(1)
Radiology Department Beijing You’an Hospital, Capital Medical University, Beijing, People’s Republic of China
Abstract
Critical medicine is a newly emerging branch of modern medicine and is an important symbol of medical progress. In China, critical medicine started late. However since 1980s, with the advance in medicine, more and more hospitals have been establishing comprehensive or specialized intensive care unit (ICU). More and more professional ICU staffs have been improving their diagnostic and therapeutic ability through education and practice.
Keywords
HIV/AIDS Related Critical and Severe Opportunistic InfectionsHIV/AIDS Related Advanced CancerHIV/AIDS Related Multiple Organ FailureHIV/AIDS Related Intensive Care11.1 Overview
Critical medicine is a newly emerging branch of modern medicine and is an important symbol of medical progress. In China, critical medicine started late. However since 1980s, with the advance in medicine, more and more hospitals have been establishing comprehensive or specialized intensive care unit (ICU). More and more professional ICU staffs have been improving their diagnostic and therapeutic ability through education and practice.
In China, patients with communicable diseases are required to be treated in local hospitals specialized in infectious diseases. In these specialized hospitals, establishment and development of ICU are later than those in the comprehensive hospitals. Due to the lack of specialized staffs in respiratory, renal, hematological and cardiovascular fields and the lack of common facilities such as breathing machine, bedside hemofiltration, hemodynamic monitoring, it is difficult for specialized hospitals to launch critical medicine. Nevertheless, with the development of modern medicine and the growing demand for health care, specialized hospitals in infectious diseases need to provide services in critical medicine, which should be supported by related research. Undoubtedly, patients with AIDS are the most important and special group demanding intensive care services in specialized hospitals of infectious diseases.
AIDS was firstly found in patients with pneumocystis pneumonia and Kaposi’s sarcoma. Both are still AIDS-related diseases threatening the life of patients. In addition, many other opportunistic infections and malignant tumors caused by AIDS are also being life-threatening. In the past 50 years, with the development of antiviral therapy, HIV infection has changed from a deadly infectious disease to a controllable chronic disease. More and more patients with HIV/AIDS are able to work and live as healthy population and the progression of the disease is increasingly slowed. Moreover, with the development of intensive care techniques, the survival rate of patients in ICU is notably increased. However, with prolonged life expectancy, life-threatening causes of advanced AIDS are becoming increasingly complex. In this chapter, assessment and monitor of critical illnesses threatening the life of patients with AIDS are described and discussed.
11.2 HIV/AIDS Related Critical and Severe Opportunistic Infections
Most HIV-infected patients are unaware of their infection until the infection progresses into the stage of AIDS. Commonly, most patients are diagnosed as having HIV infection after the occurrence of opportunistic infections. Some patients are even diagnosed when they sustain a life-threatening condition caused by critical opportunistic infections. When AIDS was initially acknowledged, the death rate in patients with AIDS receiving intensive care was up to 90 % due to their severely compromised immunity. But recently, the death rate in patients with AIDS receiving intensive care has dropped to less than 50 %. In China, opportunistic infections have always been the main cause of death in HIV-infected patients, and clinicians treating patients with HIV/AIDS need more knowledge about the related critical and severe opportunistic infections.
The CD4 T cell count in HIV infected patients is closely related to the types of opportunistic infections as well as the location and involved range of neoplasms. When CD4 T cell count is above 500/μl, patients are susceptible to acquired pneumonia and have more frequent occurrence o tuberculosis than non-HIV-infected subjects, but with basically the same diseases spectrum as the non-infected group. When CD4 T cell count is below 500/μl, opportunistic infections may occur and recur, including esophageal candidiasis, herpes simplex virus infection, and zoster virus infections. In addition, they also have a higher incidence of pneumococcal infection than populations with normal immunity. When CD4 T cell count is below 200/μl, the incidence of pneumocystis pneumonia (PCP) increases significantly. When CD4 T cell count is below 50/μl, disseminated infections tend to occur, such as cytomegalovirus infection and cryptococcus infection. In addition, such patients have a higher occurrence of central nervous system infections.
Pneumocystis pneumonia (PCP) is the most common opportunistic infection and is the main cause of death during early days HIV epidemic. In the year of 1988, the pathogen was proved to be fungus and later specified to be pneumocystis carinii (PC) [1]. Most HIV-infected patients are not aware of their infection until the onset of symptoms. Their symptoms like fever and cough are commonly misdiagnosed as common respiratory infection and are treated with common anti-infection therapies that are ineffective for PCP. Consequently, many patients are only accurately diagnosed after the occurrence of tachypnea or even respiratory failure. Therefore, most patients with PCP receive oxygen therapy or even mechanical ventilation. Nowadays, PCP is still the main cause of death in HIV-infected patients for its high case fatality rate.
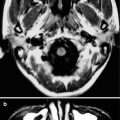
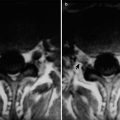
Since toxoplasma gondii has an affinity to the central nervous system, toxoplasmic encephalitis is a life threatening opportunistic infection. Even after timely appropriate treatment, sequelae occur, including focal neurological deficits, hemiplegia and epilepsy. The severity of toxoplasmic encephalitis is related to the location of lesions. It is characterized by acute onset and rapid progress. Without timely appropriate therapies, it is life-threatening.
Despite of slow progression of tuberculosis, its case fatality rate is significant, as its occurrence in HIV-infected patients. The occurrence of tuberculosis in HIV-positive population is 8 times higher than that in HIV-negative populations. Meanwhile, HIV infection accelerates multi-drug resistance to tuberculosis, leading to increased difficulties in treating tuberculosis. Tuberculosis rarely causes death in patients but aggravates existing illnesses and accelerates the decline of immunity to cause their susceptibility to other opportunistic infections. Therefore, it is necessary to administer drug sensitivity monitoring for patients with AIDS complicated by tuberculosis.
Atypical mycobacteriosis is one of the main reasons for the symptoms of fever, diarrhea and weight loss in HIV-infected patients. Without timely appropriate treatment, it could cause deterioration of the clinical conditions.
Progressive multifocal leukoencephalopathy (PML) is a serious demyelinating disease of the central nervous system. It is caused by JC virus, a polyoma virus, which is the second most common opportunistic infection of the nervous system in patients with AIDS, following toxoplasmosis. Its clinical symptoms include cognitive impairment and focal neuropathy and hemiplegia, language disorder or visual disorders are the most common. Clinically, there is no specific therapy against it.
Bacterial pneumonia occurs in any stage of HIV/AIDS, whose occurrence is not obviously related to the decrease of CD4 T cell count. However, the promotion of ART treatment does not significantly reduce its incidence and its treatment is similar to those for non-HIV-infected patients.
Cryptosporidiosis is an intestinal parasitosis with a spreading route of faecal-oral transmission. Death may occur in such patients with severely compromised immunity due to fluid and electrolytes loss caused by long-term diarrhea.
Cryptococcus neoformans infection is commonly transmitted by bird faeces, commonly involving lungs and central nervous system. Without timely definitive diagnosis and appropriate treatment, it may invade the central nervous system, followed by a rapid progression. Such patients may have fever, headache and conscious disturbance, cranial nerve palsy, severe headache caused by increased intracranial pressure. Its definitive diagnosis depends on microscopic examination after India ink staining of cerebrospinal fluid (CSF) obtained by lumbar puncture.
11.3 HIV/AIDS Related Advanced Cancer
The most common HIV/AIDS related tumors are Kaposi’s sarcoma (KS) and lymphoma. KS is related to human herpes virus 8 (HHV-8), spreading by sexual contacts, blood and saliva and is an indicator of AIDS. The patients in advanced stage of AIDS with no history of therapies usually have a rapid progression of KS, with an average survival period of less than 1 year. Even death may occur within several weeks in cases of rapid progression. Unlike cases of non-HIV-infected patients, KS in HIV-infected patients occurs at varying locations, including skin, oral cavity, alimentary canal, genital organ and ocular region. And the lesions range from painless skin lesion to invasive and disseminated lesions with lymph nodes and internal organs involved.
KS is conventionally diagnosed based on the following clinical findings on the skin or mucous membranes:
1.
Purple plaques or nodules;
2.
Lesions distributing along dermal texture;
3.
Yellowish green skin surrounding the lesion of tumor hemorrhage;
4.
Peripheral edema;
5.
Disseminated lesions, with possible involvement of skin mucosa.
Definitive diagnosis can be made based on biopsy of the focal tissues. KS can be self alleviated or alleviated after treatment. But due to hemosiderin deposition caused by erythrocyte exudation, brown or light brown pigmentation may present for several months or several years. For the cases of initial KS diagnosis, following examinations should be regularly performed for monitoring, the clinical staging and corresponding treatments:
1.
General examination of skin mucosa;
2.
Ultrasonography of lymph nodes;
3.
Abdominal ultrasonography;
4.
Upper gastrointestinal endoscopy;
5.
Lower gastrointestinal endoscopy;
6.
Chest X-ray;
7.
CT scanning.
Simultaneously, CD4 T cell count and HIV virus load should be monitored for decisions about administration of antiviral therapy. Both indicators are valuable in predicting the prognosis.
Compared to healthy subjects, HIV-infected patients are more susceptible to lymphomas, among which invasive B cell Non-Hodgkin’s lymphoma (B-NHL) is the most dangerous. Currently, lymphoma has a higher incidence than KS, ranked the first in occurrence of HIV/AIDS related malignancies. Its symptoms include lymphadenectasis and immobile hardened painless masses. The patients may sustain fever, night sweating and/or weight loss. General upset and physical deterioration are also common.
Since chemotherapy is the most commonly used therapy, electrocardiography (ECG) and ultrasonic cardiography (UCG) should be regularly performed to assess the cardiac toxicity caused by chemotherapy. In addition, pulmonary function should be examined before and during therapies containing medication of bleomycin. During chemotherapy, assessment should be performed every other therapeutic course for clinical staging and efficacy evaluation. After the chemotherapies are finished, bone marrow biopsy and CT scanning should be performed for a general clinical staging. For cases of complete remission, follow-up clinical staging should be performed every 3 months during the first year, every 6 months after 1 year and every 12 months after 2 years. During the follow-up period, cerebrospinal fluid test should be ordered regularly to exclude meningeal involvement.
11.4 HIV/AIDS Related Multiple Organ Failure (MOF)
One organ could be involved due to opportunistic infection in HIV-infected patients, which could lead to multiple organ failure (MOF) if such patients cannot receive timely appropriate treatment. Meanwhile, due to compromised immunity, multiple organs infections may occur simultaneously, leading to multiple organs impairments. In conclusion, multiple organs impairments in patients with HIV/AIDS can occur and gradually progress to MOF because of the involvement of one organ or concurrent involvement of multiple organs.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree