Study
N
Study dates
Retreatment radiotherapy
Median follow-up (mo.)
5-year local control rate (%)
5-year overall survival rate (%)
Serious complications rate (%)
Amputation rate (%)
Nori et al. (1991)
40
1979–1988
BT
36
68
55–85
13
0
Essner et al. (1991)
21
1972–1988
EBRT
36
48
52
42
28
Graham et al. (1992)
5
1981–1987
EBRT
NR
50
40
>10
20
Catton et al. (1996)
10
1990–1995
BT and/or EBRT
31
100
NR
60
10
Pearlstone et al. (1999)
26
1990–1997
BT
16
52
52
15
0
Moureau-Zabotto et al. (2004)
16
1980–1994
BT or EBRT
59
37
NR
NR
NR
Torres et al. (2007)
37
1991–2004
BT or EBRT
72
58
66a
51
35
Indelicato et al. (2009)
5
1997–2004
BT and EBRT
3
40
0
80
80
Tinkle et al. (2015)
15
2000–2011
IORT
NR
55
NR
33
NR
Cambeiro et al. (2015)
10
1986–1999
IORT
NR
74
37
10
10
Cambeiro et al. (2015)
16
2001–2010
BT
NR
38
68
56
NR
A common concern regarding the administration of repeat external-beam irradiation for recurrent sarcomas is the fear of severe soft tissue necrosis and fibrosis. In the UCLA series described above, there were 3 serious complications in the 7 patients treated with preoperative reirradiation. Two of the 3 complications required reoperation, including 1 amputation as a result of the complication. In the 14 patients receiving postoperative reirradiation, there were 7 serious complications. Six of these required reoperation, including 1 amputation. Functional analysis was performed on all patients. The most common complication was edema requiring a support stocking, occurring in 29 % of the preoperative patients and 64 % of the postoperative group. No fractures of adjacent long bones or pain occurred in the preoperative reirradiation group, while 7 % and 14 % in the postoperative reirradiation group experienced fracture or pain, respectively. Twenty-nine percent and 36 % required the use of external support (canes or braces) in the preoperative group and postoperative group, respectively. No instance of neuritis or compartment syndrome was observed despite the high cumulative radiation doses. Normal range of motion, defined as being 95 % of the uninvolved extremity, was present in 86 % of the preoperative patients and 36 % of the postoperative patients. The investigators from UCLA concluded that limb salvage was possible in the setting of an isolated local recurrence provided that external-beam radiation was delivered preoperatively in the manner described. For reasons of inferior local control and toxicity, they recommended against postoperative radiation.
In an attempt to further improve salvage therapy for local recurrences, some investigators have used brachytherapy for reirradiation. The largest series is from Memorial Sloan-Kettering Cancer Center (MSKCC; New York, NY) and includes 40 patients with recurrent extremity sarcoma treated from 1979 to 1988 (Nori et al. 1991). Seventy percent of patients had recurrent thigh lesions, and most had received external-beam irradiation as their initial treatment. For salvage, patients underwent conservative function-preserving surgery with brachytherapy alone via a temporary afterloaded iridium-192 (Ir-192) tumor bed implant. A median dose of 4500 cGy was delivered (range, 3000–4800 cGy) at a median dose rate of 40 cGy/h. The median follow-up was 3 years, which was sufficient to capture most local recurrences (Lindberg et al. 1981; Singer et al. 1992) and complications. The 5-year overall survival rate was 85 % and the 5-year local control rate was 68 %. The most important factor impacting the likelihood of local control following salvage was the number of prior local recurrences.
Another large experience involving salvage brachytherapy alone for sarcoma in a previously irradiated field was published in 1999 by Pearlstone et al. from MD Anderson Cancer Center (Houston, TX) (Pearlstone et al. 1999). This study included 26 patients with recurrent sarcoma treated from 1990 to 1997 with a diverse range of tumor sites including the extremities (55 %) as well as the trunk (27 %) and head-and-neck region (8 %). Sixty-five percent of patients had received external-beam irradiation as part of their initial treatment and the rest had received primary brachytherapy. For salvage, patients underwent conservative function-preserving surgery followed by brachytherapy alone via a single-plane afterloaded Ir-192 tumor bed implant. A mean dose of 4720 cGy was delivered (range, 1100–5000 cGy) at a median dose rate of 40 cGy/h. The median follow-up was 16 months. Five-year overall survival was 52 %, and 5-year local control was 52 %. As with the MSKCC experience, the most important factor impacting the likelihood of local control following salvage was the number of prior local recurrences. When patients with tumors located near joint spaces (notoriously difficult areas for brachytherapy) are excluded from the analysis, the local control rate was 82 %.
Brachytherapy alone for salvage offers several theoretical and practical advantages over external-beam reirradiation. By approaching the process of radiation as part of a team of physicians, the areas of highest risk can be directly identified and targeted in the operating room. Interstitial Ir-192 brachytherapy can be delivered in only a few days and commences approximately 1 week following surgery. This treatment option is in contrast to external-beam radiotherapy that typically lasts 6–7 weeks and cannot begin until at least 3–4 weeks following surgery or perhaps longer in tissue that has impaired wound healing from previous radiation. This prolonged postoperative period not only increases the social and economic burden of treatment but may delay the start of adjuvant chemotherapy if indicated. From a radiation delivery perspective, the rapid dose falloff of brachytherapy is such that very little previously irradiated normal tissue outside the target volume receives radiation. The MSKCC brachytherapy reirradiation series (Nori et al. 1991) reported five patients (12.5 %) who experienced serious complications (four patients had soft tissue necrosis and one had a long bone fracture). All patients recovered completely without amputation, functional loss, or disability. The group at MDACC reported a similar low rate of complications (15 %) and no amputations (Pearlstone et al. 1999). All of the patients who experienced a perioperative complication underwent primary wound closure, and none of the patients who were reconstructed using a nonirradiated tissue flap experienced a perioperative complication. With a median follow-up of 16 months, however, events in this study may be underreported. In contrast to these series, a study from the Claudius Regaud Institute (Toulouse, France) with a median follow-up of 59 months reported significantly higher rates of late complications after reirradiation with brachytherapy (Moureau-Zabotto et al. 2004). Moureau-Zabotto et al. reported that 49 % of patients developed one or more chronic grade 3 or 4 complications after salvage surgery and reirradiation.
A series from The University of Navarre (Pamplona, Spain) included 16 patients with locally recurrent STS treated for salvage with limited resection followed by brachytherapy beginning within 9 days of surgery (Cambeiro et al. 2015). Brachytherapy consisted of a single-plane catheter array covering the tumor bed plus a margin in 8–10 twice-daily treatments to a dose of 32 or 40 Gy for R0 and R1 resections, respectively. With a median follow-up in excess of 3 years, 5-year local-regional control, distant control, and overall survival rates were 38 %, 44 %, and 68 %, respectively. Similar to the French series, these investigators reported high rates of treatment-related complications, with 56 % of patients experiencing grade 3–4 complications, 50 % of whom required reoperation. All acute and late complications were related to soft tissue injury (including wound dehiscence, infection/abscess, graft failure, necrosis).
Not surprisingly, there are striking differences between the disease control and toxicity outcomes among these retrospective single-institution reports using brachytherapy for reirradiation, which are likely related to differences in patient selection and treatment technique. Notably, the series from MSKCC and MDACC favored smaller and more accessible tumors for which one might expect better tumor control (Pearlstone et al. 1999; Zagars et al. 2003) and fewer complications. For example, the MSKCC series was limited to extremity tumors. Additionally, although recurrent sarcoma may be inherently aggressive from a biological standpoint, some reports indicate that brachytherapy is less effective for low-grade sarcomas, at least in the primary setting (Pisters et al. 1996).
Due to previous surgery and radiation, recurrent STS develop among disturbed tissue where fascial planes are obscured by fibrosis and lymphovascular drainage patterns are distorted. Disease may unpredictably extend well beyond the normal margins. In addition to physiologic remodeling, the anatomy itself is altered and challenges the geometry of brachytherapy implants (Torres et al. 2007). Supplementary external-beam radiotherapy has been utilized by some practitioners to essentially extend and compensate for the irregular dose distribution of brachytherapy.
The largest series describing outcomes following this approach of brachytherapy plus external-beam irradiation comes from the University of Florida. From 1976 to 2005, five patients who underwent primary conservative resection and irradiation developed an isolated local recurrence and were managed with preoperative external-beam radiation and then wide local excision followed by a brachytherapy boost. The external-beam radiation was 24 Gy delivered in a hyperfractionated manner at 1.2 Gy twice daily to minimize the late tissue effects. For the brachytherapy, eight to ten catheters were used, and the dose rate was 50–60 cGy/h prescribed to 5–10 mm from the single implant plane. The median interval between surgery and Ir-192 afterloading was 5 days. The median brachytherapy dose was 39 Gy (range, 26–42 Gy). The median total dose for retreatment was 63.5 Gy (range, 51.5–66.0 Gy). With a median follow-up of 3 years, the results were dismal. All five patients eventually died from their disease. This aggressive retreatment approach led to severe complications in four of five patients (all of which were chronic non-healing ulcers or other wound complications requiring amputation). Despite aggressive management, three patients ultimately developed another local recurrence before death.
Following a rationale similar to brachytherapy, several investigators have reported success using intraoperative electron-beam radiation therapy (IOERT) for reirradiation of STS (Azinovic et al. 2003; Cambeiro et al. 2015; Tinkle et al. 2015). IOERT applicators are desirable because they can directly visualize and access the surgical bed in the operating room and the dosimetry of the electrons may be easily customized. This strategy may decrease toxicity since dose-limiting normal tissues can be displaced or protected during IOERT (Willett et al. 2007). Like brachytherapy, IOERT might indirectly improve the quality of therapy by decreasing the overall treatment time. In the experience from the University of Navarre, ten patients with locally recurrent extremity STS or aggressive fibromatosis were treated with IOERT from 1986 to 1999 following limb-sparing surgery. The radiation therapy details of initial patient treatments were not available. For the IOERT course of reirradiation, electron energies between 6 and 15 MeV were utilized depending on the clinical scenario and the extent of residual disease. The IOERT reirradiation dose was between 10 and 20 Gy depending on the margin status. The 5-year actuarial local control, distant control, and overall survival rates were 58 %, 76 %, and 37 %, respectively. One severe toxicity (≥grade 3) occurred involving graft failure requiring amputation (Cambeiro et al. 2015).
A recent series from University of California, San Francisco, also utilized intraoperative radiotherapy for salvage of locally recurrent STS. Tinkle et al. (2015) described 26 patients with locally recurrent STS of the extremities treated with limited resection and IOERT. Of the 26 patients, 15 had previously received external-beam radiotherapy (EBRT; median dose, 63 Gy; range, 25–72 Gy) as part of their initial treatment course. The remaining 11 patients, who had received no prior radiotherapy, were treated with adjuvant EBRT (median dose, 52 Gy; range, 22–60 Gy) following limited resection and IOERT. Surgery consisted of limb-sparing surgery achieving a gross total resection and IOERT to 10–18 Gy (median dose, 15 Gy). With a median follow-up of 35 months, there was no major difference in 5-year actuarial local control in the reirradiation cohort compared to those with no prior radiotherapy, 55 % and 61 % (p > 0.05), respectively. In the reirradiation group, 20 % experienced ≥grade 3 acute toxicity, and 33 % experienced ≥grade 3 late toxicity, consisting of wound complications and limb/joint dysfunction.
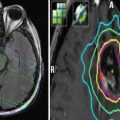
3 Reirradiation Technique
As described above, there are limited published outcomes following reirradiation for STS, and most include few patients using varied patient selection methods. The information below represents guidelines based on the best available evidence and expert opinion. For all reirradiation cases, patients may benefit from referral to a high-volume center.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree