Diagnosis requires excluding other causes of biliary dilatation, including tumor, stone, or stricture
• Classified into 5 types based on Todani classification
 Type III: Dilation limited to intraduodenal segment of ED (a.k.a. choledochocele), with dilated segment of duct located within duodenal wall
Type III: Dilation limited to intraduodenal segment of ED (a.k.a. choledochocele), with dilated segment of duct located within duodenal wall
 Type IV: Presence of multiple biliary cysts, at least 1 of which must involve extrahepatic bile duct
Type IV: Presence of multiple biliary cysts, at least 1 of which must involve extrahepatic bile duct
 Type III: Dilation limited to intraduodenal segment of ED (a.k.a. choledochocele), with dilated segment of duct located within duodenal wall
Type III: Dilation limited to intraduodenal segment of ED (a.k.a. choledochocele), with dilated segment of duct located within duodenal wall Type IV: Presence of multiple biliary cysts, at least 1 of which must involve extrahepatic bile duct
Type IV: Presence of multiple biliary cysts, at least 1 of which must involve extrahepatic bile duct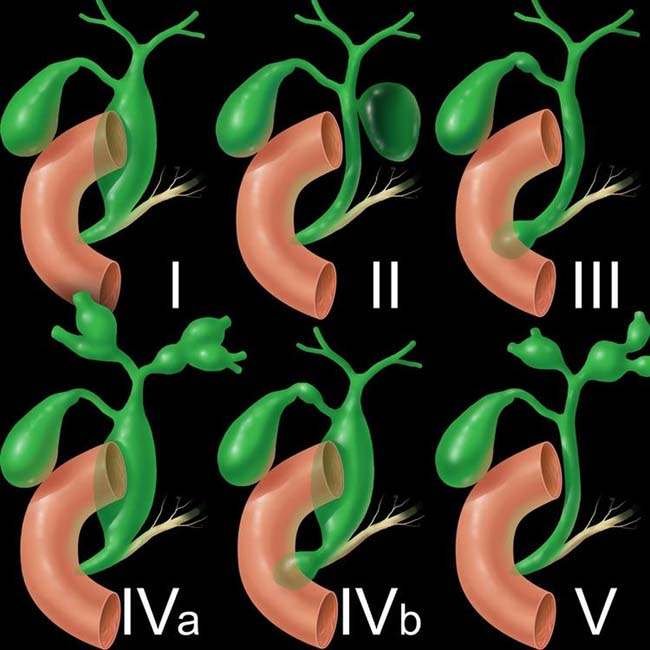
 . Type I lesions are the most common type of choledochal cyst.
. Type I lesions are the most common type of choledochal cyst.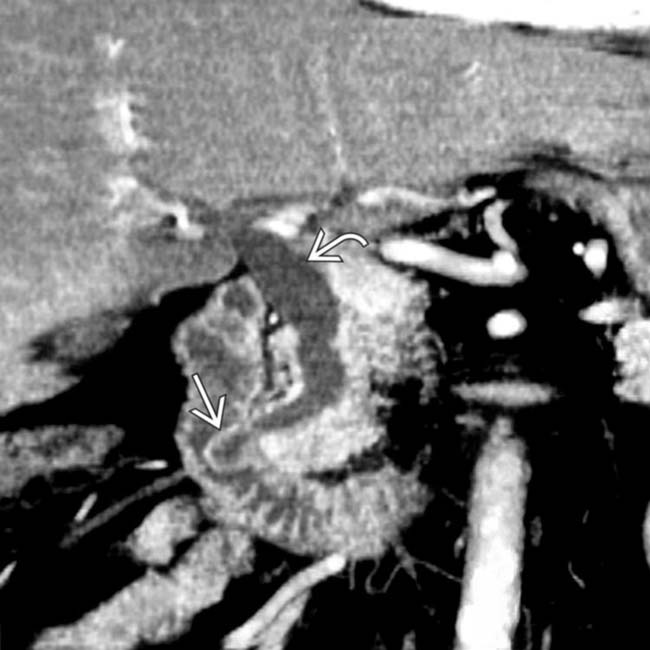
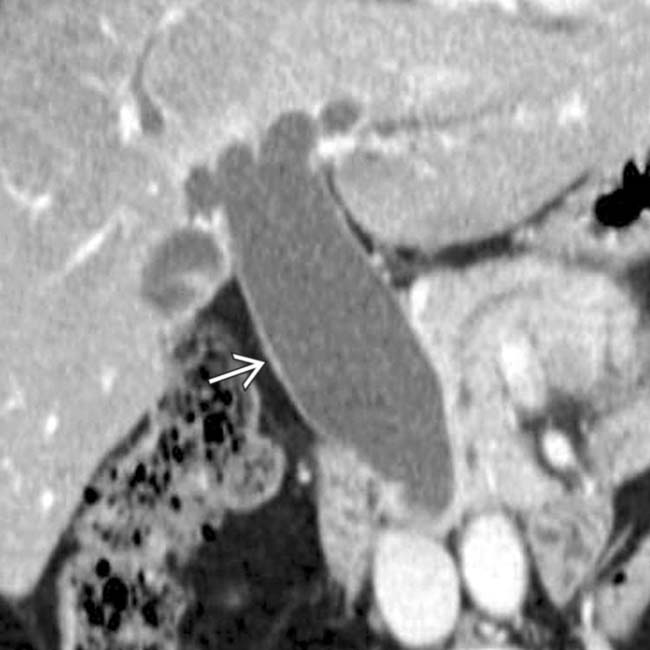
 protruding into the duodenal lumen and mild dilation of the common bile duct
protruding into the duodenal lumen and mild dilation of the common bile duct  . This is either a type III or IVb choledochal cyst, depending on whether the ED is considered to be involved.
. This is either a type III or IVb choledochal cyst, depending on whether the ED is considered to be involved.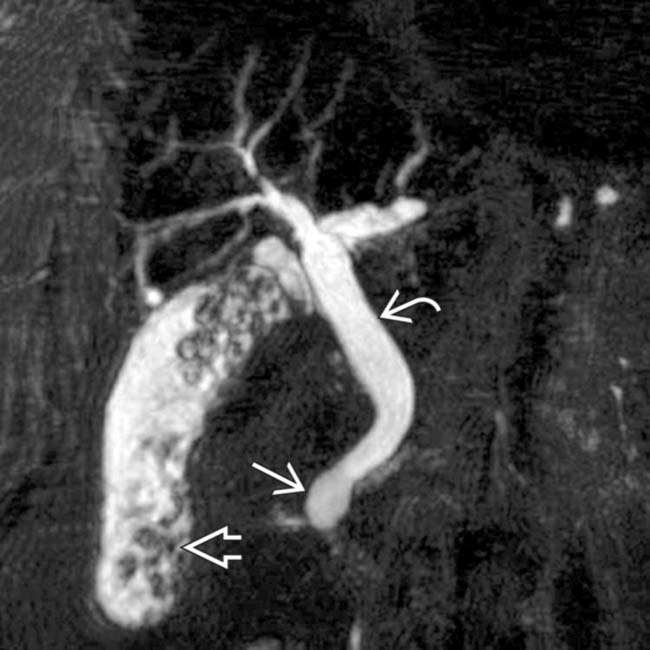
 protruding into the duodenal lumen and the mildly dilated extrahepatic duct
protruding into the duodenal lumen and the mildly dilated extrahepatic duct  , along with numerous stones in the gallbladder
, along with numerous stones in the gallbladder  .
.IMAGING
General Features
• Rare disorder usually diagnosed in infancy and childhood, but is most common congenital lesion of large bile ducts
• Segmental cystic dilatation of bile ducts with dilated segments maintaining communication with biliary tree
 Diagnosis requires excluding other causes of biliary dilatation, including tumor, stone, or stricture
Diagnosis requires excluding other causes of biliary dilatation, including tumor, stone, or stricture
 Commonly associated with cholelithiasis, cystolithiasis (stones within choledochal cyst), choledocholithiasis, and hepatolithiasis
Commonly associated with cholelithiasis, cystolithiasis (stones within choledochal cyst), choledocholithiasis, and hepatolithiasis
 Most commonly classified into 5 different types based on Todani classification
Most commonly classified into 5 different types based on Todani classification
 Diagnosis requires excluding other causes of biliary dilatation, including tumor, stone, or stricture
Diagnosis requires excluding other causes of biliary dilatation, including tumor, stone, or stricture Commonly associated with cholelithiasis, cystolithiasis (stones within choledochal cyst), choledocholithiasis, and hepatolithiasis
Commonly associated with cholelithiasis, cystolithiasis (stones within choledochal cyst), choledocholithiasis, and hepatolithiasis Most commonly classified into 5 different types based on Todani classification
Most commonly classified into 5 different types based on Todani classification – 2003 modification of Todani classification incorporates presence of abnormal pancreaticobiliary junction (APBJ)
– Type I: Solitary fusiform or cystic dilation of extrahepatic bile duct (ED)
 Much more common in females than males (3:1) and may present with pain, jaundice, or gallstone formation (due to bile stasis)
Much more common in females than males (3:1) and may present with pain, jaundice, or gallstone formation (due to bile stasis)
 Differentiate from distal obstruction of ED (e.g., stone or tumor) or mild normal dilatation of ED after cholecystectomy
Differentiate from distal obstruction of ED (e.g., stone or tumor) or mild normal dilatation of ED after cholecystectomy
 Much more common in females than males (3:1) and may present with pain, jaundice, or gallstone formation (due to bile stasis)
Much more common in females than males (3:1) and may present with pain, jaundice, or gallstone formation (due to bile stasis) Differentiate from distal obstruction of ED (e.g., stone or tumor) or mild normal dilatation of ED after cholecystectomy
Differentiate from distal obstruction of ED (e.g., stone or tumor) or mild normal dilatation of ED after cholecystectomy– Type III: Dilation limited to intraduodenal segment of ED (a.k.a. choledochocele), with dilated segment of ED located within duodenal wall
– Type IV: Presence of multiple biliary cysts, at least 1 of which must involve extrahepatic bile duct
 IVa: Involvement of both intrahepatic and extrahepatic ducts; 2nd most common overall, comprising 40% of cases diagnosed in adults
IVa: Involvement of both intrahepatic and extrahepatic ducts; 2nd most common overall, comprising 40% of cases diagnosed in adults
 IVa: Involvement of both intrahepatic and extrahepatic ducts; 2nd most common overall, comprising 40% of cases diagnosed in adults
IVa: Involvement of both intrahepatic and extrahepatic ducts; 2nd most common overall, comprising 40% of cases diagnosed in adultsMR Findings
• Best noninvasive modality for assessing biliary tree, choledochal cysts, and anomalous pancreaticobiliary junction
• MRCP images nicely demonstrate cystic dilatation of biliary tree and relationship (and communication) of cysts with adjacent bile ducts
• Choledochal cysts should mirror signal intensity of normal bile ducts (hypointense on T1WI, hyperintense on T2WI, and no perceptible wall enhancement on T1WI C+)
Ultrasonographic Findings
• Grayscale ultrasound
 Anechoic lesion in porta hepatis (types I, II, or IV) with posterior acoustic enhancement
Anechoic lesion in porta hepatis (types I, II, or IV) with posterior acoustic enhancement




 Anechoic lesion in porta hepatis (types I, II, or IV) with posterior acoustic enhancement
Anechoic lesion in porta hepatis (types I, II, or IV) with posterior acoustic enhancement – Can be confused with gallbladder or mesenteric cyst, unless communication with extrahepatic bile duct is established
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree