Tumor category
Major changes
Adipocytic
Mixed-type liposarcoma removed
Fibroblastic
DFSP and giant cell fibroblastoma included for the first time
Myofibroblastic
“Hemangiopericytoma” removed as a synonym for SFT
Recognition of nodular fasciitis and variants as true neoplasms
So-called fibrohistiocytic
“Malignant fibrous histiocytoma” removed
Smooth muscle
Angioleiomyoma reclassified as pericytic tumor
Pericytic
Angioleiomyoma reclassified as a pericytic tumor
Myofibroma now classified as pericytic tumor
Skeletal muscle
Spindle cell/sclerosing rhabdomyosarcoma classified together and separated from others subtypes
Vascular
Pseudomyogenic (epithelioid sarcoma-like)
Hemangioendothelioma added as a new entity
Gastrointestinal stromal
GIST included in the volume on STT for the first time
Nerve sheath
Peripheral nerve sheath tumors included volume on STT for the first time
New hybrid benign nerve sheath tumors included (schwannoma/perineurioma)
Tumors of uncertain differentiation
New tumors: acral fibromyxoma, hemosiderotic fibrolipomatous tumor differentiation
Phosphaturic mesenchymal tumor
Atypical fibroxanthoma now included
PNET removed as synonym for Ewing’s sarcoma
Undifferentiated/other category
Includes tumors that cannot be classified into any unclassified sarcoma
11.2 Adipocytic Tumors
Due to the high incidence of lipomas, angiolipomas, and liposarcomas, adipocytic tumors represent the largest single group of mesenchymal tumors. The WHO classification persists to consider atypical lipoma (atypical lipomatous tumor) and well-differentiated liposarcoma as essentially synonymous (Table 11.2) and considered locally aggressive with no potential for metastasis [1]. The terms “mixed-type liposarcoma” and myxolipoma have been deleted.
Table 11.2
Group 1 – Adipocytic tumors
Benign |
Lipoma |
Lipomatosis |
Lipomatosis of the nerve |
Lipoblastoma |
Angiolipoma |
Myolipoma of the soft tissue |
Chondroid lipoma |
Spindle cell lipoma/pleomorphic lipoma |
Hibernoma |
Intermediate (locally aggressive) |
Atypical lipomatous tumor/well-differentiated liposarcoma |
Malignant |
Dedifferentiated liposarcoma |
Myxoid liposarcoma |
Pleomorphic liposarcoma |
Liposarcoma, not otherwise specified |
In children diffuse lipoblastoma is now the preferred term for lipoblastomatosis.
The definition of dedifferentiated liposarcoma has been slightly modified and is currently subdivided into four groups (see Table 11.1). Chondroid lipoma may resemble myxoid liposarcoma. Unlike myxoid liposarcoma chondroid lipoma usually shows calcifications, which are best demonstrated by radiographs, CT, or US [3].
11.3 Fibroblastic/Myofibroblastic Tumors
Fibroblastic/myofibroblastic tumors represent a very large group of mesenchymal tumors, many of which contain fibroblastic as well as myofibroblastic elements (Table 11.3). The current WHO classification recognizes that nodular fasciitis, proliferative fasciitis, and proliferative myositis (Fig. 11.1) are neoplastic [4], whereas previously they were believed to be reactive lesions.

Table 11.3
Group 2 – Fibroblastic/myofibroblastic tumors
Benign |
Nodular fasciitis (proliferative fasciitis/proliferative myositis) |
Myositis ossificans |
Elastofibroma |
Fibromatosis colli |
Fibrous hamartoma of infancy |
Juvenile hyaline fibromatosis |
Inclusion body fibromatosis |
Fibroma of the tendon sheath |
Desmoplastic fibroblastoma |
Mammary-type myofibroblastoma |
Calcifying fibrous tumor |
Angiofibroma |
Angiomyofibroblastoma |
Gardner fibroma |
Calcifying fibrous tumor |
Intermediate (locally aggressive) |
Superficial fibromatosis (plantar/palmar) |
Desmoid-type fibromatosis |
Lipofibromatosis |
Giant cell fibroblastoma |
Intermediate (rarely metastasizing) |
Dermatofibrosarcoma protuberans |
Solitary fibrous tumor |
Inflammatory myofibroblastic tumor |
Myofibroblastic sarcoma/atypical myxoinflammatory fibroblastic tumor |
Infantile fibrosarcoma |
Malignant |
Adult fibrosarcoma |
Myxofibrosarcoma |
Low-grade fibromyxoid sarcoma |
Sclerosing epithelioid fibrosarcoma |

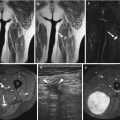
Fig. 11.1
Proliferative myositis of the thigh. Axial T2-WI image shows a well-defined mass (arrow) within the adductor muscle with inhomogeneous mild high signal intensity with areas of low signal within the lesion due to the fibrous content
Other changes were the inclusion of the closely related giant cell fibroblastoma and dermatofibrosarcoma protuberans (DFSP), formerly included in volume on skin lesions. DFSP is categorized as a rarely metastasizing (intermediate) tumor, although it should be noted that metastatic potential is gained only when a component of a fibrosarcomatous change is present [5]. Giant cell fibroblastoma is classified in the locally aggressive (intermediate) category because it recurs in approximately 50 % of cases, but does not metastasize [6]. Hemangiopericytoma has been removed from the classification of “extrapleural solitary fibrous tumor” because it is well established that this outdated term included tumors that represented cellular examples of SFT [5]. Lipomatous hemangiopericytoma and giant cell angiofibroma have also been included as SFT. The term “atypical myxoinflammatory fibroblastic tumor” was introduced for as synonym for “myxoinflammatory fibroblastic sarcoma.” This new term better reflects the extremely low potential for metastasis for this tumor type.
11.4 So-Called Fibrohistiocytic Tumors
As the concept of fibrohistiocytic differentiation has been a matter of debate [7], malignant fibrous histiocytoma (MFH) has been finally deleted from the current WHO classification. MFH and its subtypes have been reclassified in the new separate group of unclassified/undifferentiated sarcomas (group 12). Thus, group 3 now does not include malignant tumors (Table 11.4). It includes the common tenosynovial giant cell tumors, the uncommon giant cell tumor (Fig. 11.2) of soft tissues, and the plexiform fibrohistiocytic tumor.

Table 11.4
Group 3 – The so-called fibrohistiocytic tumors
Benign |
Tenosynovial giant cell tumor |
Localized type |
Diffuse type |
Malignant |
Deep benign fibrous histiocytoma |
Intermediate (rarely metastasizing) |
Plexiform fibrohistiocytic tumor |
Giant cell tumor of the soft tissue |

Fig. 11.2
Giant cell tumor of the soft tissue with Paget’s disease. Axial T2-WI image shows an intermediate signal nodular lesion in the pretibial subcutaneous space (thin arrow). Note the cortical thickening due to Paget’s disease (thick arrow)
11.5 Smooth Muscle Tumors
Smooth muscle tumors arising at non-cutaneous, non-uterine locations have been the focus of a considerable conceptual shift in the past but there were no major changes in this category (Table 11.5). The only change is that angioleiomyoma (vascular leiomyoma) was reallocated to the category of pericytic (perivascular) tumors (group 5). There are no changes on the deep leiomyosarcoma, although some tumors classified as undifferentiated pleomorphic sarcoma closely resemble a subset of leiomyosarcoma, which may suggest the existence of “dedifferentiated leiomyosarcoma.”
Table 11.5
Group 4 – Smooth muscle tumors
Benign |
Leiomyoma of the deep soft tissue |
Malignant |
Leiomyosarcoma (excluding the skin) |
11.6 Pericytic (Perivascular) Tumors
The lesions in the pericytic/perivascular category were first included in the 2002 edition. At the same time, hemangiopericytoma was removed from this group and listed as synonym for solitary fibrous tumor (group 2). Although rare, the most common tumor analyzed on imaging in this group is glomus tumor [8], composed of cells resembling the modified smooth muscle cells of the normal glomus body. It has been acknowledged that myofibroma/myofibromatosis represent morphological features along the spectrum of myopericytic neoplasms (Table 11.6) instead of fibroblastic/myofibroblastic tumors (group 2), which were included in the past. Angioleiomyoma (vascular leiomyoma) which typically presents as a painful lesion in the distal extremities of middle-aged adults has now been included in this group [9, 10].
Table 11.6




Group 5 – Pericytic (perivascular) tumors
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree