15 Vertebral Collapse—Benign or Malignant
Introduction
Vertebral collapse is a serious condition, which is closely related to age.1,2 According to the demographic changes of our society the incidence and prevalence of vertebral compression fractures are increasing. Vertebral compression fractures are associated with increased morbidity and mortality and thus, vertebral collapse has a significant impact on the patient’s overall quality of life and on the patient’s life expectancy.3,4 The causes of vertebral collapse are manifold, including benign and malignant conditions.5–7 Most vertebral compression fractures are of benign origin caused by inadequate trauma in patients with osteoporosis or osteomalacia.8 The International Osteoporosis Foundation estimated that at the age of 65 years 1% of women and 0.5% of men will sustain an acute vertebral compression fracture and the presence of an osteoporotic vertebral compression fracture increases the odds of subsequent fractures five fold.9 Early diagnosis followed by appropriate therapy reduces the occurrences of subsequent fractures and other sequelae.10
Less frequently seen are vertebral compression fractures following metastatic, hematologic or neoplastic disease.1,4 The spine represents the most frequent site of skeletal metastasis predominating in the thoracic and lumbar spine.11 It is essential to differentiate benign from malignant vertebral collapse because their medical management and their outcome are substantially different.1,4,12
In general, the differentiation of pathological from benign vertebral compression fractures is based on distinct imaging findings such as replacement of fatty bone marrow, contrast enhancement, soft tissue compartments, and the shape and site of fracture.1, 11 However, separating benign from malignant vertebral compression fractures can be problematic in the acute setting, because within the first 8 to 12 weeks after the vertebral collapse the clinical presentation and radiological appearance are similar in both conditions. The problem in the differentiation arises from edema, hemorrhage, and the presence of repair tissue that accompanies acute benign fractures, which results in bone marrow changes which resemble metastatic disease.13,14 Thus, the differentiation between benign or pathological vertebral compression fractures remains a challenge for the clinician and the radiologist involved.14–16
Although clinical evaluation, laboratory data, and imaging findings may be suggestive of either benign or pathological vertebral collapse, there are currently no absolute criteria available for definite diagnosis of one or the other type of fracture.17,19 There is general agreement that definite diagnosis can only be established by obtaining a tissue specimen. This, however, requires a biopsy or another invasive procedure, which is inappropriate or even counterproductive in patients with multiple or subsequent vertebral compression fractures.14,20–22 Thus, in these patients differentiation between benign or pathological vertebral compression fractures has to be based on imaging features, clinical presentation, and laboratory data.
In the following paragraphs the most important clinical findings and radiologic features for the differentiation of benign versus pathological vertebral collapse will be discussed.
Clinical Evaluation
Age
The patient’s age is ambiguous for such differentiation, as most of the vertebral collapses occur in elderly people because the prevalence of both osteoporosis and metastatic disease increases with age.23 In patients with known metastatic disease, up to 25% of vertebral compression fractures are of osteoporotic origin. On the other hand, in patients with moderate to severe osteoporosis up to 10% of vertebral collapses are of pathological origin.11 It is also well known that a pathological vertebral compression fracture is frequently the first presentation of an otherwise occult primary tumor, thus the lack of a known neoplasm does not necessarily exclude a pathological vertebral compression fracture. Furthermore, patients with known metastatic disease in other locations than the spine may also suffer from benign vertebral collapse, following adjuvant therapy for the primary tumor.7,10,24 Most of these adjuvant therapy concepts use chemotherapeutic agents and/or radiation, with either localized or generalized effects on bone metabolism.3–5
History of Trauma
In most patients with benign vertebral collapse a trauma history can be obtained. However, if such patients report inadequate trauma strength or if the fracture location does not match with the trauma mechanism the suspicion of a pathological compression fracture has to be raised.
| Benign | Malignancy | |
| Involvement of dorsal elements | 1 | 4 |
| Bulging/destruction of dorsal wall | 1 | 4 |
| Involvement of posterior half of vert. body | 2 | 3 |
| Soft tissue mass | 2 | 3 |
| Edema (diffuse) | 2 | 3 |
| Contrast enhancement | 2 | 3 |
| Single segment | 3 | 3 |
| Dislocation of intact dorsal wall | 3 | 2 |
| Edema (focal) | 3 | 2 |
| Multi-segmental | 3 | 2 |
| Involvement of anterior half of vert. body | 3 | 2 |
| Fatty bone marrow (remnants) | 4 | 1 |
| Fluid sign (if present) | 5 | 0 |
Likelihood to be found in either benign or malignant vertebral compression fractures: 0 (not likely at all) to 5 (almost pathognomonic)
Other clinical features, such as pain, restricted mobility of the spine, neurological deficits or fatigue are common in patients with both benign and pathological vertebral compression fractures, and may therefore not be used for differentiation. Thus, clinical presentation may provide clues but not criteria for the differentiation of benign versus pathological vertebral collapse.
Imaging Findings
In general, recognition of vertebral collapse presents no difficulties to the radiologist (Table 15.1). Most vertebral collapses are diagnosed on conventional radiographs, which are considered an adequate screening technique. The detection and diagnosis of vertebral collapse has improved significantly with the use of cross-sectional imaging, such as magnetic resonance imaging (MRI) or computed tomography (CT), mainly because of their multi-planar reconstruction (MPR) capabilities.25,26 However, the differentiation between benign and pathological vertebral compression fractures remains a challenge to the radiologist because of their ambiguous appearance.16,27–30 Thus, the radiologist and the clinician involved have to keep in mind that the accuracy of almost all imaging findings listed below is low because they can be found in both pathological and benign fractures or they occur infrequently (see Tab. 15.2).23,31
Fatty Bone Marrow
The best imaging clue for distinguishing benign from pathological fractures is the presence of fatty (yellow) bone marrow.11 After adolescence, yellow bone marrow replaces the preexisting hematopoietic (red) bone marrow (Fig. 15.1). Yellow bone marrow has a distinctive (i. e., fatty) appearance on MRI presenting with hyperintense signals on T1W and T2W sequences and loss of signal on STIR and fat-saturated sequences.32–34 On the other hand in metastatic disease tumor tissue, which in general lacks any fatty compartments, supersedes fatty bone marrow. Hence, the MRI appearance of osseous metastases presents with low-signal intensities on T1W images and high-signal intensities on STIR and T2W images.
Thus, yellow bone marrow and tumor tissue produce a distinctive natural contrast on T1W images, which can be easily depicted on MRI. It is safe to say that if fatty bone marrow is present in a vertebral collapse, vertebral metastasis can be excluded.19,35
Edema
Unfortunately, the reverse does not apply, because acute vertebral collapse presents with pronounced edema regardless of the underlying cause. Features favoring benign vertebral collapse include preservation of fatty bone marrow within the collapsed vertebral body and a typical, horizontal band-like pattern of the edema.30 Signs suggesting pathological vertebral compression fractures include diffuse replacement of fatty bone marrow by edema typically throughout the entire vertebral body including the posterior elements.36,37
These two distinctive patterns are useful guidelines for differentiating benign from pathological vertebral compression fractures, however, they are infrequently present and they lack specificity.23
Shape—Extent of Fracture
Vertebral collapse can be of minimal extent (circumscribed vertebral endplate fracture), of moderate extent (loss of height less than 25%), or severe (up to 75% of height) or subtotal. However, the extent of fracture does not correlate with its cause.
Several different shapes of vertebral compression fractures are known, such as: (1) “wedge-shaped vertebrae” related to collapse of the anterior aspect of the vertebral body (Fig. 15.2); (2) “fish-bone vertebrae,” which are characterized by intact anterior and posterior walls, and bi-concave deformities of the upper and lower vertebral endplate (Fig. 15.3); (3) “pancake vertebrae,” which are flat-shaped remnants of vertebral bodies after subtotal vertebral compression fractures; and (4) “burst fractures,” which are complex-shaped vertebral collapses with irregular margins and multiple fragments.11 The first three types of fractures are frequently associated with benign collapses, and the latter two with pathological fractures.
Convex deformation of the posterior wall is frequently seen in metastatic disease and may serve as an indicator for pathological vertebral compression fractures (Fig. 15.4). However, in patients with extensive vertebral collapse displacement of the posterior wall may resemble such pathological deformation.
Although shape is a good indicator for distinguishing between benign and pathological collapse, this feature lacks specificity and is infrequently suitable for differentiation.

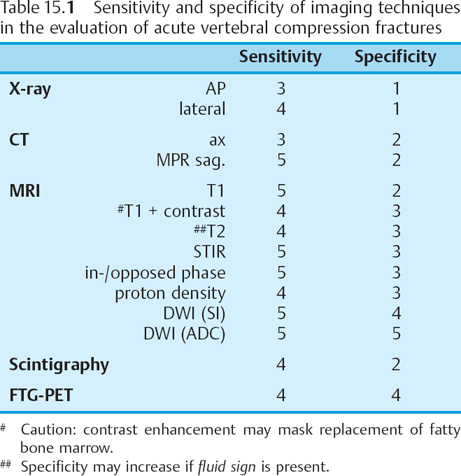
Fig. 15.1 Pathological vertebral compression fracture. A T1W image (a) before and (b) after (fat suppression) i. v. application of contrast material. c A T1W image in the axial plane. Convex deformation (bulging) of the posterior vertebral wall and involvement of the posterior vertebral elements as well as the marked enhancement after i. v. administration of gadolinium are almost pathognomonic for metastatic disease. The involvement of the dorsal vertebral structures is best delineated on the axial images.
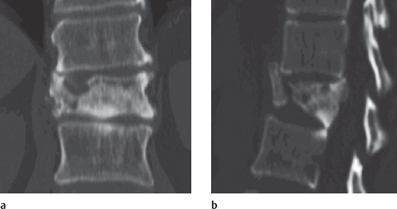
Fig. 15.2 Benign vertebral compression fracture of L1. The images show a multi-planar reconstruction in the coronal (c) and sagittal (b) planes. The patient was reported to have fallen from a ladder (adequate trauma). A wedgeshaped vertebral compression fracture is shown with a dislocated anterior vertebral wall and an intact posterior vertebral wall, which is a typical finding in posttraumatic vertebral compression fractures. Note the sclerotic appearance of the fractured vertebra following impaction. There is no soft tissue mass, edema, or hemorrhage present indicating an old vertebral compression fracture.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree