Internal jugular veins (green)
Sinus transversus
Facial vein
Pharyngeal vein
Vein of pterygoid canal
Lingual vein
Superior thyroid vein
Inferior thyroid vein
External jugular veins (red)
Posterior auricular vein
Retromandibular vein
Anterior jugular veins (blue)
Cutaneous vessels
Anonymous veins (yellow)
Inferior thyroid vein
Thyroid ima vein
Vertebral vein
Subclavian veins (pink)
Direct continuation of the axillary vein, forming the anonymous vein with the external jugular vein
External jugular vein
Superficial cervical vein S
uprascapular vein
Transverse cervical vein
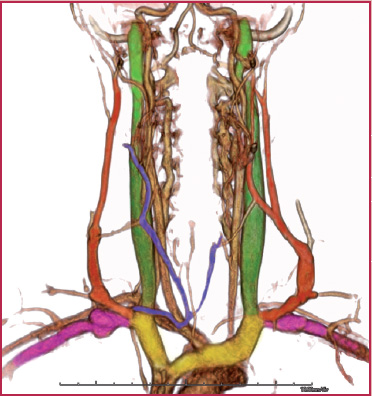
Fig. 17.1
17.1
Table 17.2
Venous anatomy of the upper limbs
Cephalic vein (red) | Dorsal venous network of the hand Digital veins of hand Intercapital veins |
Basilic vein (yellow) | Dorsal venous network of the hand |
Median basilic vein (orange) | Variable |
Median vein (blue) | Variable |
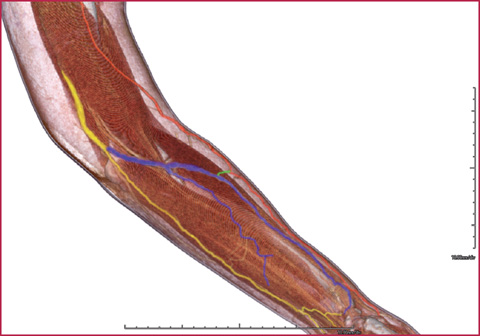
Fig. 17.2
Direct CT venography of the forearm in a patient with previous thrombotic events: the study demonstrated the patency of the venous system of the arm and forearm
The cephalic vein originates from the radial side of the forearm, crosses the elbow anteriorly and runs up along the anterolateral surface of the biceps and brachioradialis muscle; after passing between the pectoralis major muscles and through the deltopectoral triangle, it ends at the axillary vein.
The basilic vein originates on the ulnar side of the forearm, runs up on the posteromedial side of the forearm and, after crossing anteriorly the elbow, travels between the muscles around the pronator and biceps, crossing the brachial artery. It ends at the axillary vein at the inferior edge of the teres major muscle.
Veins of the Lower Limbs
Knowledge of the venous system of the lower limbs and the exact difference between the vessels of the superficial and deep districts is not only crucial for anatomical and functional analysis, but, more importantly, can have direct clinical implications for diagnosis: for example, venous thrombosis principally occurs in the vessels of the deep system (deep venous thrombosis, DVT), being a possible cause of distant embolism.
On the other hand, the superficial system is more frequently affected by other pathological conditions, such as varicosis and phlebitis; thrombosis of the superficial vessels is rare, and with less relevant possible consequences.
The deep and superficial veins are largely interconnected. The blood drained by the superficial veins flows into the deep system through the perforating veins, reaching the inferior vena cava and the heart. The veins of the deep system are accompanied by the homonymous arteries. The two main vessels of the superficial system are the great saphenous vein (GSV) and the small saphenous vein (SSV).
The SSV originates from the lateral side of the foot and runs up on the posterolateral edge of the achilles tendon; after reaching the popliteal fossa, between the two heads of the gastrocnemius muscle, it ends at the popliteal vein (Table 17.3, Fig. 17.3).
The GSV (Table 17.3, Figs. 17.4–17.5) originates from the medial side of the foot, travels anteriorly to the medial malleolus and runs up the medial side of the knee; in the thigh it keeps running in an anteromedial position, passes through the foramen ovale and ends at the common femoral vein (saphenofemoral junction).
Signs of the Embryological Development of the Venous System
The cardinal veins are the main vessels for the venous drainage of the embryo. The anterior and posterior cardinal veins run on the ventral and dorsal sides of the common cardinal veins, and empty into them before ending in the sinus venosus.
In the eighth week an oblique anastomosis connects the anterior cardinal veins; this anastomotic vessel will form the left brachiocephalic vein after the complete degeneration of the distal part of the anterior cardinal vein.
The superior vena cava (SVC) originates from the right anterior cardinal vein and the right common cardinal vein.
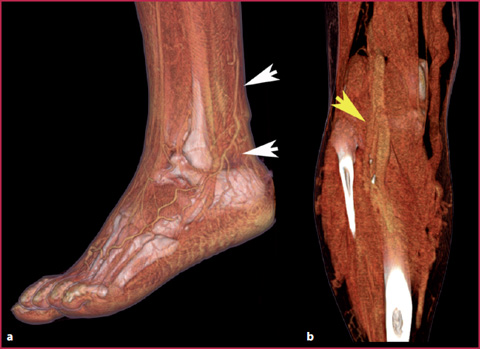
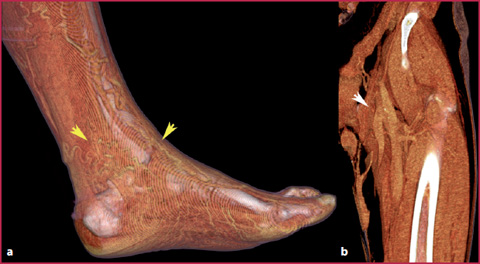
Table 17.3
Venous anatomy of the lower Limbs
Great saphenous vein | Dorsal venous network of the foot (medial side) Dorsal venous arch of the foot Superficial epigastric vein Superficial circumflex iliac vein Scrotal veins (or anterior labial veins) |
Small saphenous vein | Veins of the knee Plantar digital veins |
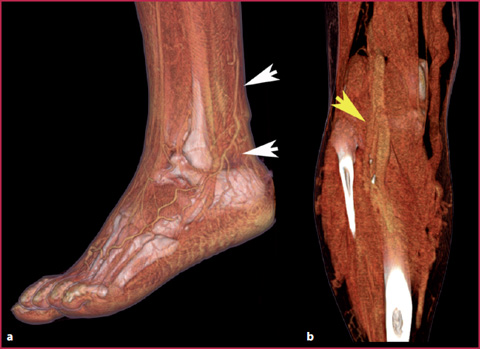
Fig. 17.3
CT venography showing the origin and termination in the popliteal cavity of the SSV. a the SSV originating posteriorly to the lateral malleolus from multiple small venous vessels of the superficial network of the foot (white arrow heads). b Sapheno-popliteal junction (yellow arrow head), where the SSV ends into the popliteal vein
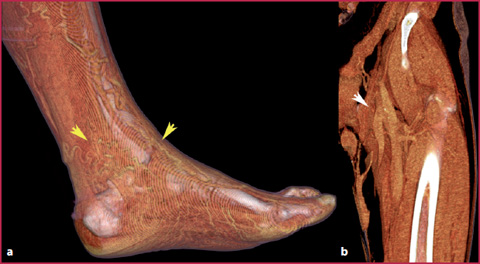
Fig. 17.4
CT venography showing the origin and termination in the femoral vein of GSV. a the GSV originating from small venous vessels of the dorsal and ventral regions of the foot (arrow heads). b termination of the GSV at the sapheno-femoral junction after its complete path along the lower limb (arrow head)
The posterior cardinal veins almost completely degenerate during development; their only residuals are the origin of the azygos vein and the common iliac veins.
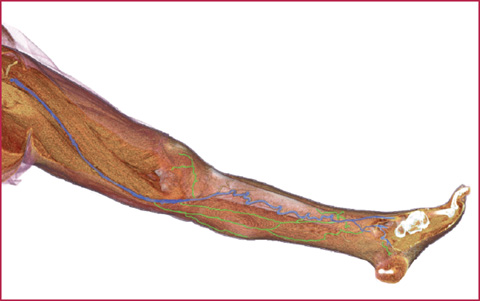
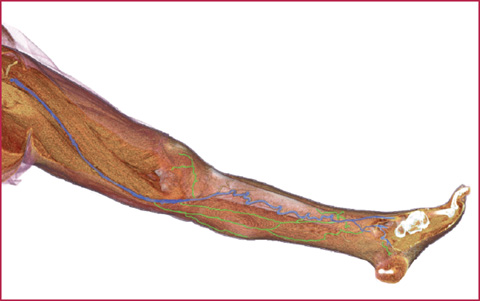
Fig. 17.5
CT venography for the evaluation of the GSV system in a patient with venous insufficiency and previous DVT. The study enables visualization of the entire GSV (blue) from the dorsal region of the medial side of the foot to the sapheno-femoral junction. In the calf, the vessels are tortuous and slightly dilated. In green, multiple collateral vessels, variable from patient to patient
The posterior cardinal veins are gradually substituted by the subcardinal and supracardinal veins. The subcardinal veins, the first to appear, are interconnected by the subcardinal anastomosis; the mesophrenic sinusoids connect the subcardinal veins with the posterior cardinal veins; the subcardinal veins form the peduncle of the left renal vein, the suprarenal veins, gonadic veins (ovaries and testicles) and a part of the inferior vena cava (IVC).
The supracardinal veins appear later, ending in the region of the kidneys; in their upper part they are connected by an anastomosis which will form the azygos and hemiazygos veins.
Below the kidneys, the left supracardinal vein disappears, while the right supracardinal vein will form a part of the inferior vena cava.
The SVC is formed by the right anterior cardinal vein and the right common cardinal vein.
Development of the Inferior Vena Cava
The IVC is formed by four main embryonic segments:
A hepatic segment derived from the hepato-cardiac channel;
A suprarenal segment derived from the right subcardinal vein;
A renal segment derived from the subcardinal and supracardinal anastomosis;
A subrenal segment derived from the right supracardinal vein.
17.2 17.2 Main Congenital Anomalies
The complexity of venous system development leads to the possible presence of multiple anomalous variants in its definitive structure, which are not frequently observed. In most cases these anomalies are asymptomatic and have no clinical significance; nevertheless, it is necessary to be aware of all the main anatomic venous anomalies to be able to recognize them in imaging studies performed for other purpose (above all in patients evaluated for thoracic and abdominal surgery), in complex malformative syndromes, or when an anomalous venous vessel is the cause of the clinical symptomatology due to its interactions with surrounding normal structures (syndrome of the pyeloureteral junction, Fig. 17.6).
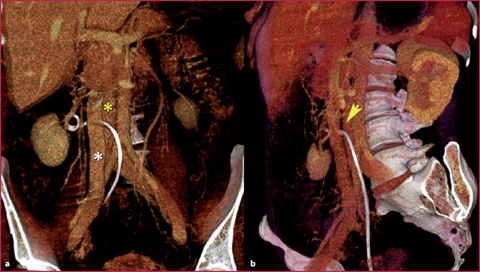
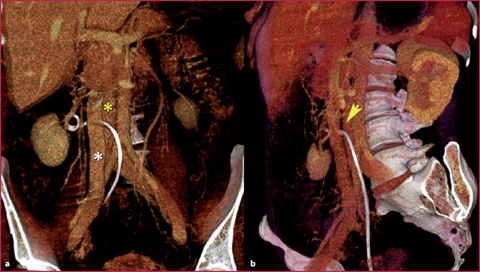
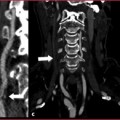
Fig. 17.6
CT venography in a patient with double IVC causing compression of the pyeloureteral junction, treated by ureteral stent positioning. a The two vessels form a double IVC in the sub-hepatic tract (asterisks). b Ureteral compression between the two vessels (arrow head)
Superior Vena Cava
The most frequent anomaly is persistence of the left SVC. This abnormality, which leads to the presence of a double SVC, derives from the persistence of the left anterior cardinal vein. The anastomosis that usually forms the left brachio-cephalic vein is small or absent (Fig. 17.7). A unique left SVC occurs when the persistence of the left SVC is associated with the degeneration of the right common and anterior cardinal veins (normally forming the right SVC).
The evaluation of the anomalies of the vessels forming the superior caval district is crucial in patients awaiting the placement of endovascular devices with subclavian or jugular access, such as a central venous catheter or port-a-cath.
Inferior Vena Cava
The inferior vena cava can show several anomalies in its abdominal tract, which can sometimes be interrupted at different levels; in such cases, the blood coming up from the lower limbs, abdomen and pelvis is drained by the azygos system through collateral circles. The clinical symptoms essentially depend on the obstructed and delayed blood flow on its way to the heart; this can lead, in prone patients, to the occurrence of DVT in the iliac veins and the deep veins of the lower limbs.




Azygos continuation of the IVC (absence of the hepatic segment of the IVC): this anomaly derives from the failure to form the right subcardinal-hepatic anastomosis, with resulting atrophy of the right subcardinal vein. As a consequence, the blood drained from the lower limbs is shunted to the azygos system; the hepatic veins end independently in the right atrium. It can be associated with severe congenital heart disease and asplenia or polysplenia syndromes.
Double IVC: this anomaly originates from persistence of the lower tract of the left supracardinal vein and results in the presence of two venous vessels constituting the inferior caval system inferiorly to the renal veins; the left vessel is generally smaller.
Left IVC: A left IVC results from regression of the right supracardinal vein with persistence of the left supracardinal vein. Typically, the left IVC joins the left renal vein uniting with the right renal vein to form a normal right-sided IVC in its above renal path.
Absence of the entire posthepatic IVC: this condition suggests that all three paired venous systems failed to develop properly and leads to the constitution of multiple collateral circles in the lumbar, sacral and inferior epigastric systems (Figures 17.8-17.9).
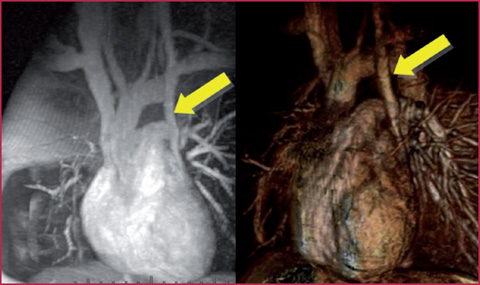
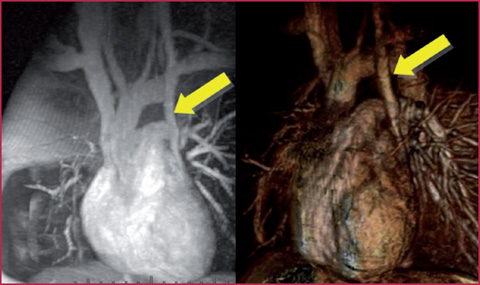
Fig. 17.7
Contrast-enhanced MR venography with Maximum Intensity Projection (MIP) and Volume Rendering (VR) reformations, showing a double SVC with a posterior outlet in the coronary sinus (arrows)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree