Pericholecystic free fluid, intraluminal or pericholecystic hematoma, or GB wall thickening
 Poor definition of GB wall, abnormal GB contour, or collapsed GB, particularly with surrounding pericholecystic fluid, suggest GB perforation
Poor definition of GB wall, abnormal GB contour, or collapsed GB, particularly with surrounding pericholecystic fluid, suggest GB perforation• Bile duct injuries
 Proximal biliary dilatation with abrupt narrowing of duct at site of bile duct laceration or stricture
Proximal biliary dilatation with abrupt narrowing of duct at site of bile duct laceration or stricture
 MR hepatobiliary contrast agents (e.g., Eovist) can be utilized to directly visualize leak or stricture
MR hepatobiliary contrast agents (e.g., Eovist) can be utilized to directly visualize leak or stricture
 Proximal biliary dilatation with abrupt narrowing of duct at site of bile duct laceration or stricture
Proximal biliary dilatation with abrupt narrowing of duct at site of bile duct laceration or stricture MR hepatobiliary contrast agents (e.g., Eovist) can be utilized to directly visualize leak or stricture
MR hepatobiliary contrast agents (e.g., Eovist) can be utilized to directly visualize leak or stricture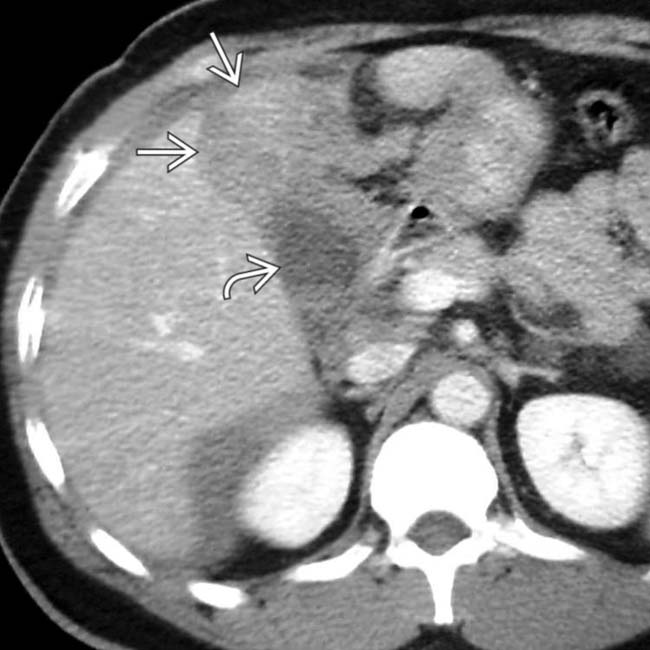
 separating the gallbladder
separating the gallbladder  from its normal location in the gallbladder fossa. The patient was taken to surgery where the gallbladder was found to be “avulsed” from its hepatic attachment and leaking bile.
from its normal location in the gallbladder fossa. The patient was taken to surgery where the gallbladder was found to be “avulsed” from its hepatic attachment and leaking bile.
 immediately adjacent to a surgical clip
immediately adjacent to a surgical clip  , in keeping with an iatrogenic stricture. The stricture in this case ultimately required hepaticojejunostomy.
, in keeping with an iatrogenic stricture. The stricture in this case ultimately required hepaticojejunostomy.
 and small hemoperitoneum. The depth of the laceration raised concern for biliary transection. The patient developed signs of bile peritonitis.
and small hemoperitoneum. The depth of the laceration raised concern for biliary transection. The patient developed signs of bile peritonitis.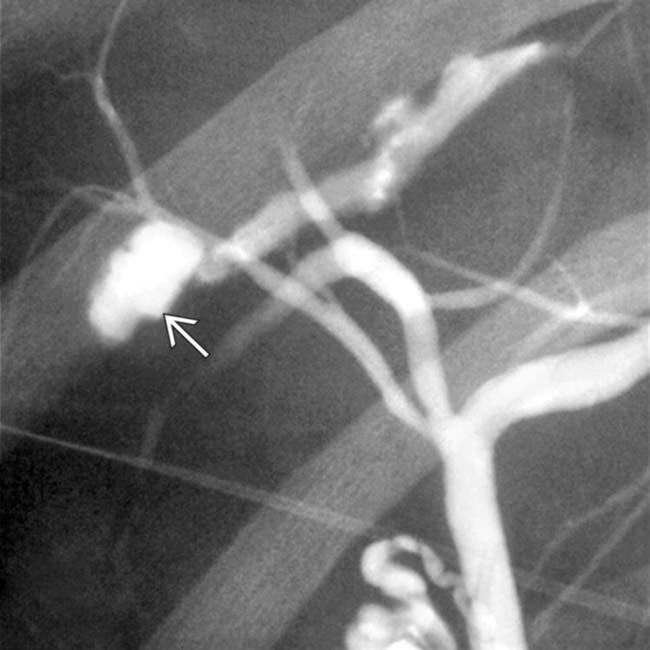
 . The patient was successfully treated with biliary stenting without surgery. The biliary and hepatic injuries resolved.
. The patient was successfully treated with biliary stenting without surgery. The biliary and hepatic injuries resolved.IMAGING
General Features
• Location
 Postoperative injuries: Common hepatic duct (45-64%) and hepatic hilum (20-33%) most common locations
Postoperative injuries: Common hepatic duct (45-64%) and hepatic hilum (20-33%) most common locations
 Postoperative injuries: Common hepatic duct (45-64%) and hepatic hilum (20-33%) most common locations
Postoperative injuries: Common hepatic duct (45-64%) and hepatic hilum (20-33%) most common locations– Most common injury is common duct transection (common duct mistaken for cystic duct during cholecystectomy)
– Postoperative bile leaks usually arise from cystic duct stump, duct of Luschka (accessory duct in right hepatic lobe that traverses GB fossa), and GB bed
CT Findings
• Gallbladder injury
 Imaging findings may vary depending on degree of injury, and some mild gallbladder contusions may be invisible on imaging
Imaging findings may vary depending on degree of injury, and some mild gallbladder contusions may be invisible on imaging
 Presence of pericholecystic free fluid, intraluminal or pericholecystic high-density hematoma, or gallbladder wall thickening should raise concern for injury
Presence of pericholecystic free fluid, intraluminal or pericholecystic high-density hematoma, or gallbladder wall thickening should raise concern for injury
 Poor definition of gallbladder wall (i.e., sites of nonenhancement), abnormal GB contour, or collapsed GB, particularly with surrounding pericholecystic fluid, raises suspicion for GB perforation
Poor definition of gallbladder wall (i.e., sites of nonenhancement), abnormal GB contour, or collapsed GB, particularly with surrounding pericholecystic fluid, raises suspicion for GB perforation
 Imaging findings may vary depending on degree of injury, and some mild gallbladder contusions may be invisible on imaging
Imaging findings may vary depending on degree of injury, and some mild gallbladder contusions may be invisible on imaging Presence of pericholecystic free fluid, intraluminal or pericholecystic high-density hematoma, or gallbladder wall thickening should raise concern for injury
Presence of pericholecystic free fluid, intraluminal or pericholecystic high-density hematoma, or gallbladder wall thickening should raise concern for injury Poor definition of gallbladder wall (i.e., sites of nonenhancement), abnormal GB contour, or collapsed GB, particularly with surrounding pericholecystic fluid, raises suspicion for GB perforation
Poor definition of gallbladder wall (i.e., sites of nonenhancement), abnormal GB contour, or collapsed GB, particularly with surrounding pericholecystic fluid, raises suspicion for GB perforation• Bile duct injuries
 Free fluid or loculated collections (bilomas) in right upper quadrant (either intra- or extrahepatic) adjacent to biliary tree
Free fluid or loculated collections (bilomas) in right upper quadrant (either intra- or extrahepatic) adjacent to biliary tree
 Proximal biliary dilatation with abrupt narrowing of duct at site of bile duct laceration or stricture
Proximal biliary dilatation with abrupt narrowing of duct at site of bile duct laceration or stricture
 Free fluid or loculated collections (bilomas) in right upper quadrant (either intra- or extrahepatic) adjacent to biliary tree
Free fluid or loculated collections (bilomas) in right upper quadrant (either intra- or extrahepatic) adjacent to biliary tree– CT cannot differentiate bilomas from other common post-traumatic and postsurgical fluid collections (hematomas, seromas, lymphocele, abscess)
 Proximal biliary dilatation with abrupt narrowing of duct at site of bile duct laceration or stricture
Proximal biliary dilatation with abrupt narrowing of duct at site of bile duct laceration or stricture• Helical CT cholangiography (after IV administration of biliary contrast material) to verify and localize bile duct leakage
• Presence of biliary dilatation, configuration of injured bile duct, and ancillary abdominal findings