First author
Year
N
Follow-up (years)
Local control (%)
Alpert
2005
30
13.8
93
Abner
1993
16
3.25
69
Kurtz
1991
50
4.25
62
Komoike
2003
30
3.6
70
Salvadori
1999
57
6.1
86
Gentilini
2007
161
3.6
79
Dalberg
1998
14
13
50
Ishitobi
2014
130
4.8
81
Voogd
1999
16
4.3
62
Alpert et al. utilized salvage breast-conserving surgery in 30 patients with tumor size <3 cm, ≤3 positive lymph nodes, no skin involvement, and no lymphovascular space invasion. These patients were compared to a cohort of patients with ipsilateral breast cancer recurrence treated with salvage mastectomy. With a median follow-up after salvage surgery of 13.8 years, local control was 93 %. After a second local failure, mastectomy was performed for repeat salvage surgery. There was no difference in distant metastasis, cause-specific survival, or overall survival between the repeat lumpectomy and mastectomy groups. In the cohort who underwent salvage mastectomy for local recurrence, 24 % had multicentric disease on pathologic review. Multicentric disease was identified preoperatively on physical exam or mammography in all patients (Alpert et al. 2005).
Abner et al. reviewed 16 patients who refused mastectomy and received excisional biopsy alone for recurrent breast cancer. The local failure rate was 31 % (Abner et al. 1993). The Milan group performed a review of their repeat lumpectomy patients (n = 57) and salvage mastectomy (n = 134) with a median follow-up of 73 months. In the lumpectomy alone group, local control and 5-year overall survival were 86 and 85 %, respectively, compared to 97 and 70 % in the mastectomy group. No difference was seen with regard to the disease-free survival between patients who underwent mastectomy and those who had repeat excision (Salvadori et al. 1999). A review of 14 patients who received salvage breast-conserving surgery reported a local failure rate of 50 % (Dalberg et al. 1998).
As noted above, local recurrence rates following repeat breast-conserving surgery range from 10 to 50 %, with most reports in the 30–35 % range. Interpretation of these results is limited by the fact that the use of breast imaging and margin status are not uniformly reported. The local control rate of salvage lumpectomy is similar to that seen in prospective trials of newly diagnosed breast cancer patients treated with lumpectomy without adjuvant radiation. The addition of repeat irradiation may lead to a decrease in local failure after salvage lumpectomy similar to that seen at initial treatment.
1.3 Salvage Breast-Conserving Surgery with Breast Re-irradiation
Despite the belief that previous breast or mantle irradiation is considered a contraindication to breast conservation surgery and repeat breast irradiation, several investigators have reported their clinical experience or performed prospective trials. The general treatment approach has utilized partial breast irradiation or accelerated partial breast irradiation. Technological advances in radiotherapy delivery have aided in the delivery of radiation to a portion of the breast over a shorter period of time compared to standard whole breast radiotherapy. In the case of repeat breast radiotherapy, delivering radiation to a portion of the breast has the advantage of limiting the possible toxicity of re-irradiation. Partial breast irradiation can be delivered using conformal external beam radiation therapy, interstitial brachytherapy, intracavitary brachytherapy, electron therapy, or intraoperative orthovoltage therapy (Harms et al. 2016).
Chadha et al. reported the results of a prospective phase I/II trial of partial breast low-dose-rate interstitial brachytherapy after salvage lumpectomy. The median prior external beam dose to the breast was 60 Gy (Chadha et al. 2008). The first six patients received 30 Gy and after a minimum follow-up of 12 months, there was no unacceptable toxicity. For the next nine patients, the repeat radiation dose was increased to 45 Gy to the lumpectomy cavity plus a 1–2 cm margin. The skin dose was limited to ≤20 Gy. At a median follow-up of 36 months, overall survival is 100 %, and local disease-free survival is 89 %. One patient developed a local recurrence at 27 months after re-irradiation, underwent salvage mastectomy, and is without evidence of disease. Three patients developed skin pigmentation at catheter entry/exit sites with no grade 3 or 4 fibrosis. No infection was noted. No adverse cosmetic outcomes were noted on serial follow-up examinations with the exception of breast asymmetry present prior to re-irradiation.
The Allegheny group published their results of 26 patients treated with salvage breast-conserving surgery followed by repeat breast irradiation with brachytherapy with a median follow-up of 38 months from re-irradiation (Trombetta et al. 2009). The previous radiotherapy was 45–60.4 Gy, with one patient treated with mantle irradiation and the remainder treated for breast cancer. A total of 22 patients were treated with interstitial low-dose-rate brachytherapy to the tumor bed plus 1 cm margin to 45–50 Gy. Four patients were treated with intracavitary balloon brachytherapy to 34 Gy in ten fractions given twice daily. Local control was 96 %. Cosmetic outcome was graded according to the National Surgical Adjuvant Breast and Bowel Project cosmesis scale. Two patients had grade III cosmesis, and no grade IV cosmesis was seen. In a separate study, this same group treated 18 patients with balloon-based brachytherapy to 34 Gy in 3.4 Gy fractions twice daily. At a median follow-up of 39.6 months, 11 % experienced a local failure treated with salvage mastectomy. One patient developed a chronic infection in the balloon tract which required a mastectomy (Trombetta et al. 2014).
In a prospective trial from Vienna University, 17 patients with small (0.5–2.5 cm) breast recurrences underwent a second breast-conserving surgery and breast re-irradiation (Resch et al. 2002). The prior dose to the breast was 50–60 Gy. In the pilot phase of the trial, eight patients were treated. They received 30 Gy external beam radiotherapy and a 12.5 Gy pulsed-dose-rate brachytherapy to the tumor bed plus 2 cm margin. The next seven patients were treated with decreasing the external beam dose while increasing the dose delivered via brachytherapy. The final nine patients received 40.2–50 Gy pulsed-dose-rate brachytherapy alone. After a median follow-up of 59 months, 24 % (four patients) developed a second local recurrence. A total of 12 patients were alive and free of local tumor, with bone metastasis in two patients. Toxicity was limited to grade 1–2 fibrosis. There were no issues with wound healing. No patients developed unacceptable cosmesis. As a follow-up to this pilot, the authors conducted a prospective protocol of repeat radiotherapy after breast-conserving therapy using multi-catheter accelerated PDR brachytherapy to 50.1 Gy to the tumor bed plus 2 cm (Kauer-Dorner et al. 2012). The EQD2 to the late-responding tissue was calculated to be 63.4 Gy for the PDR brachytherapy. The prior whole breast radiotherapy dose was 50 Gy with a boost given to 28 %. At 57 months mean follow-up, local control was 93 % with late grade ≥3 side effects in 16 % in the 24 women with detailed data on late side effects. Seventy-six percent had excellent to fair cosmesis.
Investigators from two institutions in France reported the largest series of breast re-irradiation with interstitial LDR brachytherapy in 69 patients who declined salvage mastectomy (Hannoun-Levi et al. 2004). The mean dose to the breast at diagnosis was 60.5 Gy. After second lumpectomy, repeat irradiation was delivered to the tumor bed plus 2 cm to a dose of 50 and 30 Gy in Marseilles and Nice, respectively. A cumulative dose (first-course dose plus second-course dose) greater than 100 Gy was administered to the breast in 62 patients. The median follow-up was 50.2 months. Freedom from a second local recurrence at 5 years was 77.4 %, and freedom from metastasis after local recurrence at 5 years was 86.7 %. Grade 2 (toxicity requiring medical treatment) and grade 3 (toxicity requiring surgical intervention) late complications were experienced by 11.6 and 10.2 % of the study patients, respectively. When the cumulative radiotherapy dose was greater than 100 Gy, the rate of grade 2 or 3 complications was higher (4 % versus 32.5 %, p = 0.005). When the re-irradiation dose was greater than 46 Gy, the rate of grade 2 or 3 toxicity was 36 % compared to 13.6 % when the re-irradiation dose was less than 46 Gy (p = 0.007).
A series of 42 patients who underwent a second lumpectomy followed by interstitial HDR brachytherapy was performed by the investigators in Nice (Hannoun-Levi et al. 2011). A dose of 34 Gy in 10 fractions over 5 consecutive days was prescribed to the tumor bed plus 1 cm. Median follow-up was 21 months. Local control was 97 % and late toxicities were grade 1, 28 %; grade 2, 19 %; and grade 3, 3 %. Most toxicities were cutaneous and subcutaneous fibrosis. However, pain, telangiectasias, and rib fractures were observed in 28, 21, and 2 %.
A multi-institutional retrospective review of 217 patients who received a second lumpectomy and repeat radiotherapy using interstitial partial breast brachytherapy was performed from eight European radiation oncology departments (Hannoun-Levi et al. 2013). Five- and 10-year local failure rates were 5.6 and 7.2 %, respectively. Five- and 10-year metastasis rates were 9.6 and 19.1 %, respectively. Grades 3–4 late toxicity rate was 11 %.
Limited data is available on intraoperative radiotherapy for repeat breast radiotherapy. The first publication included 15 patients treated with a single dose of 14.7–20 Gy 50 kV X-rays to the applicator surface with Intrabeam (Kraus-Tiefenbacher et al. 2007). Local control was 100 % at a median follow-up of 26 months and no late grade 3 or 4 toxicities were seen.
Most reports of repeat partial breast irradiation have utilized interstitial brachytherapy as opposed to external beam radiation therapy (Table 2). Deutsch published a review of 39 patients with recurrent breast cancer (n = 38) or ductal carcinoma in situ (n = 8) who underwent repeat breast-conserving surgery and external beam re-irradiation (Deutsch 2002). All patients received prior whole breast radiation to 45–50 Gy followed by a boost to the tumor bed (unreported dose) in 21 patients. Margins were positive in 13 % after salvage lumpectomy. Repeat irradiation was performed using electrons to the tumor bed to 50 Gy in 25 fractions. Local control was 79 %, with the second local recurrence developing in the same quadrant in three of the eight local failures. Nine patients had a fair to poor cosmetic result.
Table 2
Results of salvage breast-conserving surgery and partial breast re-irradiation
First author | Year | N | Technique | Prior RT dose (Gy) | Re-RT dose (Gy) | Local control (%) |
|---|---|---|---|---|---|---|
Chadha | 2008 | 15 | LDR PBI | 60 | 30–45 | 89 |
Hannoun-Levi | 2004 | 69 | LDR PBI | 60.5 | 30–50 | 77 |
Maulard | 1995 | 38 | LDR PBI | 65 | 30–70 | 79 |
Resch | 2002 | 17 | Mixed | 50–60 | 40–50 | 76 |
Trombetta | 2009 | 26 | LDR/HDR PBI | 45–60.4 | 45–50 LDR; 34 HDR | 96 |
Trombetta | 2014 | 18 | HDR PBI | NR | 34 | 89 |
Guix | 2010 | 36 | HDR | NR | 30 | 89 |
Hannoun-Levi | 2011 | 42 | HDR | 45–66 | 34 | 97 |
Kauer-Dorner | 2012 | 39 | PDR | 50–61.8 | 50.1 | 93 |
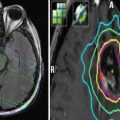
The NRG Oncology/Radiation Therapy Oncology Group has completed a prospective phase II trial evaluating salvage lumpectomy and re-irradiation using three-dimensional conformal radiation therapy. Eligible patients must meet the following criteria: recurrent tumors ≤3 cm, no evidence of multicentric disease on MRI and breast imaging, no distant metastasis, no skin involvement, ≤3 positive axillary nodes. Previous lumpectomy and adjuvant breast radiotherapy must be completed at least 1 year prior to enrollment. The treatment technique generally uses three, four, or five non-coplanar beam arrangements to meet dose constraints (Table 3) (Baglan et al. 2003; Formenti et al. 2004; Kozak et al. 2006a&b). The target volumes are defined as follows:
Table 3
Normal tissue constraints for repeat partial breast irradiation according to RTOG 1014
Normal tissue | Constraint |
|---|---|
Uninvolved normal breast | <60 % of whole breast receives ≥50 % of prescription dose and <35 % of whole breast receives prescribed dose |
Contralateral breast | <3 % receives prescription dose |
Ipsilateral lung | <15 % receives 30 % of prescription dose |
Contralateral lung | <15 % receives 5 % of prescription dose |
Heart (right-sided recurrence) | <5 % receives 5 % of prescription dose |
Heart (left-sided recurrence) | Volume of receiving 5 % of prescription dose <40 % |
Thyroid | Maximum point dose of 3 % of prescription dose |
Clinical target volume (CTV) is defined as the tumor bed with uniform expansion of 15 mm. The CTV is limited to 5 mm from skin surface and excludes the posterior chest wall structures.
Planning target volume (PTV) is defined as the CTV with a uniform 10 mm expansion. The PTV is used to define the appropriate block margin.
PTV_EVAL is defined as the PTV excluding portion of PTV that extend outside the breast and first 5 mm of tissue beneath the skin and posterior extent of the breast. PTV_EVAL is used for dose volume histogram analysis.
A hyperfractionated regimen of 45 Gy in 1.5 Gy twice-daily fractions is prescribed to the PTV. Study endpoints include toxicity outcomes, cosmesis, local control and freedom from mastectomy rate, disease-free survival, and overall survival. For the first 55 patients at 1-year follow-up, skin, fibrosis, and/or breast pain adverse events were grade 1 in 63 %, grade 2 in 7 %, and grade ≥3 in <2 % (Arthur et al. 2015). Recurrence endpoints have not been published and longer follow-up is needed.
1.4 Chest Wall Re-irradiation Alone
An early publication on chest wall re-irradiation from the University of Washington suggested that repeat radiotherapy was feasible (Laramore et al. 1978). A total of 13 patients were re-irradiated after postmastectomy radiotherapy was given at diagnosis, after a mean disease-free interval of 5.9 years. The initial radiation therapy dose to the chest wall was 40–50 Gy, with the details of prior radiation unknown in four patients. The dose of the chest wall re-irradiation was 36–60 Gy in 2 Gy fractions. Cumulative radiotherapy doses were 80–100 Gy. At a mean follow-up of 20 months, the local disease-free survival was 62 %. Acute toxicity appeared tolerable with one patient requiring a treatment break due to moist desquamation. Late toxicity was not reported.
A total of 13 patients from Memorial Sloan-Kettering Cancer Center received chest wall repeat radiation therapy (Wagman et al. 2002). At initial diagnosis, 12 patients underwent lumpectomy and adjuvant breast radiotherapy to 45–50.4 Gy followed by a tumor bed boost of 6–20 Gy. One patient received preoperative radiotherapy 22 Gy in four fractions followed by mastectomy. The median disease-free interval was 46 months to first recurrence, when three patients had repeat radiotherapy. Ten patients had re-irradiation at second local recurrence. Treatment was given with conformal electron fields to a dose of 7.5–64.4 Gy (median 50.4 Gy). The median follow-up from re-irradiation was 20 months. The 2-year local recurrence-free survival was 85 % and 2-year overall survival was 85 %. Grade 3 skin toxicity was noted in 46 %, with 38 % requiring a treatment break. Late toxicities include a rib fracture and pericarditis.
1.5 Chest Wall Re-irradiation with Hyperthermia or Chemotherapy
Response rates and local disease-free survival rates vary widely after repeat radiotherapy, with complete response rate of 20–70 % (Table 4). Adding concurrent chemotherapy and/or hyperthermia may improve response rates (Datta et al. 2016). A randomized trial of radiation therapy with or without concurrent hyperthermia in superficial tumors demonstrated an improved complete response rate in the hyperthermia arm (Jones et al. 2005). Approximately, 60 % of patients enrolled in that trial had a breast cancer diagnosis. A superior complete response rate from radiotherapy and hyperthermia was seen in previously irradiated patients compared to previously unirradiated patients (68 % versus 24 %, respectively). A meta-analysis of five randomized trials of radiation therapy and hyperthermia revealed that previously irradiated patients who had concurrent hyperthermia and re-irradiation had a statistically significant improvement in complete response rate compared to re-irradiation alone, 57 % versus 31 %, respectively (OR 4.7, 95 % CI 2.4–5.9) (Vernon et al. 1996). A multi-institutional retrospective review of chest wall re-irradiation demonstrated a trend toward improved response rate with the addition of hyperthermia; however, it was not significant (67 % versus 39 %, p = 0.08) (Wahl et al. 2008). Despite the poor prognosis of chest wall recurrences, a complete response to therapy enhances the quality of life and hyperthermia appears to improve response rates.
Table 4
Results of chest wall re-irradiation
First author | Year | N | F/U (mo) | RT 1 (Gy) | RT 2 (Gy) | Cumulative dose (Gy) | HT | CR (%) | LC (%) |
|---|---|---|---|---|---|---|---|---|---|
Laramore | 1978 | 13 | 20 | 40–50 | 36–60 | 80–100 | No | 62 | 62 |
Wagman | 2002 | 13 | 20 | 60.8 | 50.4 | 111.2 | No | – | 85 |
Jones | 2005 | 39 | – | – | 30–66 | – | Yes | 68 | – |
van der Zee | 1999 | 13 | 21 | 45
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|