of these two most widely utilized classification systems to the various spinal vascular lesions.
A number of features of this modified classification system remain controversial, including its classification of cavernous malformations (CMs) as neoplasms (18). Nevertheless, familiarity with these two most widely used classifications is useful for understanding, evaluating, and communicating information regarding this important group of spinal vascular lesions.
With regard to the spinal dura, which represents a topographical landmark for localization of spinal vascular malformations, these lesions can be classified as follows:
Spinal extradural AVMs
Paraspinal arteriovenous shunts.
These are very rare lesions characterized by a direct fistulous connection between a segmental artery or a branch of it and the corresponding segment of the paraspinal venous system at this level. They may occur at any level along the spinal notochord but the majority occurs at the thoracic level. They may drain through a radicular vein into the perimedullary venous system causing significant venous ectasias with cord compression and venous congestion of the spinal cord. In addition, arterial steal phenomenon may occur in cases with a high-volume arteriovenous shunt.
Spinal epidural arteriovenous shunts
These are also extremely rare and small lesions located within the spinal epidural space and draining into epidural veins. They may cause intradural venous congestion or present with an acute epidural hematoma.
SDAVMs or shunts
These are the most common spinal vascular malformation with arteriovenous shunting. They are acquired lesions located within the dura, most commonly within the dural sleeve of a nerve root in the intervertebral foramen, are fed by a radiculomeningeal artery and drain through a radicular vein in a retrograde direction into the perimedullary venous system. Intramedullary venous congestion with progressive myelopathy is the pathophysiologic and clinical hallmarks of the disease.
Spinal intradural AVMs
Spinal intradural AVMs may be located in the subarachnoid space surrounding the spinal cord, along the intradural course of a nerve root, in the spinal cord itself with or without extramedullary extension, or in the filum terminale. Topologically, intradural AVMs are, therefore, classified into four types:
Perimedullary AVFs
Intramedullary AVMs
Radicular AVMs
Filum terminale AVFs
In addition, spinal intradural AVMs may have or lack a genetic association. Depending on the hereditary or nonhereditary type of genetic association, or the absence of a genetic link, spinal intradural AVMs are classified into three types:
Single arteriovenous shunts associated with a genetic hereditary disorder.
The great majority of these patients have hereditary hemorrhagic telangiectasia type I (HHTI) or Rendue–Osler–Weber disease. The arteriovenous shunt is typically a perimedullary arteriovenous macrofistula.
TABLE 23.2 Spinal Vascular Malformations
Terminology
Typical location
Vascular supply
Presentation and course
Clinical associations
Treatment
SDAVF, type I, dorsal intradural AVF
Lumbar, thoracic
Dural arteries
Chronic myelopathy
None
1. Embolization
2. Surgery
SCAVM, type II, intradural AVM
Cervical, thoracic, lumbar
Spinal arteries (ASA, PSA)
Acute, hemorrhage common
Paraspinal involvement—rare
1. Embolization
2. Surgery
SCAVF, type IV, ventral intradural AVF
Lumbar, thoracic
Spinal arteries (ASA > PSA)
Acute or chronic may hemorrhage
None
1. Embolization
2. Surgery
CM
Cervical, thoracic, lumbar
Minimal
Acute or chronic may hemorrhage
Intracranial or familial CM
Surgery
ASA, anterior spinal artery; AVF, arteriovenous fistula; AVM, arteriovenous malformation; CM, cavernous malformation; PSA, posterior spinal artery; SDAVF, spinal dural arteriovenous fistula; SCAVM, spinal cord arteriovenous malformation.
Multiple genetic, nonhereditary arteriovenous shunts
with a metameric distribution affecting the cord, the dura, the vertebral body, the paraspinal musculature and the skin.
A typical representative of this group is the Cobb syndrome.
without an evident metameric link.
In the majority of these patients, the intradural arteriovenous shunt is co-existent with a vascular malformation of a limb corresponding to the Klippel–Trenauney or Parks–Weber syndrome.
Single, sporadic spinal intradural AVMs.
This is the most common type of a spinal intradural arteriovenous shunt. It may affect the cord, a nerve root, or the filum terminale. Angiomorphologically, the shunt is either of the plexiform (nidus) type or a small AVF.
Spinal cord CMs
This chapter will emphasize imaging evaluation of major groups of nonneoplastic spinal vascular lesions including:
the major angiomorphologic types of spinal arteriovenous shunts, that is, the spinal dural arteriovenous shunts, the plexiform (nidus) type spinal cord AVMs, and the perimedullary AVFs;
the spinal cord CMs;
spinal cord ischemia and infarction; and
spinal hemorrhage (Tables 23.1 and 23.2).
It has to be noted that neither developmental venous anomalies (DVAs) nor capillary telangiectasias occur in the spinal cord and will therefore not be discussed here.
Spinal Dural Arteriovenous Fistula
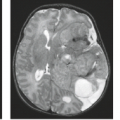
SDAVFs, also known as type I or dorsal intradural AVFs, are the most common spinal vascular malformation, with some estimates ranging as high as 80% of the total (23,24). The use of MRI has resulted in more frequent diagnosis of these lesions, which are often undetectable by other noninvasive imaging modalities.
In contrast to spinal cord AVMs, SDAVFs are believed to be acquired lesions, possibly resulting from thrombosis of the extradural venous plexus. Evidence for their acquired nature includes their virtual absence in young patients and predominance in later life; the lack of association of SDAVF with other vascular anomalies; and their predilection for a location below the midthoracic spine, where increased venous pressure exists in a standing position (25,26).
Anatomy and Pathophysiology
SDAVFs are arteriovenous (AV) shunts that occur within the dural covering of the spinal cord (Fig. 23.9). Usually adjacent to the intervertebral foramen or within the dural root sleeve, the shunts are most often tiny, usually receiving arterial supply from a dural branch of a single radicular artery. This most common type, with a single feeding artery, has been designated type A, and the much less common type, which receives multiple feeding arteries, has been termed type B in the modified classification. An intradural vein drains directly into the pial veins of the cord, most prominently over the dorsal aspect (27). The result is venous engorgement and venous hypertension involving the spinal cord. SDAVFs may occur at any level of the spinal cord, from the foramen magnum to the sacrum, but most commonly occur at thoracolumbar levels, usually between T5 and L3. Most often, no direct arterial supply to the spinal cord itself originates from the radicular artery feeding an SDAVF. In 10% to 15% of cases, however, the SDAVF is fed by a radicular
artery that also supplies the spinal cord via a radiculomedullary or radiculopial branch (28,29).
artery that also supplies the spinal cord via a radiculomedullary or radiculopial branch (28,29).
Venous drainage from the SDAVF results in increased pressure and engorgement of the pial veins of the spinal cord. The increased venous pressure is transmitted to the intrinsic veins of the cord, reducing the intramedullary AV pressure gradient. A decrease in tissue perfusion results in hypoxia of the cord. Intramedullary vasodilation and loss of autoregulatory capacity may also occur resulting in cord edema, stagnation of blood flow, and disruption of the blood–CNS barrier (30). The longitudinal extent of cord dysfunction from the venous hypertension may be very extensive and may progress over time. Poor correlation between the location of the AV shunt and the clinical level of spinal dysfunction is a frequent finding. The chronic effects of this longstanding venous hypertensive myelopathy results in a “subacute necrotizing myelopathy” which is clinically identical to the syndrome described by Foix and Alajouanine in 1926 (31). SDAVF is, therefore, the underlying pathology in the disorder referred to as Foix–Alajouanine syndrome (23,32).
The elevated pressures in spinal pial veins draining SDAVFs vary in association with arterial pressure elevations, possibly accounting for the clinical worsening reported with exercise (33). The venous hypertensive myelopathy induced by SDAVFs is reversible if treated early but may become irreversible in later stages.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree