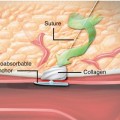
Fig. 11.1
The role of platelets in acute coronary syndrome and targets of platelet inhibitors
Aspirin
Pharmacokinetics
Aspirin, a derivative of salicylic acid whose origins date back to Hippocrates and a powder he made from the bark and leaves of the willow tree, was first commercially produced in 1900 by Felix Hoffmann, a chemist working for Bayer [1]. Aspirin irreversibly inhibits platelet activation through acetylation of the platelet cyclooxygenase-1 enzyme. Blockage of the cyclooxygenase-1 enzyme prevents the conversion of arachidonic acid to prostaglandin H2, which, in normal conditions, is then converted into thromboxane A2. Platelets possess a thromboxane A2 receptor which, upon binding with thromboxane A2, promotes platelet activation. Thus, as a result of inhibited thromboxane A2 production, platelet activation is inhibited. Because the inhibition of the cyclooxygenase-1 enzyme is irreversible and the platelets cannot create more of the enzyme, the effects last for the lifespan of the platelet (7–10 days).
Clinical Evidence for Use
Aspirin (preferably given prior to the procedure) is indicated as an adjunctive pharmacologic therapy in all coronary interventions. In the pre-stent era, Schwartz et al. evaluated aspirin loading prior to PCI in 376 patients undergoing balloon angioplasty. Patients were randomized to receive either a combination of aspirin/dipyridamole (330 mg/75 mg) or placebo 24 h prior to PTCA. Treatment was continued in patients with a successfully dilated vessel until follow-up angiography, which was performed 4–7 months after PTCA. While the investigators had proposed that the combination of aspirin/dipyridamole would reduce restenosis (it did not), they did demonstrate a significant reduction in the incidence of periprocedural Q wave myocardial infarction (6.9 % in placebo vs. 1.6 % in treatment arm; p = 0.011) [2].
Similar to pre-PCI loading, there is also a single randomized trial for long-term continuation of aspirin post-PCI. In this study, 752 patients were randomly assigned to aspirin (325 mg daily), the thromboxane A2 receptor antagonist sulotroban (800 mg QID), or placebo, started within 6 h before PTCA and continued for 6 months. The results demonstrated that while there was again no difference in restenosis, the rate of myocardial infarction at 6 months was significantly reduced by antithromboxane therapy: 1.2 % in aspirin group, 1.8 % in the sulotroban group, and 5.7 % in the placebo group [3].
The most comprehensive evaluation for dosing of aspirin in the setting of acute coronary syndromes comes from the Antithrombotic Trialists’ Collaboration, which made indirect comparisons between either high or low doses of aspirin. This analysis reviewed 287 studies involving both comparisons of antiplatelet therapy versus control and comparisons of different antiplatelet regimens. While a loading dose of at least 150 mg of aspirin was found to be of significant advantage up front, the benefits of long-term aspirin therapy were similarly independent of whether the maintenance dosing was high dose (>150 mg) or low dose (<150) [4]. Higher doses of aspirin are associated with increased rates of both minor as well as major and intracranial bleeding events. In the CURE study, three aspirin dose groups (≤100, 101–199, and ≥200 mg) were evaluated with or without clopidogrel. Results from this study demonstrated an increased incidence of major bleeding associated with increasing aspirin dose both in the group without concomitant clopidogrel (1.9 % for ≤100 mg, 2.8 % for 101–199 mg, and 3.7 % for ≥200 mg; p = 0.0001) and for the clopidogrel-treated group (3.0 % for ≤100 mg, 3.4 % for 101–199 mg, and 4.9 for ≥200 mg; p = 0.0009). In addition, there was no benefit in cardiovascular death, myocardial infarction, or stoke associated with the higher dose of aspirin [5].
The ACCF/AHA guidelines recommend a loading dose of 325 mg in the setting of STEMI and pre-PCI, and the most updated guidelines now recommend that after PCI, it is reasonable to use 81 mg of aspirin as the maintenance dose [6] (Table 11.1).
Table 11.1
ACCF/AHA guidelines for oral antiplatelet therapy
Class I | |
1. | Patients already taking daily aspirin therapy should take 81–325 mg before PCI (level of evidence B) |
2. | Patients not on aspirin therapy should be given nonenteric aspirin 325 mg before PCI (level of evidence B) |
3. | After PCI, use of aspirin should be continued indefinitely (level of evidence A) |
4. | A loading dose of a P2Y12 receptor inhibitor should be given to patients undergoing PCI with stenting (level of evidence A). Options include: |
(a) Clopidogrel 600 mg (ACS and non-ACS patients) (level of evidence B) | |
(b) Prasugrel 60 mg (ACS patients) (level of evidence B) | |
(c) Ticagrelor 180 mg (ACS patients) (level of evidence B) | |
5. | The loading dose of clopidogrel for patients undergoing PCI after fibrinolytic therapy should be 300 mg within 24 h and 600 mg more than 24 h after receiving fibrinolytic therapy (level of evidence C) |
6. | Patients should be counseled on the need for and risks of DAPT before placement of intracoronary stents, especially DES, and alternative therapies should be pursued if patients are unwilling or unable to comply with the recommended duration of DAPT (level of evidence C) |
7. | The duration of P2Y12 inhibitor therapy after stent implantation should generally be as follows: |
(a) In patients receiving a stent (BMS or DES) during PCI for ACS, P2Y12 inhibitor therapy should be given for at least 12 months. Options include clopidogrel 75 mg daily, prasugrel 10 mg daily, and ticagrelor 90 mg twice daily (level of evidence B) | |
(b) In patients receiving DES for a non-ACS indication, clopidogrel 75 mg daily should be given for at least 12 months if patients are not at high risk of bleeding (level of evidence B) | |
(c) In patients receiving BMS for a non-ACS indication, clopidogrel should be given for a minimum of 1 month and ideally up to 12 months (unless the patient is at increased risk of bleeding; then, it should be given for a minimum of 2 weeks) (level of evidence B) | |
Class IIa | |
1. | After PCI, it is reasonable to use aspirin 81 mg per day in preference to higher maintenance doses (level of evidence B) |
2. | If the risk of morbidity from bleeding outweighs the anticipated benefit afforded by a recommended duration of P2Y12 inhibitor therapy after stent implantation, earlier discontinuation (e.g., <12 months) of P2Y12 inhibitor therapy is reasonable (level of evidence C) |
Class IIb | |
1. | Continuation of DAPT beyond 12 months may be considered in patients undergoing DES implantation (level of evidence C) |
Class III: HARM | |
Prasugrel should not be administered to patients with a prior history of stroke or transient ischemic attack (level of evidence B) | |
Thienopyridines and Ticagrelor
Pharmacokinetics
In the modern PCI era with both bare-metal and drug-eluting stents, dual antiplatelet therapy with aspirin and a thienopyridine has become the standard of treatment. The thienopyridines that are used post-PCI with aspirin are ticlopidine, clopidogrel, and prasugrel. While aspirin inhibits platelet activation, thienopyridines inhibit both platelet activation and aggregation. These effects on platelets are due both to their inhibition of the activation of the GPIIb/IIIa receptor responsible for platelet linking and the binding of fibrinogen and to their inhibition of platelet ADP receptor P2Y12. The inhibition of the platelet ADP receptor P2Y12 prevents platelet activation and aggregation by downregulating platelet degranulation and the subsequent release of prothrombotic and inflammatory mediators [7] (Fig. 11.1). The mechanism of action of ticlopidine, clopidogrel, and prasugrel all involve inhibition of the platelet ADP receptor P2Y12 by blocking the ADP binding site. Like aspirin, this results in an irreversible inhibition of the platelet, and thus, the effects last for the 7–10 day lifespan of the platelet. The newest oral antiplatelet agent, ticagrelor, is an exception to this irreversible inhibition. Although ticagrelor also blocks the ADP receptor P2Y12 like the thienopyridines, it does so at a different binding site from ADP, and as a result, its effects are reversible [8].
Clinical Evidence for Use
The evidence in favor of the use of thienopyridines in the setting of STEMI and during PCI is supported by significant clinical evidence. The COMMIT study randomized 45,852 patients presenting with acute myocardial infarction to clopidogrel 75 mg daily with no loading dose vs. placebo, in addition to aspirin 162 mg daily. Within the trial, 93 % of the patients presented with ST segment elevation myocardial infarction. In this study, clopidogrel (or placebo) was continued for the duration of the hospitalization or up to 4 weeks with mean treatment duration of 15 days. The composite end point of death, reinfarction, or stroke was significantly reduced in the group receiving clopidogrel as compared to placebo (9.2 % vs. 10.1 %; p = 0.002). There was no significant difference in combined rates for fatal bleeds, blood product transfusion, or intracerebral hemorrhage (0.58 % vs. 0.55 %; p = NS) [9].
Clopidogrel loading prior to PCI has also been demonstrated to be beneficial. The PCI-CLARITY trial, a continuation of the CLARITY–TIMI 28 study, prospectively randomized 1,863 patients undergoing PCI after mandatory angiography in the CLARITY–TIMI 28 trial to either clopidogrel (300 mg oral loading dose followed by 75 mg daily) or placebo in addition to aspirin. Pretreatment with clopidogrel led to a significant reduction in the composite end point of cardiovascular death, recurrent MI, or stroke from PCI to 30 days post-randomization (3.6 % in clopidogrel group vs. 6.2 % in the placebo group; p = 0.008). Pretreatment with clopidogrel also reduced the incidence of MI or stroke prior to PCI (4.0 % vs. 6.2 %; p = 0.03). Importantly, as in the COMMIT study, there was no significant difference in both major and minor bleeding risks (2 % vs. 1.9 %; p = NS) [10].
Prasugrel is one of the newer members of the thienopyridine family. Like clopidogrel, prasugrel is a prodrug that requires conversion to an active metabolite in order to become active. What differentiates prasugrel from clopidogrel is that prasugrel is converted to its active form more quickly and inhibits the ADP binding site of the ADP receptor P2Y12 more potently. The TRITON–TIMI 38 trial evaluated the safety and efficacy of prasugrel in a double-blinded study involving 13,600 patients presenting with acute coronary syndrome undergoing scheduled percutaneous intervention. Patients were randomized to receive either prasugrel (a 60 mg loading dose followed by 10 mg daily) or clopidogrel (a 300 mg loading dose followed by 75 mg daily) for 6–15 months. The primary end point was death from cardiovascular causes, nonfatal MI, or nonfatal stroke. Of the patients included in the study, 26 % presented with STEMI. The primary end point occurred in 12.1 % of clopidogrel patients and 9.9 % of prasugrel patients (p < 0.001). This was driven in part by a significant reduction in the rate of myocardial infarction (9.7 % clopidogrel vs. 7.4 % prasugrel; p < 0.001). Additional benefits of prasugrel included decreased stent thrombosis (3.7 % clopidogrel vs. 2.5 % prasugrel; p < 0.001), and these benefits carried over to the STEMI subset. The benefit of prasugrel in the primary efficacy end point was seen within the first 24 h of randomization and persisted through 15 months of follow-up. Certain subgroups of patients also had a significant benefit with prasugrel, including diabetics and patients receiving Gp IIb/IIIa inhibitors. These improved efficacy outcomes, presumably due to the more potent pharmacokinetics, were however associated with an increased rate of bleeding. Major bleeding was seen in 2.4 % of prasugrel patients compared to 1.8 % seen in the clopidogrel group, including a significant increase in life-threatening bleeding (1.4 % prasugrel vs. 0.9 % clopidogrel; p = 0.01) and fatal bleeding events (0.4 % prasugrel vs. 0.1 % clopidogrel; p = 0.002). Three groups in particular were found to not have a clinical benefit from prasugrel: patients with prior TIA or stroke, patients with a weight <60 kg, and patients >75 years in age. For patients with prior TIA or stroke, there was a net harm from prasugrel administration as compared to clopidogrel [11]. Based on this data, the FDA declared prasugrel to be contraindicated in patients with prior TIA or stroke.
The final current oral antiplatelet agent is ticagrelor, a reversible P2Y12 inhibitor. Ticagrelor was recently evaluated in the PLATO trial, which randomized 18,600 patients presenting with ACS to either clopidogrel (300 mg or 600 mg loading dose followed by 75 mg daily) or ticagrelor (180 mg loading dose followed by 90 mg twice daily). A total of 38 % of patients presented with STEMI. The primary end point of death from vascular causes or cerebrovascular causes, or death from an unknown cause, occurred in 9.8 % in the ticagrelor group vs. 11.7 % in the clopidogrel group (p < 0.001). Furthermore, the composite of all-cause death, MI, or stroke was also reduced in the ticagrelor group (10.2 % vs. 12.3 %; p < 0.001). Similarly, the rate of stent thrombosis was also lower among those patients receiving ticagrelor (1.3 % vs. 1.9 %; p = 0.009). While the rates of major bleeding were similar between the two groups, intracranial bleeding episodes were more common among the ticagrelor group. Lastly, there was no significant difference in the incidence of stroke, including hemorrhagic stroke [12]. Based on the PLATO trial, ticagrelor was FDA approved for patients with acute coronary syndromes in July 2011.
Heparin and Glycoprotein IIb/IIIa Inhibitors
According to the most recent ACC/AHA guidelines, use of anticoagulation therapy in addition to antiplatelet therapy is a Class 1 indication in both STEMI (level of evidence B) and NSTEMI (level of evidence B). Unfractionated heparin has historically been the most widely used drug to achieve therapeutic systemic anticoagulation, with low-molecular-weight heparin and fondaparinux being more recent additions [13].
Unfractionated Heparin (UFH)
Pharmacokinetics
Unfractionated heparin has been the standard anticoagulant used for percutaneous coronary interventions around the world. It is relatively safe and inexpensive and, despite some drawbacks, works well in preventing thrombotic complications during PCI. Heparin exerts its action by enhancing the effects of antithrombin III which in turn inactivates factors IIa, IXa, Xa, XIa, and XIIa [14]. It cannot be absorbed orally and is administered parentally either as repeated boluses or infusion. The anticoagulant effects of UFH also vary across patients and require monitoring of the activated clotting time (ACT) in order to achieve the desired level of anticoagulation. Its variable intra- and interpatient effect and the need for monitoring to ensure adequate anticoagulation reflect its most significant limitation. Unfractionated heparin is prepared as polysaccharide chains of variable length and weight with varying affinity for binding with plasma proteins and cells, which limits its bioavailability [15]. In addition, there is a risk of the development of heparin-induced thrombocytopenia and the inability of heparin to inhibit clot-bound thrombin [16].
Clinical Evidence for Use
The 2011 ACC/AHA PCI guidelines have cited use of UFH during elective PCI as a Class 1 indication with level of evidence C (expert consensus). This underscored the absence of randomized controlled trial data supporting routine use of anticoagulation.
Studies during the balloon angioplasty and early stent era have shown a correlation between ACT levels and ischemic events and abrupt vessel closure [17, 18]. A meta-analysis comparing heparin plus aspirin to aspirin alone in patients with unstable angina found a 33 % reduction in mortality and myocardial infarction [19]. Heparin has a narrow therapeutic window and retrospective analysis has not identified a specific ACT value above which ischemic events are prevented without increase in bleeding [20, 21]. ACC/AHA guidelines suggest maintaining an ACT of 200–250 when using UFH + GPI and 250–300 when using UFH alone (300–350 for Hemochron ©). Empiric fixed dose vs. weight-based heparin dosing has also been studied, with both approaches showing equally effective results [22]. The guidelines do not advocate routine prolonged post-PCI use of heparin as it has been shown to be associated with increased risk of access-site bleeding without any benefit in reducing ischemic events [23].
Some recent data has questioned the routine use of anticoagulation in elective PCI. Seven hundred patients undergoing planned PCI and already on aspirin and a thienopyridine were randomized to receive UFH or no anticoagulation during their procedures. The study found decreased bleeding without an increase in ischemic or thrombotic events in the no-UFH arm, suggesting at least the possibility that routine, uncomplicated elective PCI could be performed safely with antiplatelet therapy alone [24].
The use of UFH in ACS is more validated with the guidelines, giving it a Class 1 indication (level of evidence B) for both STEMI and UA/NSTEMI populations undergoing PCI [25, 26]. The thrombotic milieu resulting from an ACS is significantly different from that during elective PCI and justifies the use of systemic anticoagulation. A meta-analysis, which included patients with ACS, found a higher incidence of ischemic and thrombotic events at lower ACTs [20], reinforcing the need for systemic anticoagulation.
LMWH: Enoxaparin
Pharmacokinetics
Low-molecular-weight heparins are fragments of unfractionated heparin with a mean molecular weight of about 5,000. There are several attributes that make LMWH more attractive than UFH: Longer half-life, dose-independent clearance, and better bioavailability allow for a more predictable anticoagulant response. LMWH have a greater ratio of anti-factor Xa activity to anti-factor IIa activity, which reduces the generation and activation of thrombin [27]. LMWH are also less apt to induce platelet activation, release of the von Willebrand factor, and cause inflammation [28]. Of the several LMWH formulations available, enoxaparin is the most widely available and has the strongest level of data backing its use in the catheterization lab. It can be given subcutaneously, or if rapid onset is needed, it may be given intravenously as well. Enoxaparin is renally excreted and its dose must be adjusted for CrCl < 30.
Clinical Evidence for Use
ExTRACT-TIMI 25 was a study comparing enoxaparin to UFH in conjunction with thrombolytic therapy in STEMI patients and found higher bleeding rates with enoxaparin [29]. However, subgroup analysis of patients who underwent PCI demonstrated a reduced risk of 30-day death/recurrent MI with LMWH compared with UFH (10.7 % vs. 13.8 %) without a significant increase in major bleeding (1.4 % vs. 1.6 %) [30]. This finding was duplicated by a prospective single-center nonrandomized comparison of outcomes in STEMI patients undergoing primary PCI with reduced in-hospital mortality with LMWH (OR, 0.32; 95 % CI, 0.12–0.85), as well as a reduction in 30-day mortality (OR, 0.4; 95 % CI, 0.17–0.99) without an increase in major (p = 0.34) or minor (p = 0.65) bleeding [31]. However, ATOLL, a large study, randomized acute myocardial infarction patients going for primary PCI to enoxaparin or UFH and found no difference in 30-day mortality or MI [32]. The main secondary end point of death, recurrent MI or acute coronary syndrome, or urgent revascularization occurred significantly less often with enoxaparin. Bleeding was similar in both groups.
Recent publication of a meta-analysis has again suggested that enoxaparin use compared to heparin leads to lower mortality and reduced bleeding. The subgroup of patients that were treated with primary PCI had reduced risk of mortality (RR 0.52, 95 % CI, 0.42–0.64) and major bleeding (RR 0.72, 95 % CI, 0.56–0.93) [33].
The majority of data evaluating LMWH use in NSTEMI has been in the conservatively managed population. These data suggest that enoxaparin use may decrease death and MI rates with uncertain effects on bleeding rates. Two studies have evaluated enoxaparin use for inpatients managed with an early invasive strategy. The SYNERGY trial randomized 10,027 patients with NSTEMI to enoxaparin or heparin and found no difference in death or MI at 30 days, 6 months, or 1 year, but there was significantly higher in-hospital bleeding with enoxaparin [34]. In the A to Z trial, enoxaparin was again compared to UFH in the NSTEMI population. The results showed no significant decrease in 30-day death, MI, or recurrent ischemia, but again there was a higher bleeding rate. However, only half of the patients were managed invasively and post hoc analysis suggested the differences were limited to the conservatively managed patients [35].
In elective PCI, STEEPLE, a large trial, randomized patients to either enoxaparin or adjusted UFH with concomitant GPIIb/IIIa and thienopyridine use and found no difference in ischemic outcomes with significantly lower bleeding with enoxaparin [36]. Due to the lack of a rapid assay to evaluate the effect of LMWH, as well as a lack of compelling evidence for its benefits over UFH in the setting of PCI, UFH remains the heparin of choice during both elective and emergent PCI.
Fondaparinux
Pharmacokinetics
Fondaparinux, a synthetic pentasaccharide, indirectly inhibits factor Xa by binding to antithrombin and inhibits thrombin generation. Fondaparinux has complete bioavailability when given subcutaneously and does not undergo metabolism [37]. It exhibits a linear pharmacokinetic profile with little inter- or intrapatient variability. Its elimination half-life is 15 h, allowing once-daily administration [38]. It does not exhibit protein binding, reducing the chances for a variable response and drug interactions [39]. It has rapid onset in 1–3 h and is renally cleared [40].
Clinical Evidence for Use
The use of fondaparinux in the catheterization lab during PCI has been limited due to the results of the OASIS-5 and OASIS-6 trials [37]. Both trials showed increased risk of catheter thrombosis when fondaparinux was used as the sole antithrombotic during PCI. Subsequent trials have shown that addition of dose-adjusted UFH in patients who are already on fondaparinux and going for PCI removed that risk [41]. At present, the use of fondaparinux as a sole antithrombotic agent during PCI is a Class III indication according to the ACC/AHA guidelines and the recommendation is to use additional dose-adjusted UFH in patients going for PCI [42].
GPIIb/IIIa Inhibitors
Pharmacokinetics
GPIIb/IIIa are the most abundant receptors on the platelet surface and have several different binding sites that respond to various stimuli [43]. However, the ones for fibrinogen are the most potent and, once activated, form ligands between platelets, allowing for cross-linking and, ultimately, thrombus formation [44]. As a result, GPIIb/IIIa receptor antagonists that block platelet aggregation and thrombus formation are the most potent antiplatelet agents, much more so than aspirin or thienopyridines [45]. Three main GPIIb/IIIa drugs are widely available: abciximab, eptifibatide, and tirofiban. All three drugs are administered intravenously, and large-scale clinical trials have demonstrated both clinical benefit and safety for adjunctive therapy in percutaneous coronary intervention.
Abciximab was the first to be developed and is a chimeric monoclonal antibody that binds nonspecifically to the GPIIb/IIIa receptor. Despite randomized data supporting its use, concerns regarding immunogenicity and nonspecificity led to development of the so-called small-molecule GPIIb/IIIa receptor inhibitors: eptifibatide and tirofiban. Both are highly specific and have shorter half-lives [43].
Clinical Evidence for Use
The current data has not been able to show clear benefit of GPIIb/IIIa during elective PCI in stable patients. The ambiguity of the timing and appropriate situation for GPIIb/IIIa use during elective PCI is reflected in 2011 ACC/AHA guidelines that give a Class IIa indication for its use in the absence of up-front thienopyridines and Class IIb when the patient has already been pretreated with dual antiplatelet therapy [46]. The TARGET trial found abciximab superior to tirofiban in reducing death, myocardial infarction, and TVR [47]. A large proportion of patients were loaded with clopidogrel 300 mg 6 h pre-procedure and both groups appeared to benefit. Abciximab was widely utilized for elective PCI until both ISAR-REACT and ISAR-SWEET trials evaluated abciximab versus placebo in the setting of preloading with clopidogrel 600 mg and failed to show a reduction in MACE at 30 days, suggesting up-front thienopyridines neutralize the benefit of GPIIb/IIIa administration [48, 49].
Contemporary use of GPIIb/IIIa during elective PCI appears to be based on the presence of high-risk features: coronary thrombus, vessel closure, no reflow/slow flow, and lack of up-front thienopyridines, a practice that is supported by the European guidelines and data from REPLACE-2, where bivalirudin and provisional GPIIb/IIIa had decreased MACE and bleeding as compared to UFH and planned GPIIb/IIIa [50, 51].
The use of GPIIb/IIIa for high-risk patients has extended into the NSTEMI population as well. The 2011 guidelines gave a Class 1 indication to UFH and adjunctive GPIIb/IIIa use in the setting of high-risk features (markedly elevated troponin, anterior MI, large thrombus burden) in the absence of thienopyridine use, and Class IIa when patients were preloaded with clopidogrel [46]. Most trials demonstrating benefit of GPIIb/IIIa in reducing composite ischemic events (EPILOG, CAPTURE, EPIC, RESTORE) were conducted in the era where pretreatment with a thienopyridine was not routine and thus the results may not be directly applicable to contemporary clinical practice [52–56]. As a result, the current guidelines have abandoned up-front treatment with GPIIb/IIIa antagonists in favor of provisional intra-procedure use, based on data that showed lack of benefit and possible increased risk of major bleeding with the former strategy [57].
ISAR-REACT 2 did show abciximab to reduce composite end points in NSTEMI patients going for primary PCI in the setting of preloading with aspirin and clopidogrel 600 mg. However, when analyzed on the basis of positive or negative troponins, the result was clearly limited to the former subset [58]. Tirofiban use during PCI in addition to aspirin and clopidogrel pretreatment also showed decreased ischemic and thrombotic events in diabetics with single vessel disease, multivessel PCI, or NSTEMI patients being treated with early invasive strategy [59].
Data evaluating the use of GPIIb/IIIa inhibitors during PCI for STEMI predates the era of dual antiplatelet therapy as well. The ADMIRAL (platelet glycoprotein IIb/IIIa inhibition with coronary stenting for acute myocardial infarction) study randomized STEMI patients to abciximab or placebo prior to PCI and showed a 51 % relative risk reduction in death and reinfarction at 30 days [60]. Though follow-up of the patients from ADMIRAL showed sustained benefit of adjunctive abciximab use, the study was subject to significant limitations [61]. A similar trial of 400 randomized STEMI patients to abciximab versus placebo demonstrated a significant reduction in mortality, earlier ST segment resolution, and decreased infarct size [62]. However, both studies showed no improvement in TVR or restenosis. Multicenter randomized studies comparing GPIIb/IIIa with placebo in the setting of STEMI and dual antiplatelet therapy have not been done, but the combination of UFH and eptifibatide was inferior to bivalirudin in the HORIZONS-AMI trial [63].
Clinical outcomes in current era of PCI for elective, NSTEMI, or STEMI population have markedly benefited from improved equipment and stent design, early and effective up-front oral antiplatelet therapy (clopidogrel, prasugrel), and improved anticoagulation (bivalirudin). The additional use of GPIIb/IIIa treads a fine line between clinical benefit and increased bleeding and seems to be limited to patients who have clinical or angiographic high-risk features (troponin elevation, large thrombus burden, or acute vessel closure).
Intravenous Direct Thrombin Inhibitors
Hirudin
Hirudin is a naturally occurring 65-amino acid polypeptide originally isolated from the medicinal leech, Hirudo medicinalis, and more recently available through recombinant DNA technology. Hirudin blocks the effects of thrombin on the hemostatic system, including the conversion of fibrinogen to fibrin, activation of coagulation factors XI and XIII, positive feedback activation of coagulation factors V and VIII, and thrombin-mediated platelet activation [64]. Administered by intravenous or subcutaneous injection, it has a plasma half-life of approximately 40 min after intravenous injection and 1–3 h after subcutaneous injection. It is primarily excreted renally. The anticoagulant effects of hirudin can be monitored in the laboratory using the activated partial thromboplastin time (aPTT) [65, 66]. Despite having been studied in patients with acute coronary syndromes and percutaneous coronary interventions, it has never assumed use as a frontline therapy.
The OASIS pilot study [67] randomized patients with an acute coronary syndrome without persistent ST elevation to a 72-h infusion of low-dose or medium-dose hirudin infusion or unfractionated heparin (UFH). Hirudin was associated with a reduction in the composite primary outcome of cardiovascular death, myocardial infarction, or refractory angina at 7 days, with a similar incidence of major bleeding. However, the study was not powered for clinical outcomes. In the follow-up OASIS-2 trial, patients with ACS were randomized to medium-dose hirudin or heparin for 72 h. Hirudin was associated with a significantly increased risk of major bleeding compared with UFH [68]. Several large randomized trials followed to evaluate hirudin as an adjunct to thrombolytic therapy in patients with ACS but were terminated because of unacceptably high rates of major hemorrhage [67–71].
Given the bleeding complications, two of the trials, TIMI9A and GUSTO-IIb [67, 68], were restarted with lower doses of hirudin and UFH. The GUSTO-IIb trial showed a small reduction in the primary composite outcome of death or myocardial infarction with hirudin compared with heparin at 30 days. There was a reduction in death or myocardial infarction with hirudin during the first 24 h, and subgroup analysis suggested a highly significant 39 % reduction in death or myocardial infarction at 30 days in the hirudin-treated group. However, in the TIMI-9B trial, no benefit of hirudin over UFH was observed. Neither TIMI-9B nor GUSTO-IIb demonstrated an increase in major or intracranial bleeding with hirudin. Similarly, the HIT-4 trial failed to show any difference between clinical outcomes or major bleeding when comparing hirudin with heparin as adjunctive therapy to streptokinase in acute myocardial infarction [72].
Due to the lack of convincing evidence supporting efficacy of hirudin over heparin and the concern for intracranial bleeding, it was never approved for use in percutaneous coronary interventions. Its only clinical role remains as anticoagulation in patients with heparin-induced thrombocytopenia.
Argatroban
Argatroban is a synthetic, small-molecule direct thrombin inhibitor that is approved in the USA for prophylaxis or treatment of thrombosis in patients with heparin-induced thrombocytopenia (HIT) and for anticoagulation of HIT patients undergoing PCI [73]. Argatroban is parenteral and the polypeptide binds to and inhibits the active site of thrombin. Unlike bivalirudin, argatroban is predominantly eliminated through the liver and plasma concentrations are not influenced by renal function [72]. It has a rapid onset of action and a half-life of 45 min (extended to 2.5 h in patients with hepatic impairment) [74, 75]. Argatroban increases the activated partial thromboplastin time, prothrombin time, and thrombin clotting time in a dose-dependent manner. The activated partial thromboplastin time is commonly used to monitor its anticoagulant effects. Like bivalirudin, argatroban has no known reversal antidote.
Clinical Evidence for Use
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree