Series
Total patients
No. with prior RT
Dose and fractionation
Local control (LC)
Toxicity
Guckenberger et al. (2010)
19
7
Median dose: 15 Gy in 3 fractions prescribed to 65 % isodose
3-year LC: 81 %
3-year LC: 100 % (re-irradiation patients)
25 %: > grade 2 late
Deodato et al. (2009)
11
5
20–30 Gy in 4–5 fractions prescribed to the 95 % isodose line
2-year LC: 82 %
0 %: > grade 2 acute and late
Kunos et al. (2009)
5
5
15–24 Gy in 3 fractions
3 complete responses, 2 partial responses
1/5: grade 3 acute (fatigue)
Dewas et al. (2011)
16
16 (5 gyne)
36 Gy in 6 fractions over 3 weeks prescribed to 80 % isodose line
1-year LC: 51 % (for entire cohort)
0 %: ≥ grade 3
Kunos et al. (2008)
3
3
24 Gy in 3 fractions
PFS: 1–3 months (all out-of-field recurrence)
0 %: ≥ grade 3
Seo et al. (2014)
23
17
27–45 Gy in 3 fractions prescribed to 80 % isodose line
2-year LC: 65 % (entire cohort)
3/17: grade 4 (fistula)
Abusaris et al. (2012)
27 (8 gyne)
27 (8 gyne)
Median maximum SBRT dose EQD2 = 90 Gy (42–420 Gy)
1-year LC: 64 %
2-year LC: 53 %
Median OS: 14 months
0 %: ≥ grade 3 acute
0 %: ≥ grade 3 late
Park et al. (2015)
85
71
Median dose: 39 Gy in 3 fractions prescribed to median 80 % isodose line (BED = 90 Gy)
2-year LC: 83 %
5-year LC: 79 %
5/85: ≥ grade 3 late
(2 rectovaginal fistula)
Pontoriero et al. (2015)
5
5
15–20 Gy in 3–4 consecutive fractions, prescribed to median isodose line 72 % (BED = 83 Gy)
3 complete responses, 2 partial responses
0 %: ≥ grade 3 within 90 days of SBRT
Guckenberger et al. (2010) described the use of stereotactic radiotherapy in 19 patients with recurrent cervix and endometrial cancer; seven had received radiotherapy as part of their initial treatment. These recurrences were either central or pelvic sidewall and ranged in size from 1.5 to 6.5 cm. These patients were treated with stereotactic radiotherapy alone and were prescribed either 30 Gy in 3 fractions or 28 Gy in 4 fractions prescribed to the 65 % isodose line. Systemic failure was the main cause of death, occurring in 7/10 patients. There were also significant rates of late ≥ grade 2 toxicity at 25 %. Unfortunately, this study did not separate their results for patients who had received previous radiotherapy. The role of SBRT has also been investigated in patients specifically with recurrent cervical cancer. One study involved 11 patients, 5 of whom had previous radiotherapy (Deodato et al. 2009). The commonly used treatment regimen consisted of 5 fractions of 6 Gy prescribed to the 95 % isodose line (EQD2 = 40 Gy). After a median follow-up of 18 months, there were two local failures. Treatment was well tolerated as there was no ≥ grade 2 late toxicity reported. Another study retrospectively reviewed 23 patients with locally recurrent cervical cancer limited to the pelvic sidewall (Seo et al. 2014). Seventeen of these patients had prior radiotherapy. Stereotactic doses ranged from 27 to 45 Gy (median, 39 Gy) in 3 fractions prescribed to the 80 % isodose line. For the entire cohort, the 2-year overall survival and local control rates were 43 % and 65 %, respectively. Patients with tumor volumes <30 cm3 did significantly better than those with larger tumors. There were three cases of rectovaginal fistula (grade 4 toxicity), which all occurred in patients with larger tumors. Seventy-one percent of patients were able to achieve an analgesic reduction of ≥50 % from baseline.
Kunos et al. (2009) described the first use of CyberKnife radiosurgery in three patients with recurrent squamous cell carcinoma of the vulva after primary radiotherapy. Treatment consisted of 3 fractions of 8 Gy prescribed to the 75 % isodose line (EQD2 57.6 Gy). All patients developed acute skin irritation and desquamating necrosis within the treatment field, although all healed and there were no late toxicities reported. Although all three patients responded locally, they all developed progressive disease within 3 months of radiosurgery. A similar study evaluating the role of CyberKnife SBRT for patients with recurrent or oligometastatic cervical cancer was conducted in 85 patients by the Korean Radiation Oncology Group. The sites treated with SBRT were within the prior radiotherapy field in 59 cases and partially overlapped in nine cases. With a median dose of 39 Gy in 3 fractions (BED = 90 Gy), the 2-year and 5-year local control rates were 83 % and 79 %, respectively. A disease-free survival interval >36 months was found to be significant for both local control and overall survival. Late grade 3–4 toxicity occurred in five patients with rectovaginal fistula occurring in two patients (Park et al. 2015).
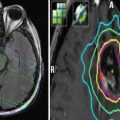
In conclusion, stereotactic radiotherapy is safe and feasible for patients with gynecological malignancies receiving re-irradiation to the pelvis. Results are promising with respect to treatment tolerance and local control. The short treatment times are also beneficial for palliative patients. Future directions may include the use of adaptive replanning in clinical scenarios of rapid tumor regression and/or anatomical changes to help with dose escalation and OAR avoidance.
3.3 Intraoperative Radiotherapy
Intraoperative radiotherapy can be delivered by two techniques: electron beam radiotherapy delivered using a linear accelerator or HDR brachytherapy using interstitial catheters. Intraoperative radiotherapy is typically reserved for cases of microscopic disease after surgery. Its benefit is that a single high-dose fraction can be delivered during surgery when adjacent OARs can be mobilized away from the target. Organs at risk include the pelvic nerves and ureters. Potential complications of intraoperative radiotherapy include damage of these structures leading to neuropathic pain, motor deficits, and ureteral obstruction. A summary of published series evaluating the role of IORT for recurrent gynecological malignancies is summarized in Table 2.
Table 2
Series demonstrating use of intraoperative radiotherapy (IORT) for re-irradiation
Series | Patients | Prior RT | IORT details | Local control | Toxicity |
|---|---|---|---|---|---|
Martinez Monge et al. (1993) | 26 | 14 | Median cone size: 8 cm (5–12 cm) Median dose: 15 Gy (10–25 Gy); median electron beam energy: 9 MeV (6–15 MeV) | 4-year LC: 33 % | ≥ grade 3 GU: 1/14 ≥ grade 3 GI: 0 Chronic pain: 6/14 |
Mahe et al. (1996) | 70 | 54 | Mean cone size: 7.5 cm (4–9 cm) Mean dose: 18 Gy (10–25 Gy) Mean energy: 12 MeV (6–20 MeV) | Median LC: 21 % | 14 % IORT-related complications (5 neuropathies, 4 ureteral obstructions, 1 rectal stricture) |
Tran et al. (2007) | 36 | 23 | Mean cone size: 6 cm (2.85–10 cm) Mean dose: 11.5 Gy (6–17.5 Gy) Energy: 6–12 MeV | 5-year LC: 44 % for entire cohort | ≥ grade 3: 28 % for entire cohort |
Gemignani et al. (2001) | 17 | 14 | Mean dose: 14 Gy (12–15 Gy) | 3-year LC: 67 % | Grade 2–3 toxicity: 58 % No life-threatening toxicity |
Stelzer et al. (1995) | 22 | 11 | Median cone size: 6 cm (6–15 cm) Median dose: 22 Gy (14–28 Gy) Median energy: 12 MeV (9–22 MeV) | 5-year LC: 48 % | Most common toxicity neuropathy: 7/22 treatment related |
Mahe et al. (1996) published on 70 patients who received IORT for pelvic recurrence after initial treatment with radiotherapy. These patients largely had pelvic side wall disease ± central disease. Surgery varied according to initial treatment and tumor size. At 15-month follow-up, the median survival was only 11 months, and local control was 21 %. Grade 2–3 toxicity was observed in 27 % of patients and included GI or urinary fistulas, infection, rectal stricture, neuropathy, and ureteral obstruction. Another study retrospectively evaluated the role of IORT for patients with recurrent gynecological malignancies. Of the 36 patients reviewed, 23 had previous radiotherapy. The 5-year local control rate was 44 % and rates of grade 3+ toxicity were 28 %. Multivariate analysis found that disease-free interval, tumor size, cervical cancer primary and previous surgery were significant prognostic factors (Tran et al. 2007). Gross tumor resection has also been found to be significant prognostic factor (Gemignani et al. 2001). A single institution retrospective review compared the addition of IORT to surgically treated patients, all of whom has previously received pelvic radiotherapy. It found that the addition of IORT did not improve clinical outcomes (Backes et al. 2014). It should be noted that the patients who received IORT tended to have poorer prognostic features, such as shorter disease-free interval and increased lateral tumor extension.
In summary, IORT has been shown to provide reasonable local control for patients with recurrent gynecological malignancies; however, rates of toxicity are not trivial. Careful patient selection is paramount.
3.4 Brachytherapy
Brachytherapy is a useful modality in the treatment of local recurrences, allowing dose escalation with a favorable therapeutic ratio. Late toxicity is reported as being less significant in patients re-irradiated with brachytherapy as opposed to EBRT (Russell et al. 1987), in part because of the rapid dose falloff that can be achieved around the target volume, limiting dose to normal tissues. Both HDR and LDR have been used in the radical setting with no difference in outcome or toxicity. Local control rates in the re-irradiation setting have ranged from 67 to 100 % in some series, particularly in small recurrences (Xiang et al. 1998; Petignat et al. 2006). Toxicities have included severe vaginal stenosis and GI toxicity rates of up to 25 %.
Multichannel applicators typically use line sources not limited to the center of the applicator but also on the edges or surfaces of the cylinder. This allows for asymmetric and conformal dose distributions to be delivered sparing the rectum and bladder but increasing vaginal mucosa dose as compared to single-channel applicators (Tanderup and Lindegaard 2004). Selected brachytherapy series are shown in Table 3.
Table 3
Series demonstrating the use of brachytherapy for re-irradiation
Series | Total patients | No. with prior RT | Dose and fractionation | Local control (LC) | Toxicity |
|---|---|---|---|---|---|
Brachytherapy (BT) | |||||
Xiang et al. (1998) | 73 | 73 | Radium therapy: 30–40 Gy in 3–5 fractions or HDR 20–35 Gy in 3–5 fractions over 3–4 weeks Followed by vaginal mold: 20–30 Gy in 4–6 fractions at 5 mm depth 30–40 Gy EBRT to involved vulva or groin | 5-year LC: 67 % | Grade 4 toxicity: 24.6 % |
Petignat et al. (2006) | 22 | 2 | Median HDR BT: 26 Gy (range, 8–48 Gy) in a median of 4 fractions (1–11) | 5-year LC 100 % | > grade 2 acute: 0 % > grade 2 late GI: 18 % > grade 2 late vaginal: 50 % |
Interstitial implants | |||||
Brabham and Cardenes (2009) | 19 | 19 | Median dose: 50 Gy (range, 25–55 Gy) | 21-month LC: 63 % | > grade 2: 5.3 % |
Badakh and Grover (2009) | 22 | 22 | Median dose: 25.8 Gy (range, 12–45 Gy) delivered BID, 4–6 Gy per fraction | LC: 22.7 % | Grade 4 toxicity: 18 % |
Jhingran et al. (2003) | 91 | 34 | Median dose: 75 Gy (range, 34–122 Gy) | 5-year LC: 69 % | > grade 2 toxicity: 12.1 % |
Gupta et al. (1999) | 69 | 15 | Median dose: 35 Gy (range, 25–55 Gy) | 3-year LC: 49 % | Grade 4 toxicity: 14 % |
Randall et al. (1993) | 13 | 13 | 30–90 Gy (0.17–0.59 Gy/h) | 2-year LC: 46 % | Grade 4 late: 1/13 (rectovaginal fistula) |
Mabuchi et al. (2014) | 52 | 52 | 42 Gy in 7 fractions, OD on day of implant then BID × 3 days | 32-month LC: 77 % | > grade 3 late: 25 % |
Zolciak-Siwinska et al. (2014) | 20 | 20 | Median EQD2 for re-irradiation: 48.8 Gy (range, 16.0–91.0 Gy) | 3-year LC: 45 % | Grade 3+ toxicity: 15 % |
3.5 Interstitial Brachytherapy
Interstitial brachytherapy allows for highly conformal dose delivery to recurrent disease with the use of catheter needles directly inserted into the tumor. This allows for high-dose radiation treatment to vaginal or pelvic recurrences from gynecological cancers. Interstitial brachytherapy may be a reasonable alternative to surgical salvage in patients with medical comorbidities or when organ sparing is preferred. In cases where surgical salvage is not appropriate due to the location of the recurrent disease, such as the lateral pelvis, interstitial brachytherapy may also be an option. Both permanent interstitial implants and remote afterloading technologies have been employed. Interstitial treatment is not a new technique as it has been studied and available for decades. However, with the introduction of three-dimensional guided imaging, there have been major advancements in the precision of the treatment planning and radiation delivery, and thus the technique has become more readily implemented in many centers.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree