Solitary or multifocal strictures of variable length
• Cholangiography: Gold standard for diagnosis
 Appearance may be identical to PSC with “beading” of biliary tree (alternating stenosis, normal ducts, and mild dilatation)
Appearance may be identical to PSC with “beading” of biliary tree (alternating stenosis, normal ducts, and mild dilatation)
 Appearance may be identical to PSC with “beading” of biliary tree (alternating stenosis, normal ducts, and mild dilatation)
Appearance may be identical to PSC with “beading” of biliary tree (alternating stenosis, normal ducts, and mild dilatation)• MR: Linear high T1 signal intensity may be visualized within dilated central ducts, characteristic of biliary cast
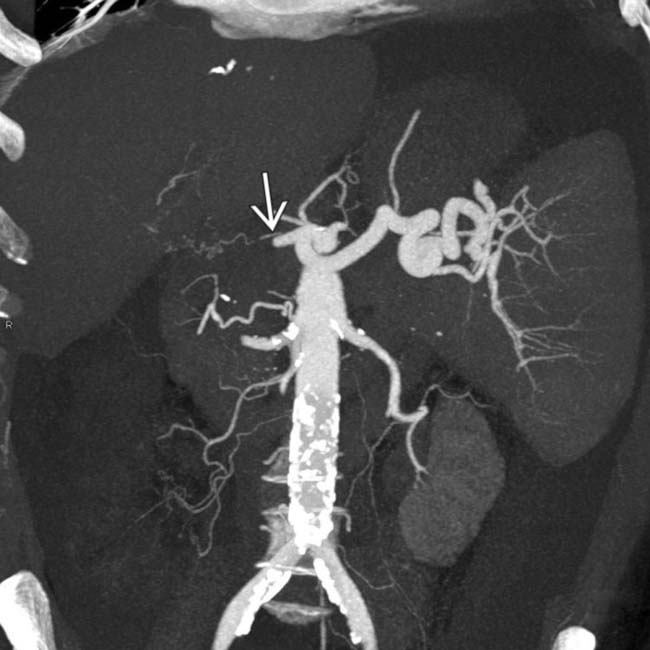
 near its origin from the celiac artery.
near its origin from the celiac artery.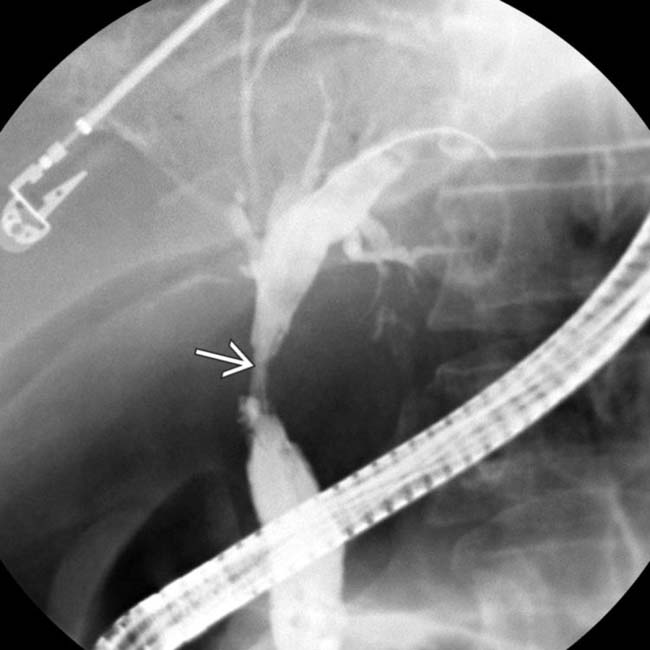
 and irregularity of the intrahepatic ducts.
and irregularity of the intrahepatic ducts.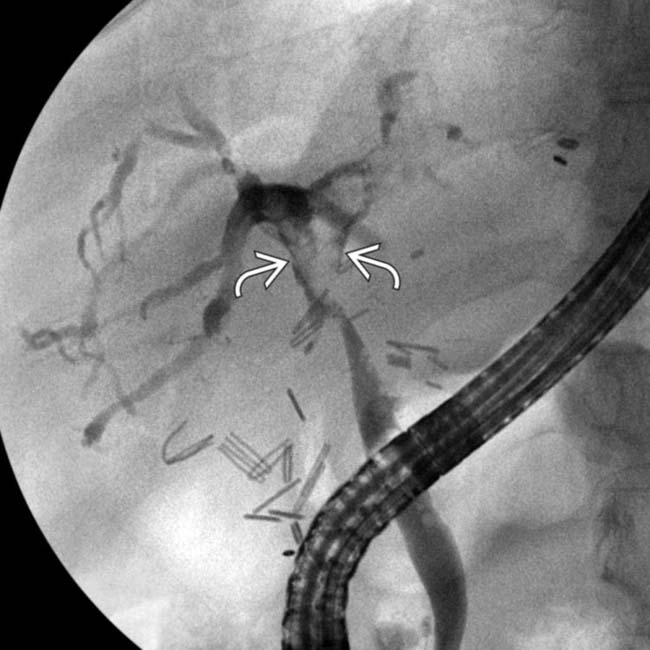
 , and diffusely irregular intrahepatic ducts. The patient’s course was complicated by portal vein thrombosis and rejection, but the hepatic artery was patent on US.
, and diffusely irregular intrahepatic ducts. The patient’s course was complicated by portal vein thrombosis and rejection, but the hepatic artery was patent on US.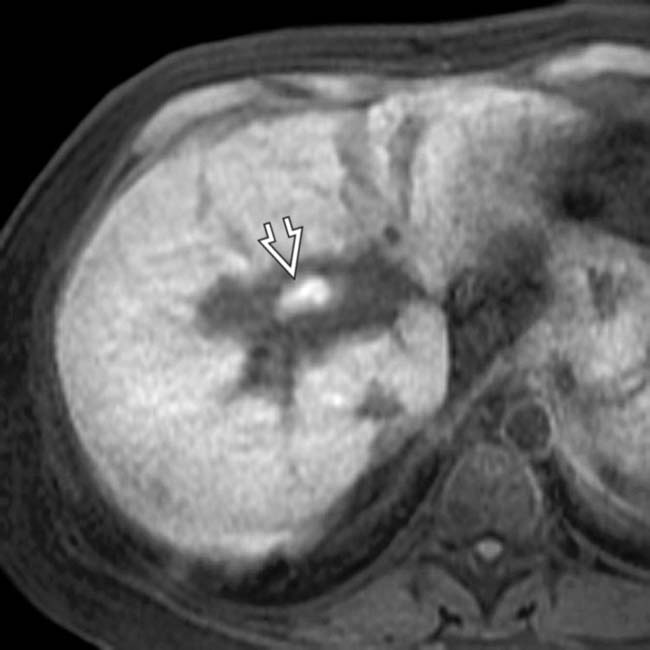
 at the duct bifurcation. Multiple ischemic and immunological insults may result in the strictures and casts that are characteristic of ischemic cholangiopathy.
at the duct bifurcation. Multiple ischemic and immunological insults may result in the strictures and casts that are characteristic of ischemic cholangiopathy.IMAGING
General Features
• Location
 Predominant involvement of middle 1/3 of common bile duct and hepatic duct confluence > intrahepatic ducts
Predominant involvement of middle 1/3 of common bile duct and hepatic duct confluence > intrahepatic ducts
 Predominant involvement of middle 1/3 of common bile duct and hepatic duct confluence > intrahepatic ducts
Predominant involvement of middle 1/3 of common bile duct and hepatic duct confluence > intrahepatic ductsRadiographic Findings
• Cholangiography (ERCP or PTC) is gold standard for diagnosis of ischemic cholangitis
 Luminal irregularity of bile ducts with beaded appearance (alternating sites of stenosis, normal ducts, and mild dilatation)
Luminal irregularity of bile ducts with beaded appearance (alternating sites of stenosis, normal ducts, and mild dilatation)
 Luminal irregularity of bile ducts with beaded appearance (alternating sites of stenosis, normal ducts, and mild dilatation)
Luminal irregularity of bile ducts with beaded appearance (alternating sites of stenosis, normal ducts, and mild dilatation)– Strictures evolve over time, beginning as sites of irregularity and developing into fibrotic strictures
CT Findings
• Scattered irregular biliary dilatation with bile duct wall thickening and hyperenhancement
 Presence of intrahepatic biloma or liver infarct in post-transplant setting should prompt careful assessment of hepatic artery for HAT/HAS
Presence of intrahepatic biloma or liver infarct in post-transplant setting should prompt careful assessment of hepatic artery for HAT/HAS
 Bile duct casts, highly suggestive of ischemic cholangiopathy, appear as linear hyperdense material within bile duct
Bile duct casts, highly suggestive of ischemic cholangiopathy, appear as linear hyperdense material within bile duct
 Presence of intrahepatic biloma or liver infarct in post-transplant setting should prompt careful assessment of hepatic artery for HAT/HAS
Presence of intrahepatic biloma or liver infarct in post-transplant setting should prompt careful assessment of hepatic artery for HAT/HAS Bile duct casts, highly suggestive of ischemic cholangiopathy, appear as linear hyperdense material within bile duct
Bile duct casts, highly suggestive of ischemic cholangiopathy, appear as linear hyperdense material within bile ductMR Findings
• Hepatobiliary contrast agents (i.e., Eovist) can be used for cholangiographic images in hepatobiliary phase
• T2WI, MRCP, and T1WI C+ Eovist cholangiographic images demonstrate luminal irregularity, stenosis, and scattered biliary ductal dilatation
• Linear high T1 signal intensity may be visualized within dilated central ducts, characteristic of biliary cast
• Advantage of noninvasively evaluating other biliary complications (anastomotic stricture, stones, leak, etc.)
Ultrasonographic Findings
• Grayscale ultrasound
 Advanced biliary ischemia due to HAT or HAS may result in presence of intrahepatic fluid collections (bilomas)
Advanced biliary ischemia due to HAT or HAS may result in presence of intrahepatic fluid collections (bilomas)
 Advanced biliary ischemia due to HAT or HAS may result in presence of intrahepatic fluid collections (bilomas)
Advanced biliary ischemia due to HAT or HAS may result in presence of intrahepatic fluid collections (bilomas)• Pulsed Doppler
 Evaluate for evidence of HAT or HAS
Evaluate for evidence of HAT or HAS
 Evaluate for evidence of HAT or HAS
Evaluate for evidence of HAT or HAS– Hepatic artery stenosis (or chronic HAT with collaterals)
 Tardus parvus waveform (systolic acceleration time > 100 msec): Rounded spectral Doppler waveforms with delayed systolic upstrokes
Tardus parvus waveform (systolic acceleration time > 100 msec): Rounded spectral Doppler waveforms with delayed systolic upstrokes




 Tardus parvus waveform (systolic acceleration time > 100 msec): Rounded spectral Doppler waveforms with delayed systolic upstrokes
Tardus parvus waveform (systolic acceleration time > 100 msec): Rounded spectral Doppler waveforms with delayed systolic upstrokesStay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree