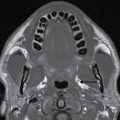
FIG. 24.1 Normal floor of mouth anatomy. Contrast-enhanced CT scans. A: In the coronal plane, the mylohyoid muscle (MH) is identified as a muscular U-shaped sling, the primary muscle forming the floor of the mouth and separating it from the inferolateral submandibular space (star). The paired genioglossus muscles (G) are just lateral to the fatty lingual septum (white arrow). Just below the mylohyoid muscle (MH) is the anterior belly of the digastric muscle (D). The masseter muscle (MM) and lateral pterygoid (L) and medial pterygoid (M) muscles are part of the adjacent masticator space. B: In the axial plane, the fatty lingual septum marks the midline floor of mouth (white arrowhead). The paired genioglossus (G) muscles are lateral to the septum. The sublingual space containing the neurovascular bundle (black arrow) is just medial to the mylohyoid muscle (MH), which is seen arising from the mylohyoid ridge of the mandible. The base of the tongue (BT) is part of the adjacent oropharynx.
Pharynx
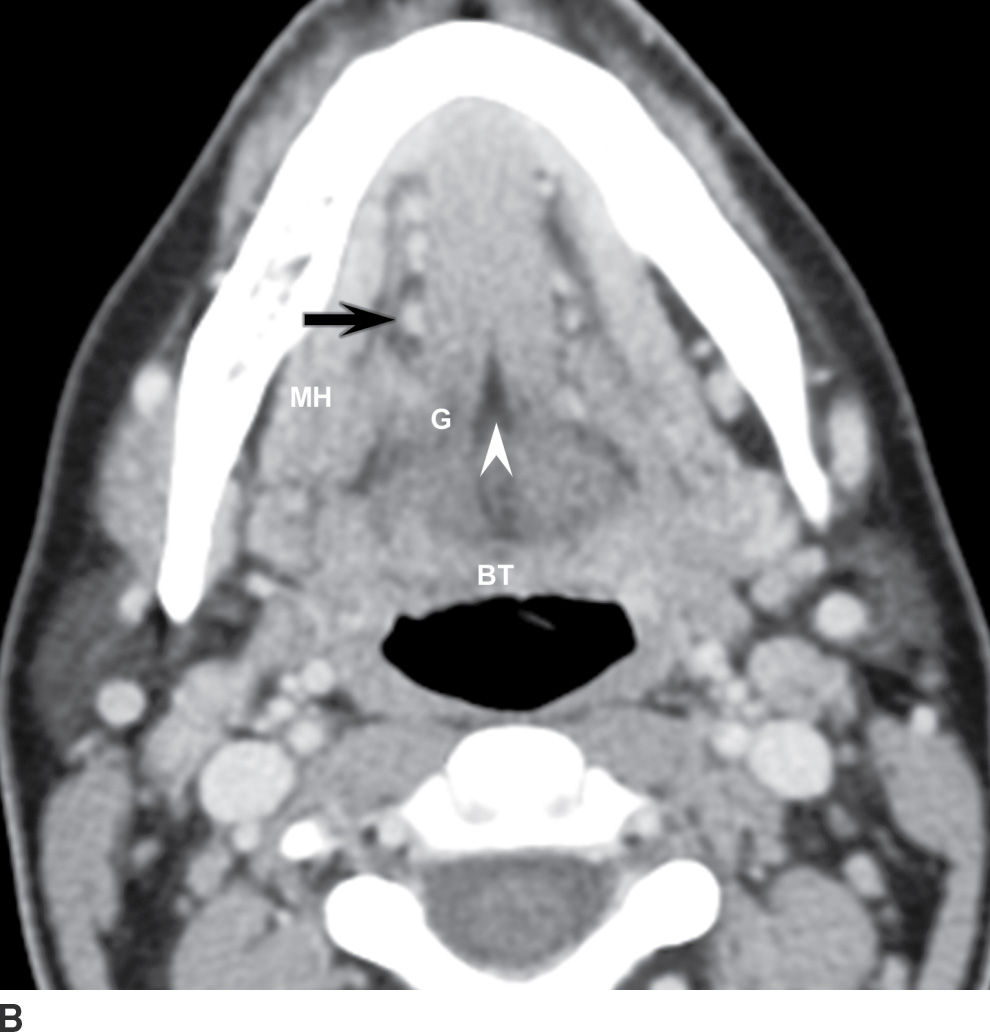
The pharynx is divided into the nasopharynx, oropharynx, and hypopharynx (Fig. 24.2).
FIG. 24.2 Sagittal CT image illustrating the craniocaudal extent of the subsites of the pharynx.
Nasopharynx
The nasopharynx is the superior portion of the pharynx located largely behind and above the hard palate. The anteroinferior extent of the nasopharynx is marked by the upper surface of the soft palate. The nasopharynx contains squamous epithelium, lymphoid tissue, minor salivary gland rests, and the pharyngeal constrictor muscles. Anteriorly, it communicates with the nasal cavity. Its roof consists of the skull base and the C1 and C2 vertebrae. The lateral walls of the nasopharynx consist of the superior pharyngeal constrictor muscles, which attach to the skull base via the pharyngobasilar fascia. A gap along the superior margin of the pharyngobasilar fascia, the sinus of Morgagni, transmits the eustachian tube.
This natural defect in the fascia facilitates spread of nasopharyngeal malignancy to the central skull base and intracranial compartment. Tumors that breach pharyngobasilar fascia can spread directly to the pterygopalatine fossa, skull base fissures, and foramina after which intracranial and sometimes intraorbital perineural spread of tumor can occur. Key anatomic landmarks of the nasopharynx are demonstrated in Figure 24.3.
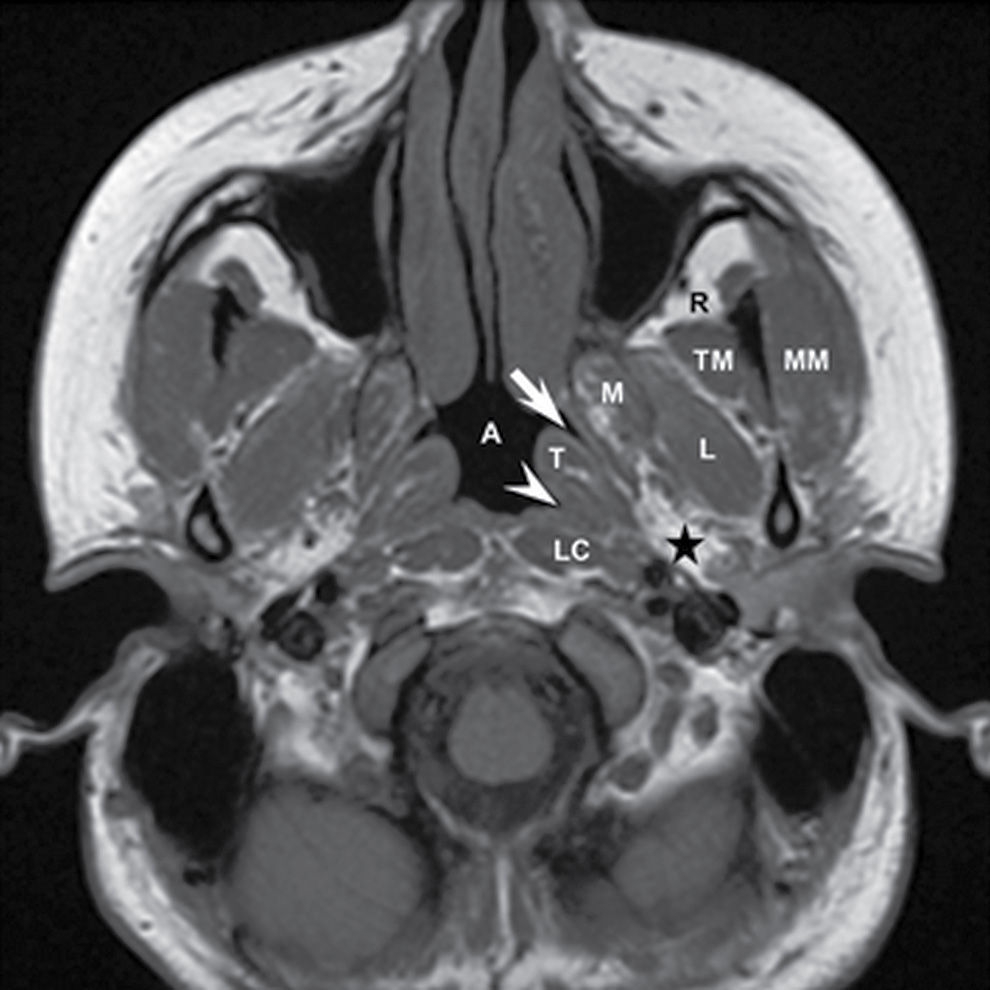
FIG. 24.3 Normal anatomy of the nasopharynx. T1-weighted MR image. Three key anatomic landmarks in the nasopharynx include the eustachian tube orifice (arrow), the torus tubarius (T), and the fossa of Rosenmuller (arrowhead). Additional structures imaged at the level of the nasopharynx include the masseter (MM), temporalis (TM), lateral pterygoid (L), medial pterygoid (M), and longus colli (LC) muscles, the retroantral fat (R), the parapharygeal fat (star), and the nasopharyngeal airway lumen (A).
Oropharynx
The oropharynx is located posterior to the oral cavity and between the nasopharynx superiorly and the hypopharynx inferiorly. The superior margin of the oropharynx is the soft palate, and the inferior margin of the oropharynx is at the level of the superior edge of the hyoid bone. The components of the oropharynx include the posterior third of the tongue (including lingual tonsils), the vallecula, the soft palate, paired palatine tonsils, and the posterior oropharyngeal wall. The glossotonsillar sulcus is the junction of the inferior aspect of the palatine tonsil and the lateral aspect of the base of the tongue (Fig. 24.4). The oropharynx also contains squamous epithelium, lymphoid tissue, and minor salivary rests.

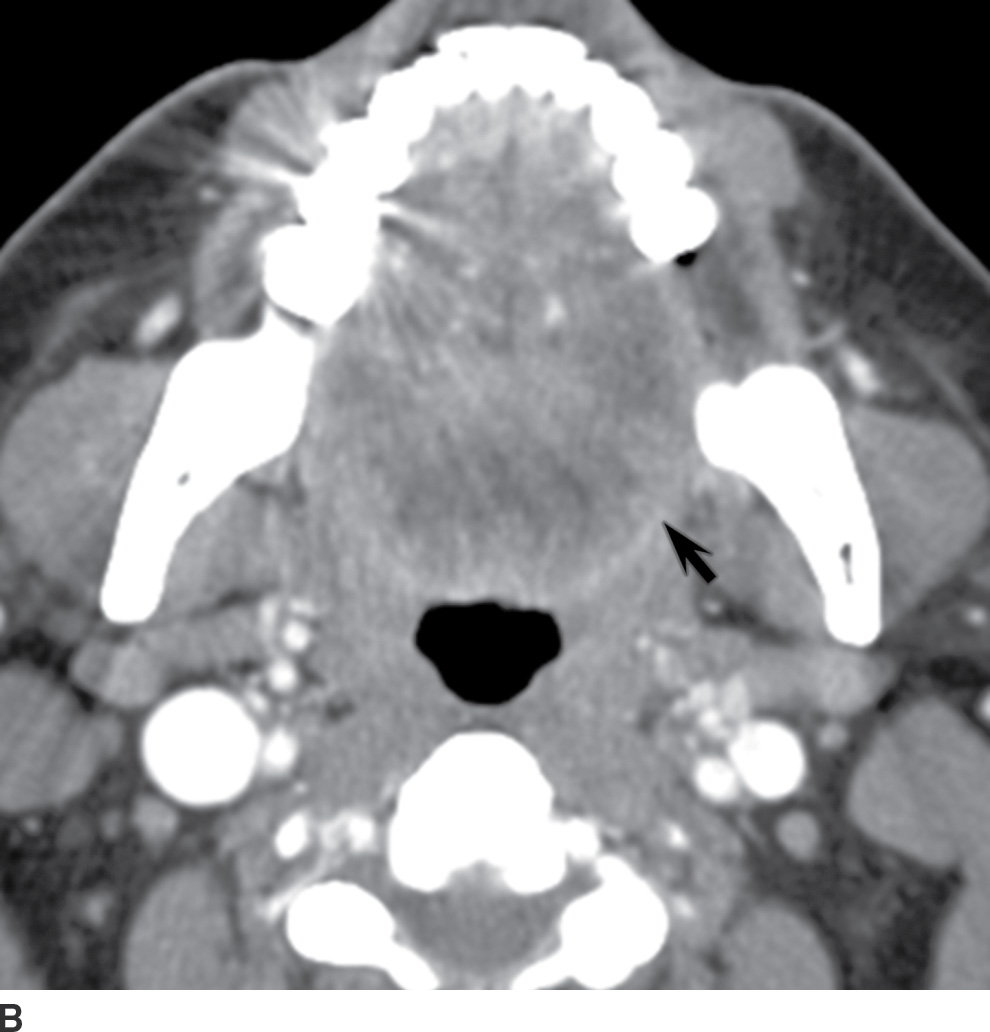
FIG. 24.4 Oropharynx anatomy. Axial contrast-enhanced CT images at the level of the oropharynx. A: The palatine tonsils (arrowheads), base of tongue (white arrow), and posterior wall of the oropharynx (black arrow) are noted at this level. B: The left glossotonsillar sulcus is noted (arrow), and the glossotonsillar sulcus is the junction of the inferior aspect of the palatine tonsil and the lateral aspect of the base of tongue.
Hypopharynx
The hypopharynx is the portion of the pharynx that extends from the lower border of the oropharynx to the cervical esophagus. The superior margin of the hypopharynx is at the level of the hyoid bone, and the inferior margin is the lower aspect of the cricoid ring. The three main subsites of the hypopharynx are the paired piriform sinuses that are situated lateral to the aryepiglottic folds, the posterior wall of the hypopharynx, and the postcricoid region (Fig. 24.5).
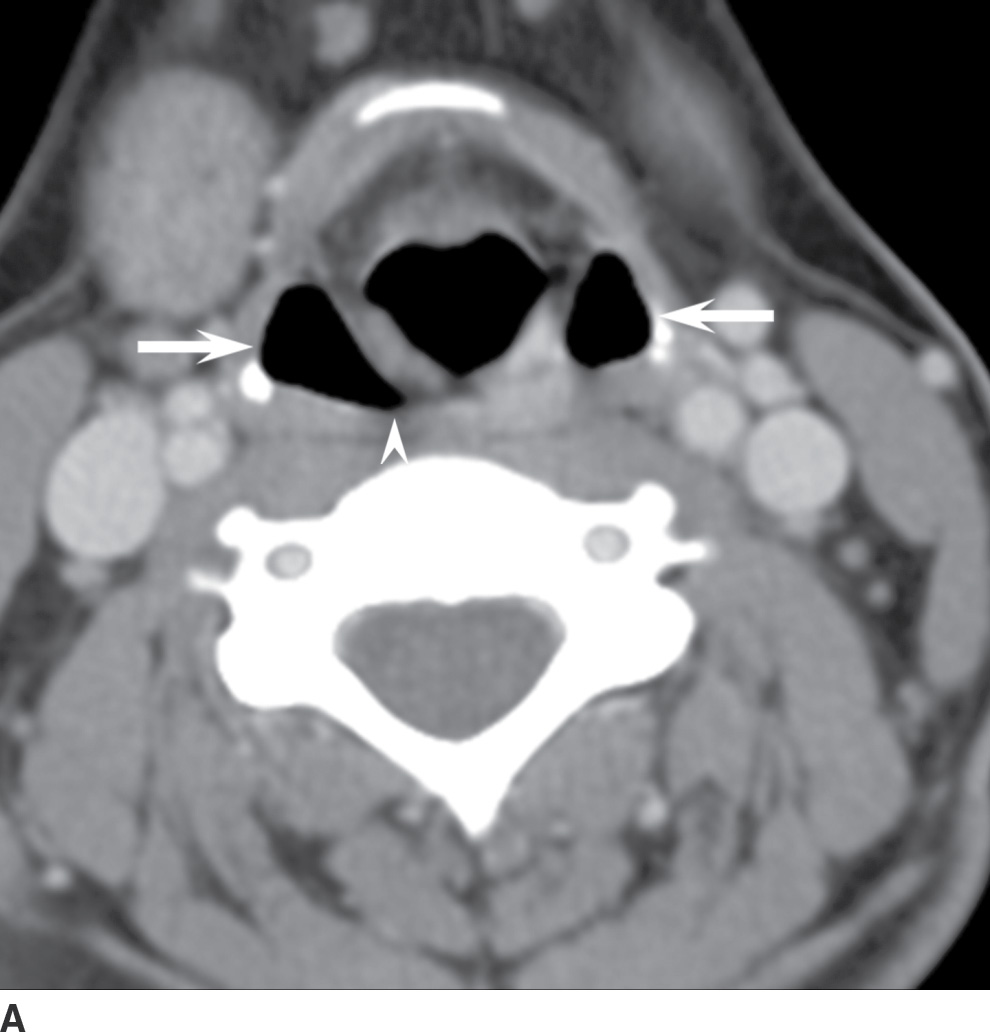
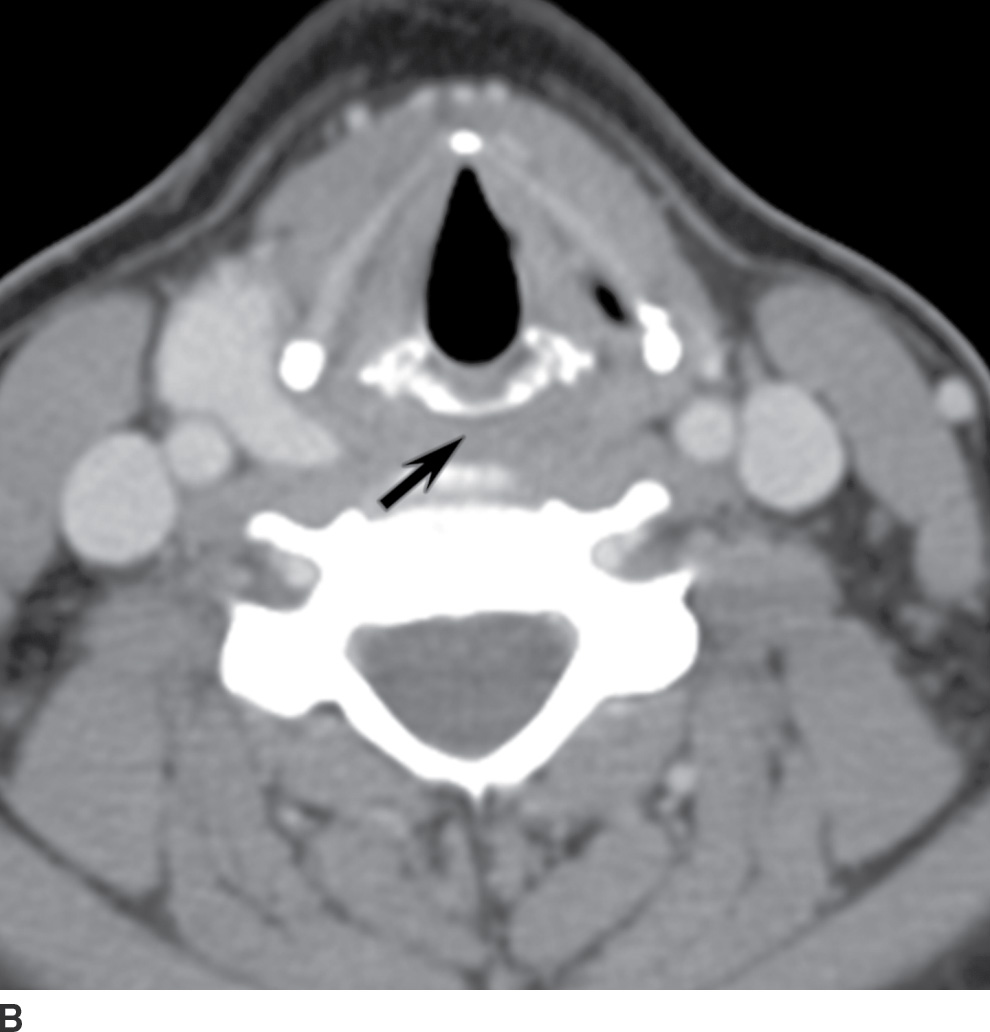
FIG. 24.5 Hypopharynx anatomy. A: The paired piriform sinuses (arrows) and posterior wall (arrowhead) are noted. B: The postcricoid portion (arrow) of the hypopharynx is noted on the more inferior image.
Larynx
Understanding the anatomy of the larynx begins with understanding the functions of the larynx: (i) creating a framework to maintain and protect the airway and (ii) phonation (Fig. 24.6). The cartilaginous backbone of the larynx includes the thyroid cartilage, which looks like a shield and protects the larynx; paired arytenoids that provide support for the true vocal cords; the epiglottis, which protects the airway during swallowing; and the cricoid cartilage, which makes a circumferential ring around the airway and is the only cartilage required to maintain airway patency. The three components of the larynx include the supraglottis, the glottis, and the subglottis.
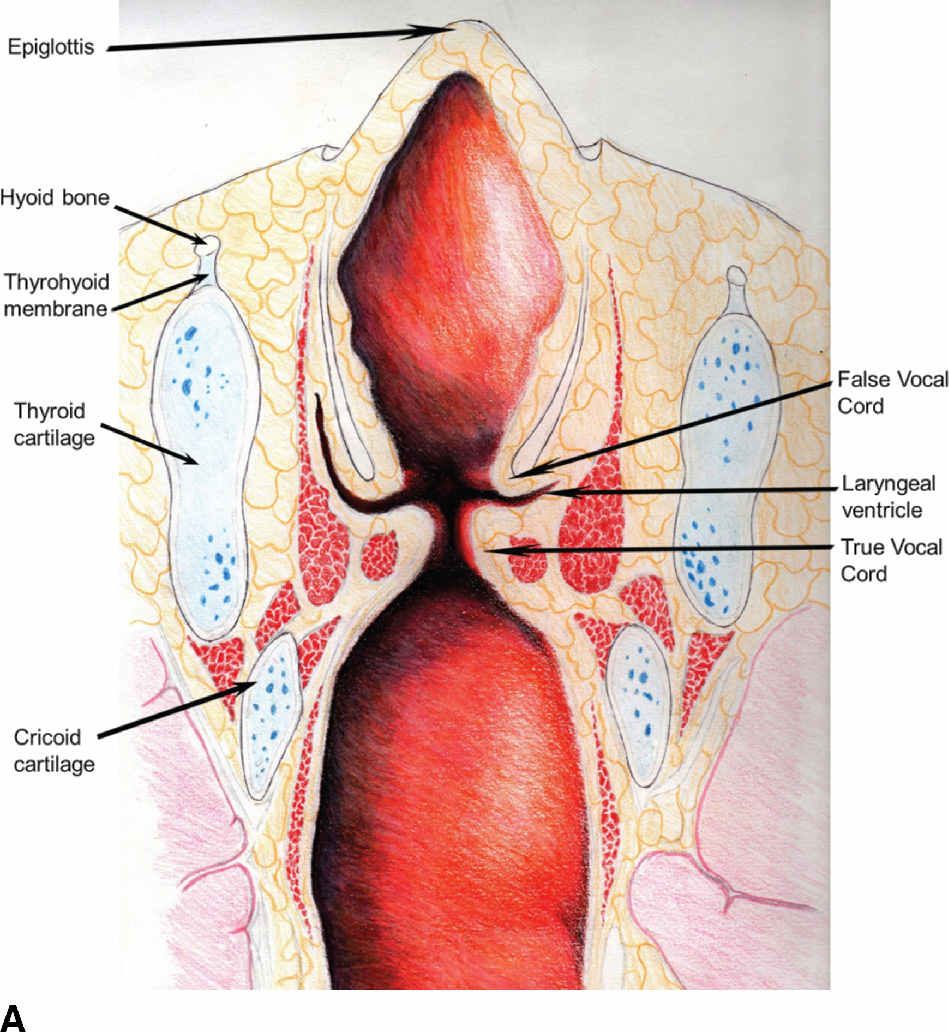
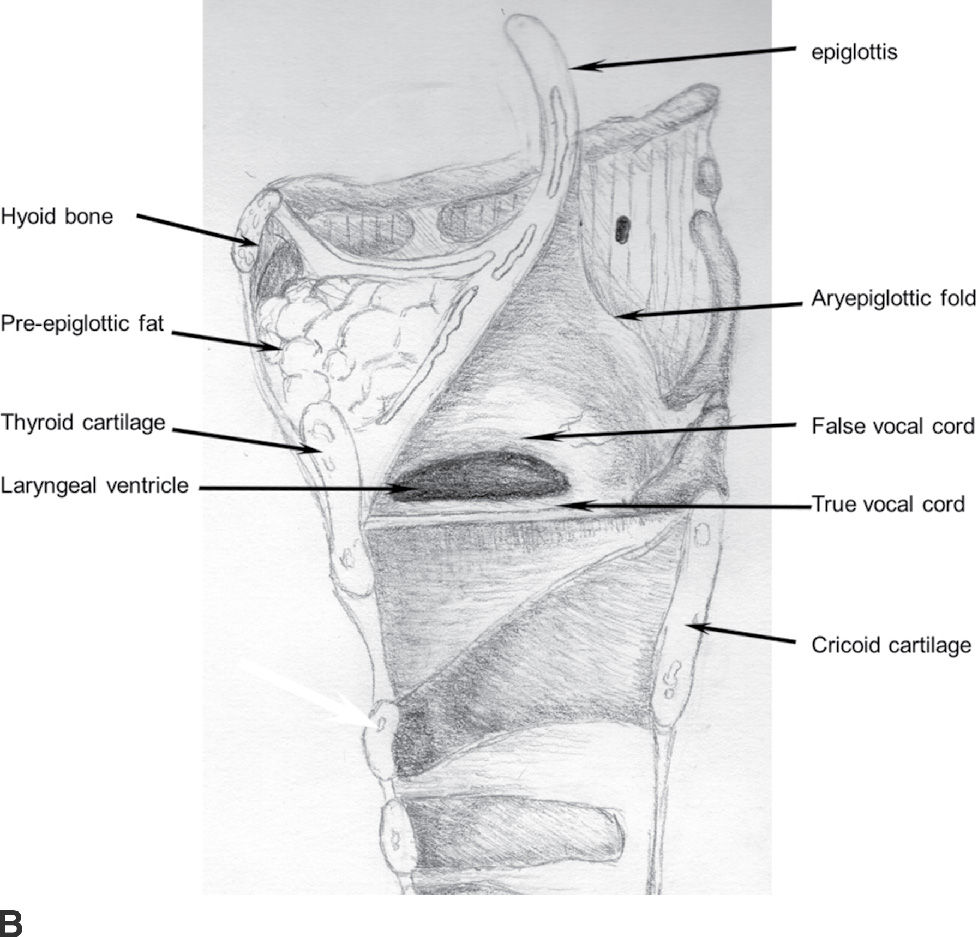
FIG. 24.6 Coronal (A) and sagittal (B) depictions of the larynx.
The supraglottis consists of the epiglottis (which has a free edge portion above the hyoid and an infrahyoid portion below the hyoid and posterior to the pre-epiglottic space), paired aryepiglottic folds, paired false vocal cords, paired arytenoids, and the laryngeal ventricle. The pre-epiglottic space is a fat-filled space anterior to the infrahyoid epiglottis and posterior to the hyoid bone (Fig. 24.7). The paraglottic spaces are the paired fatty areas deep to the false vocal cords. The paraglottic fat merges anteromedially with the pre-epiglottic fat. The paraglottic spaces continue inferiorly medial to the lamina of the thyroid cartilages. The laryngeal ventricle (the space between the false and true vocal cords) separates the supraglottic larynx from the glottic larynx and is considered part of the supraglottis (Fig. 24.8).
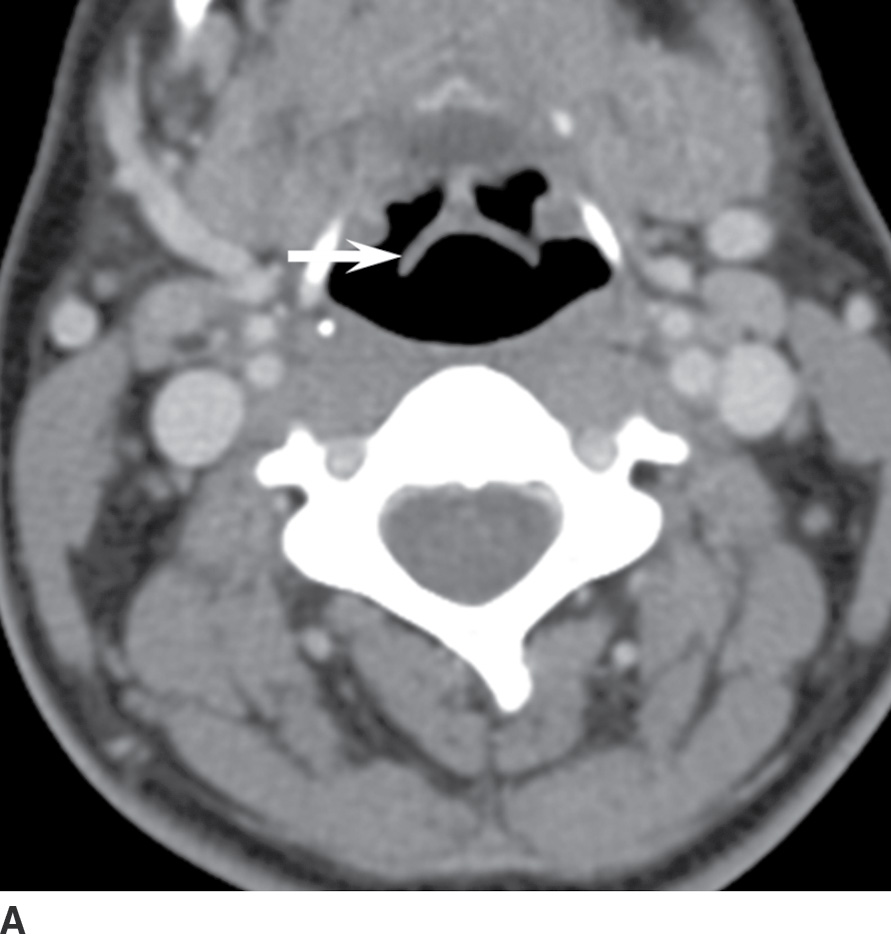
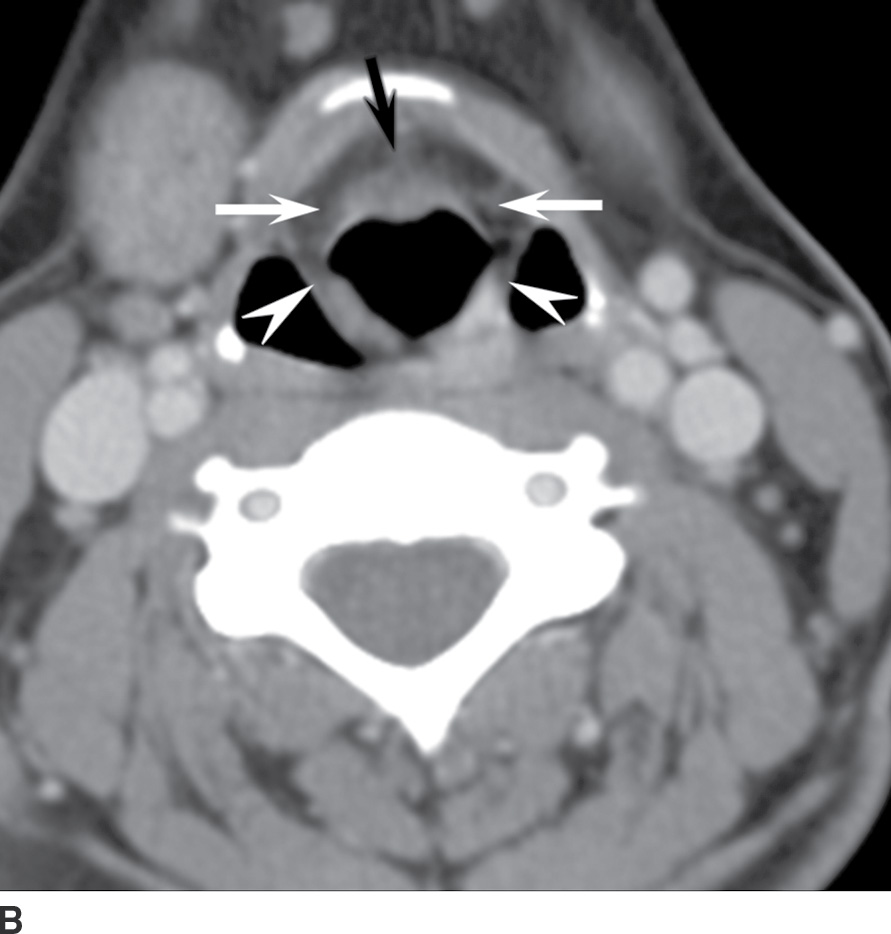

FIG. 24.7 Supraglottic laryngeal anatomy. A: Axial image at the level of the epiglottis (arrow). B: Axial image at the level of the paired aryepiglottic folds (arrowheads). The pre-epiglottic fat is also seen (black arrow) as well as the paired paraglottic fat-filled spaces (white arrows) that will extend inferiorly to the level of the false vocal cords. C: The paired fat-containing false cords are noted (arrowheads).
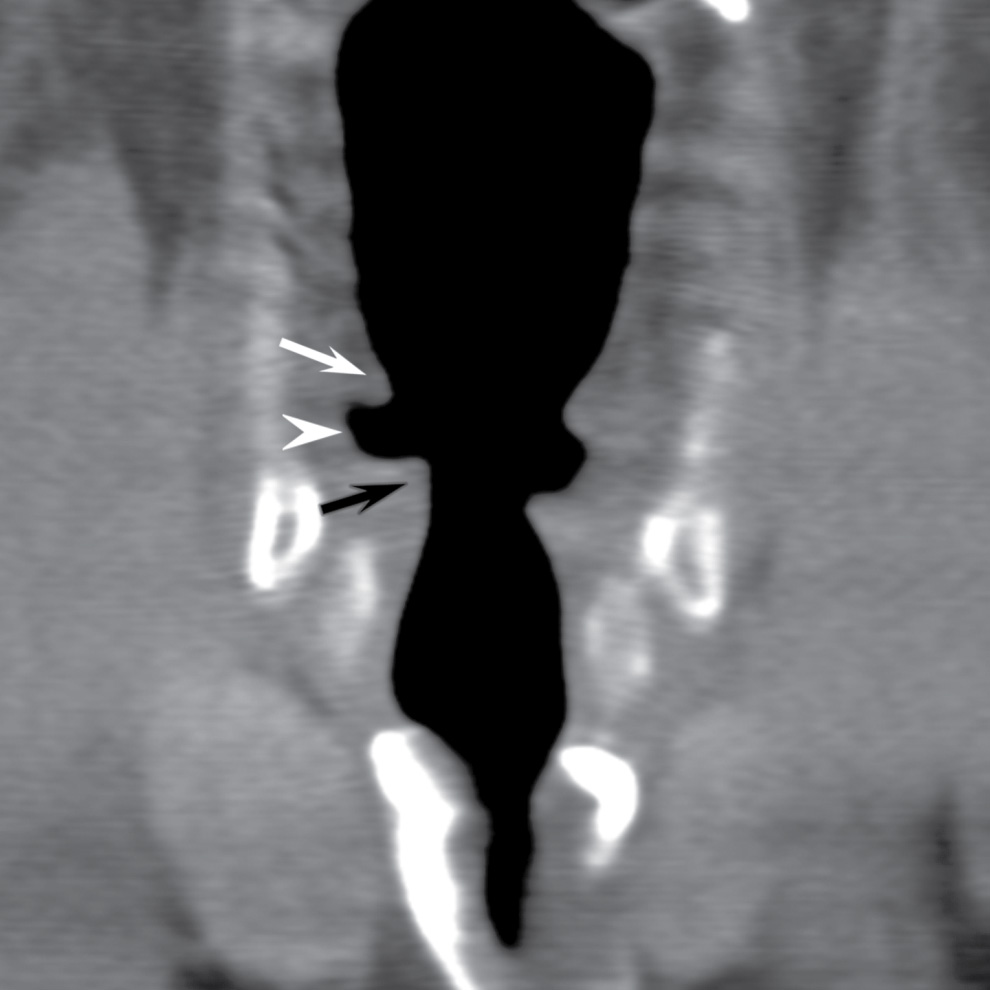
FIG. 24.8 Laryngeal anatomy. Coronal reformatted CT image at the level of the larynx demonstrates the fat-containing false cords (white arrow), gas-filled laryngeal ventricle (arrowhead), and true cords, which are of muscular attenuation (black arrow).
The glottis includes paired vocal cords (the thyroarytenoid muscles), paired vocal ligaments that arise from the vocal process of the arytenoid cartilage and support their respective true vocal cords, the anterior commissure, and the posterior commissure. The anterior commissure is the midline anterior meeting point of the true vocal cords. The posterior commissure is the interarytenoid fold. The subglottic larynx extends from 1 cm below the laryngeal ventricle to the inferior margin of the cricoid cartilage.
Identifying the location of a lesion in the larynx can be challenging at first, and the laryngeal ventricle is not always easy to find to help distinguish the supraglottis and glottis. The supraglottis is identified by the presence of fat (in the pre-epiglottic space, upper paraglottic space, false vocal cords). To locate the level of the glottis, identify the paired thyroarytenoid muscles at the level of the lower cricoarytenoid joint. This is the level of the true cords, and the bulk of the visible paired muscular structures that constitute the true cords are the thyroarytenoid muscles (Fig. 24.9).

FIG. 24.9 The glottis. The level of the true cords is identified by the paired thyroarytenoid muscles (arrowheads) and cricoarytenoid joints (arrows).
Mucosal Cancers
Squamous cell carcinoma
Oral cavity squamous cell carcinoma (SCCA)
Squamous cell carcinoma is the most common malignancy of the oral cavity, though other neoplasms such as lymphoma, minor salivary rest tumors, mesenchymal tumors, and metastases may occur in the oral cavity. SCCA most commonly affects the lip, oral tongue, and floor of mouth in order of decreasing frequency but occurs in other oral cavity subsites as well (4). Although superficial spread of tumor along the mucosa is best assessed on physical examination, radiology is critical in characterizing the deep extent of the tumor, which is often clinically occult and affects management. The following mechanisms of tumor spread should be evaluated in all cases: spread across the midline, mandibular, or maxillary bone involvement, perineural spread, and spread along the pterygomandibular raphe. The pterygomandibular raphe is a ligamentous band that extends from the hamulus of the medial pterygoid plate to the mylohyoid line of the mandible (along the inner cortex of the mandible). For oral tongue and floor of mouth tumors, the report should indicate whether the tumor crosses the midline as this affects the choice of surgical procedure. The presence of nodal metastases must always be assessed, and for oral cavity, lesions are typically found at levels I and II (submental/submandibular, and the anterior cervical lymph chain above the hyoid bone, respectively).
MRI and CT are complimentary in the evaluation of oral cavity tumors. MRI is preferable for characterizing the primary tumor, due to less dental amalgam artifact and better soft tissue resolution, which nicely characterizes oral lesions, particularly tumors involving the hard palate. Perineural spread of tumor is also well characterized with MRI. MRI better demonstrates marrow space involvement, though it has lower specificity due to dental disease and reactive changes (5). The extent of cortical erosion of the mandible or maxilla is best characterized with CT (Figs. 24.10 and 24.11). Describing the degree of mandibular or maxillary erosion if present is important as it determines the extent of mandibulectomy or maxillectomy required. Patients with advanced disease typically require multimodal treatment (surgery, radiation, and chemotherapy), whereas early disease is usually treated with either surgery alone or sometimes radiation alone.
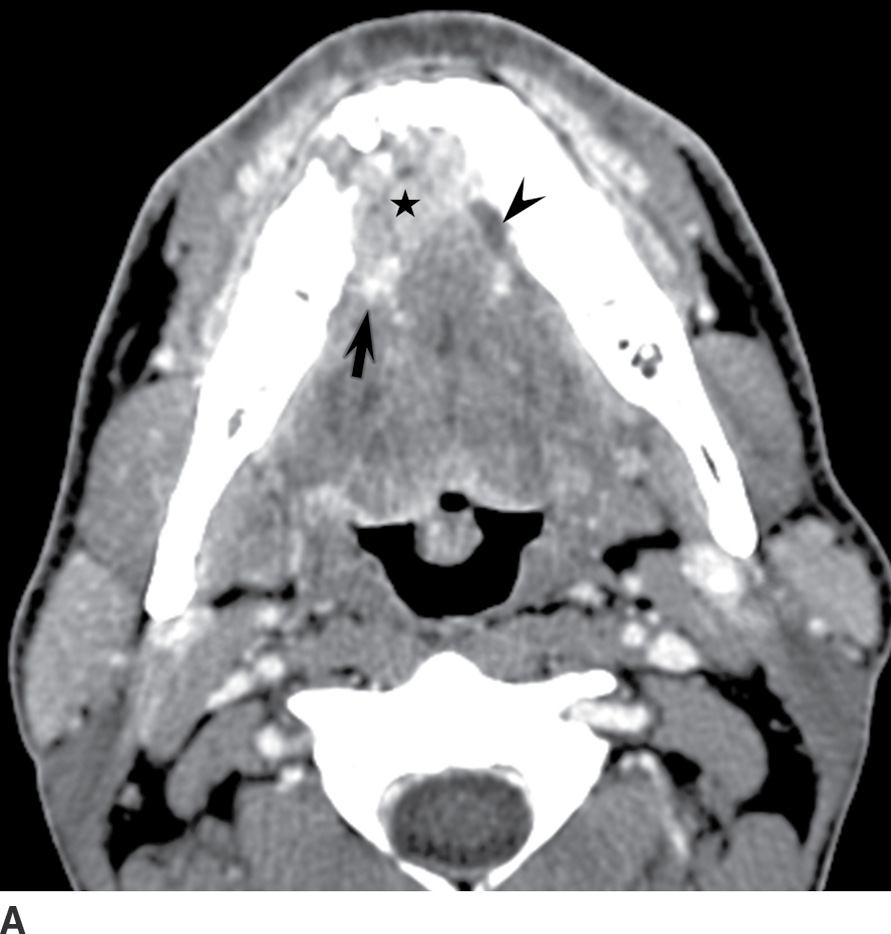

FIG. 24.10 Floor of mouth squamous cell carcinoma. Axial contrast-enhanced CT. A: The enhancing right anterior floor of mouth tumor (star) invades the right neurovascular bundle (arrow) and crosses the midline. There is obstruction of the dilated left Wharton duct (arrowhead). B: Bone windows demonstrate adjacent mandibular cortical erosion (arrow).
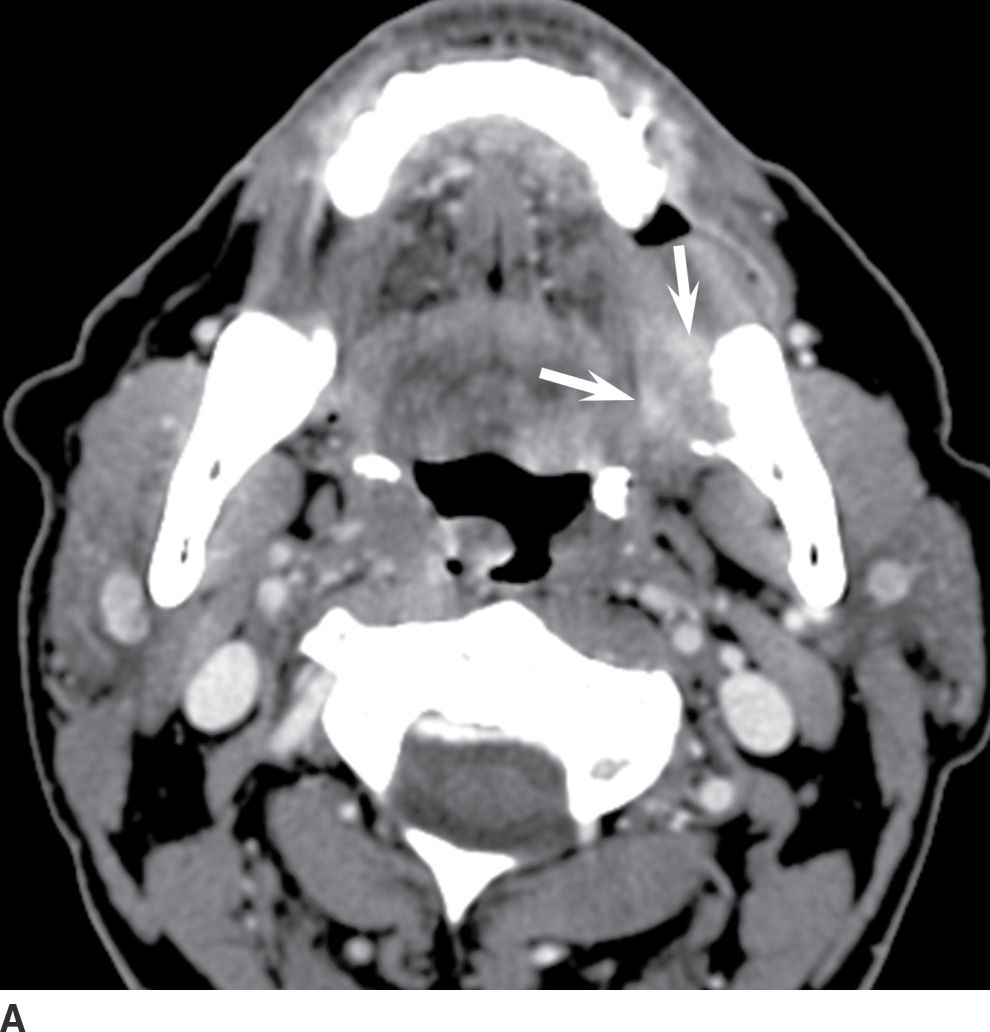
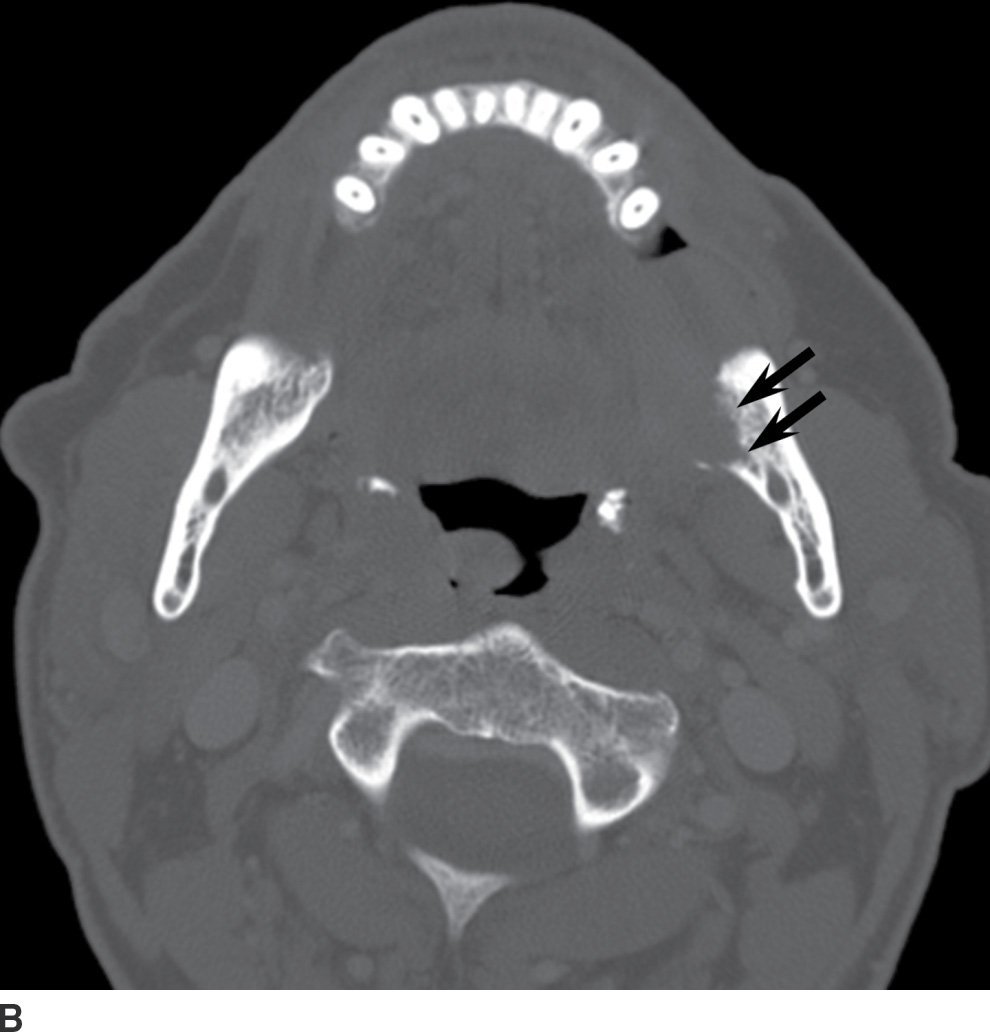
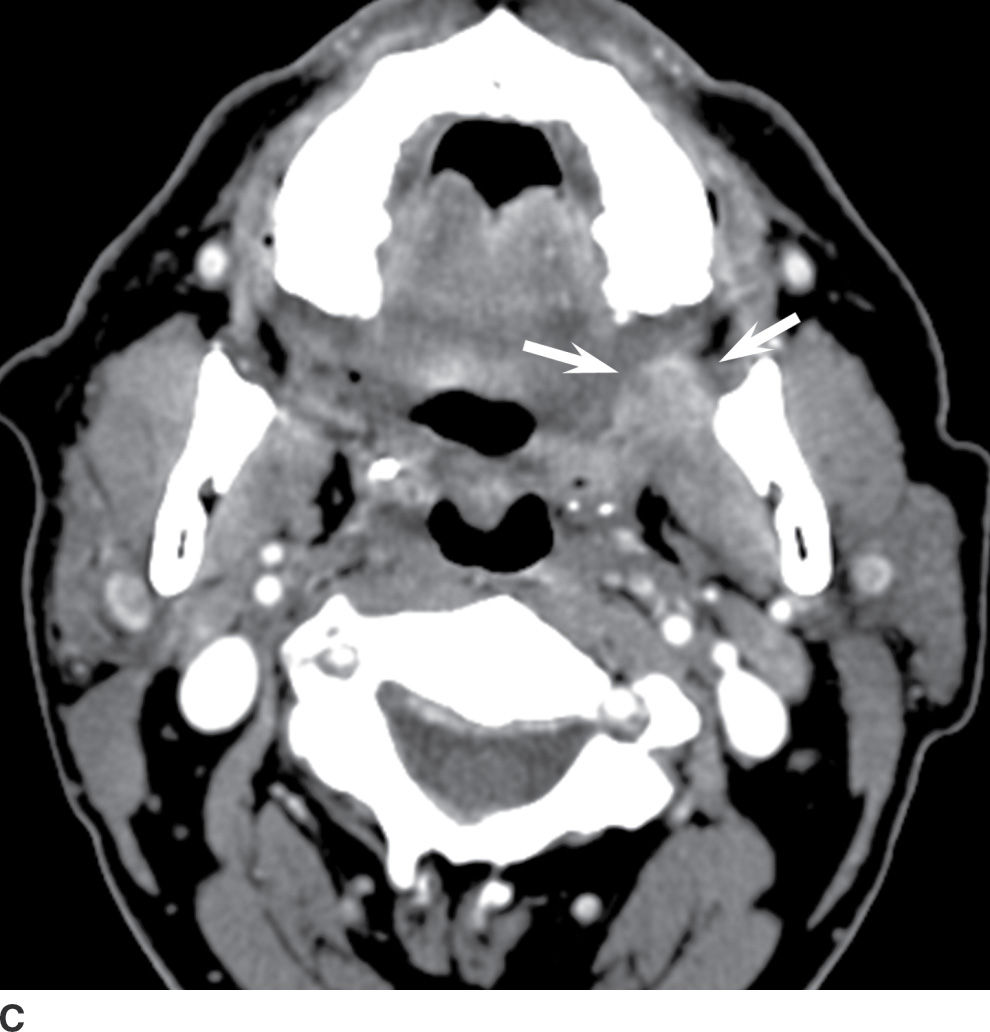
FIG. 24.11 A 52-year-old woman with left mandibular pain and a retromolar trigone cancer. Axial enhanced CT. A: A soft tissue mass arises from the left retromolar trigone (arrows). B: Bone windows demonstrate associated osseous erosion and marrow invasion (arrows). C: There is superior extension along the left pterygomandibular raphe (white arrows). Compare this to the normal contralateral side. There are incidental tonsilloliths in both palatine tonsils.
Nasopharyngeal carcinoma (NPC)
The epidemiology and histopathology of NPC is distinct from that of other SCCAs. It most commonly affects 40- to 60-year-old males. NPC is relatively rare in the United States but is endemic in southern China, where it accounts for 15% to 18% of malignancies (6). Main risk factors include prior EBV infection plus some other risk factors that may include genetic predisposition, environmental risk factors such as dietary carcinogens (e.g., nitrosamines), and/or immunocompromised states (6,7). EBV serology serves as a screening tool in high-risk populations. The most common presentation is cervical lymphadenopathy (lymph node metastases) seen in approximately 85% of patients, though other symptoms include epistaxis, nasal congestion, otalgia, headache, and cranial nerve palsies. There are three histologic types of NPC, summarized in Table 24.1 (8). Type I has the worst prognosis, behaving similar to SCCA arising elsewhere in the pharynx, and is the second most common type of NPC in North America.
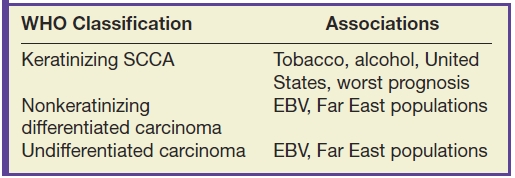
Table 24.1 World Health Organization Histologic Classification of Nasopharyngeal Carcinomas3
MRI plays a critical role in staging NPC, which preferentially spreads submucosally superior and deep to involve the skull base, and typically presents with metastatic cervical lymphadenopathy due to the rich lymphatic supply of the nasopharynx. Most (65%) of NPCs arise in the fossa of Rosenmuller and have T2 intermediate signal hyperintense to muscle (Fig. 24.12). Nodal metastases are typically to retropharyngeal nodes, followed by levels II and V nodes in the cervical lymph chains. This predilection to retropharyngeal metastasis is of critical importance to radiologists because retropharyngeal nodes are usually clinically occult and because occult NPC should be sought whenever retropharyngeal nodes are encountered. The role of the radiologist is to describe the following: the deep extent of the primary tumor, perineural and intracranial extent of tumor, metastatic neck lymph nodes (including situs and largest node), and distant metastasis. The T1-weighted sequence without fat suppression is particularly helpful to delineate tumor infiltration of the fossa of Rosenmuller, parapharyngeal fat, paratubal (eustachian tube) soft tissues, and skull base bone marrow because the normal T1-hyperintense fat will be replaced by hypointense tumor and edema (Fig. 24.13). Tumor extension into the pterygopalatine fossa allows for perineural spread to the orbit, infratemporal fossa (masticator space), and intracranial compartment and is well characterized using both unenhanced T1-weighted and T1-weighted fat-saturated contrast-enhanced sequences. Skull base foramina most commonly at risk for perineural spread include the pterygopalatine fossa, foramen rotundum, the vidian canal, foramen ovale, and foramen lacerum (Fig. 24.14).
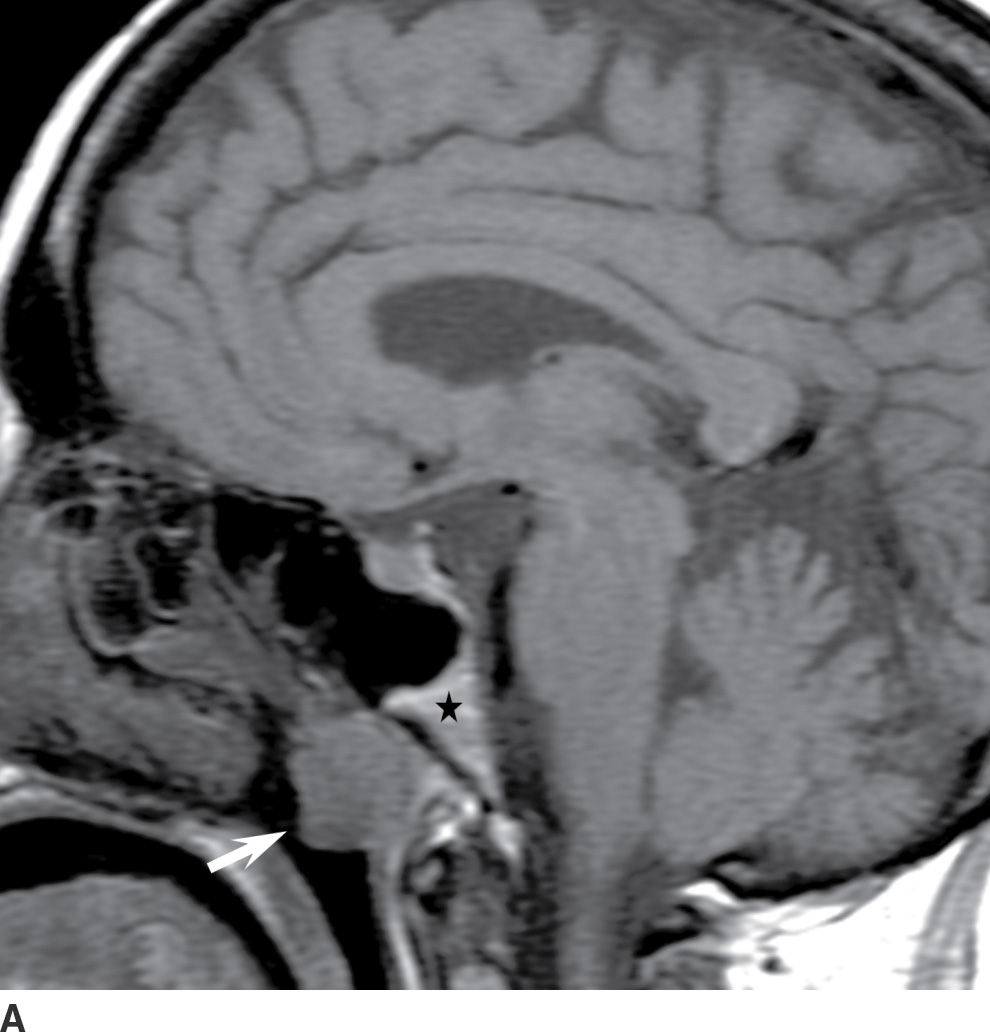
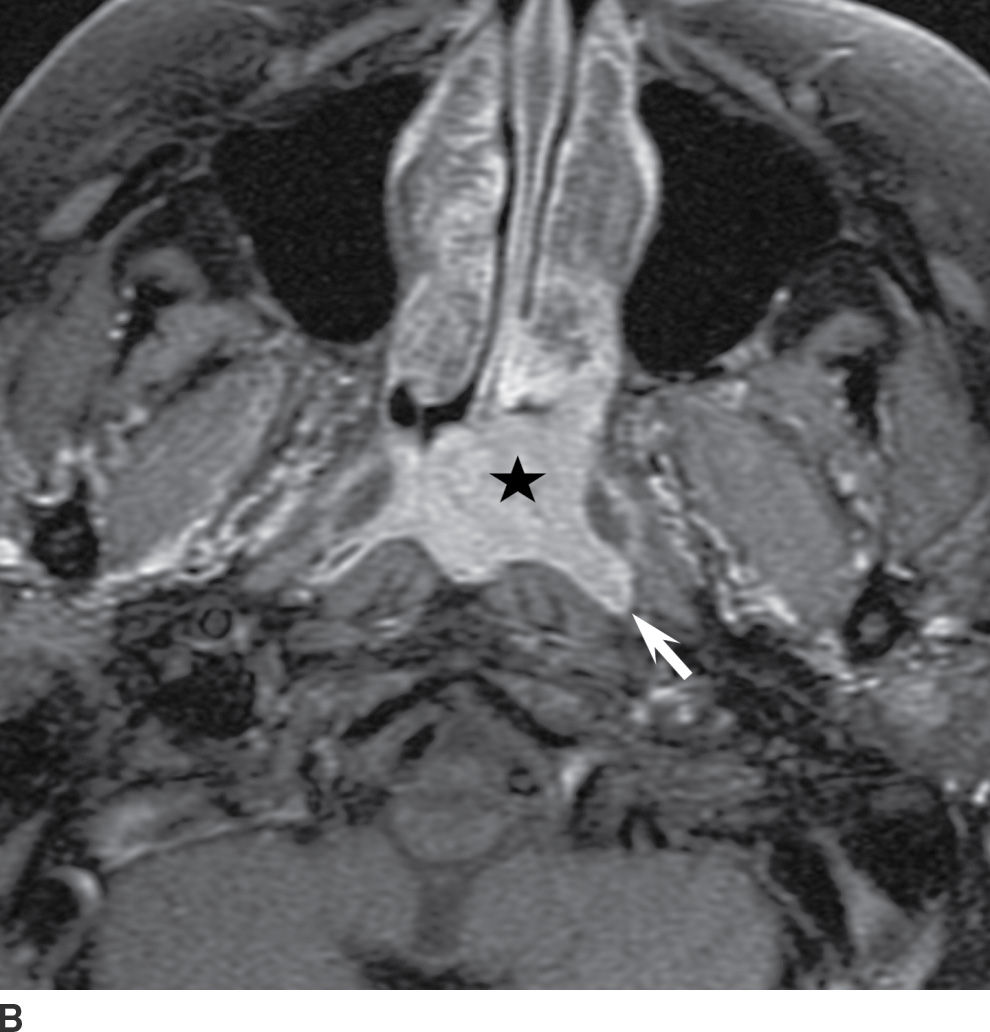
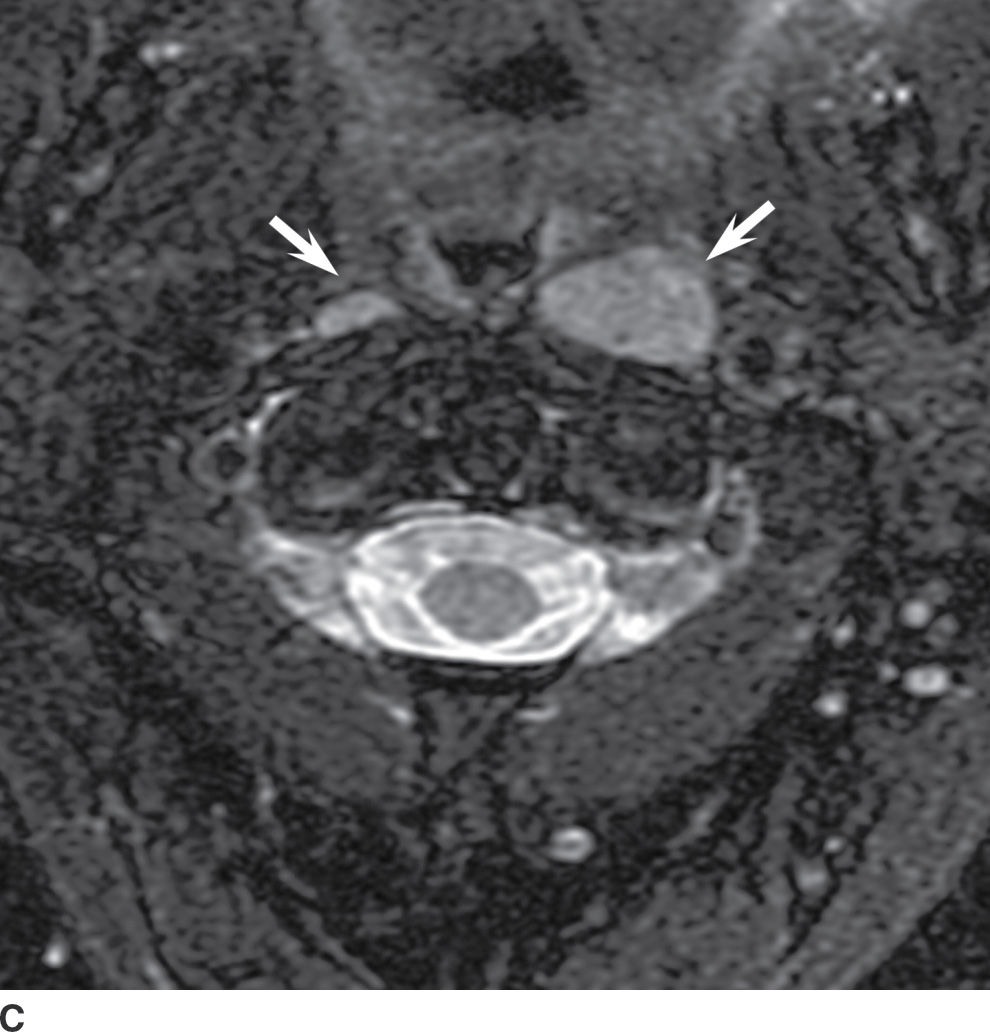
FIG. 24.12 Nasopharyngeal carcinoma. A: Sagittal T1-weighted MRI. Prominent soft tissue (arrow) is present in the nasopharynx. The T1 hyperintense marrow signal (star) of the clivus is preserved. B: Axial contrast-enhanced T1-weighted fat-suppressed MRI. A nasopharyngeal mass (star) is confined to the nasopharyngeal mucosa, arising from the widened left fossa of Rosenmuller (arrow). C: Axial T2 fat-suppressed MRI. Bilateral metastatic retropharyngeal lymph nodes (arrows) are present.
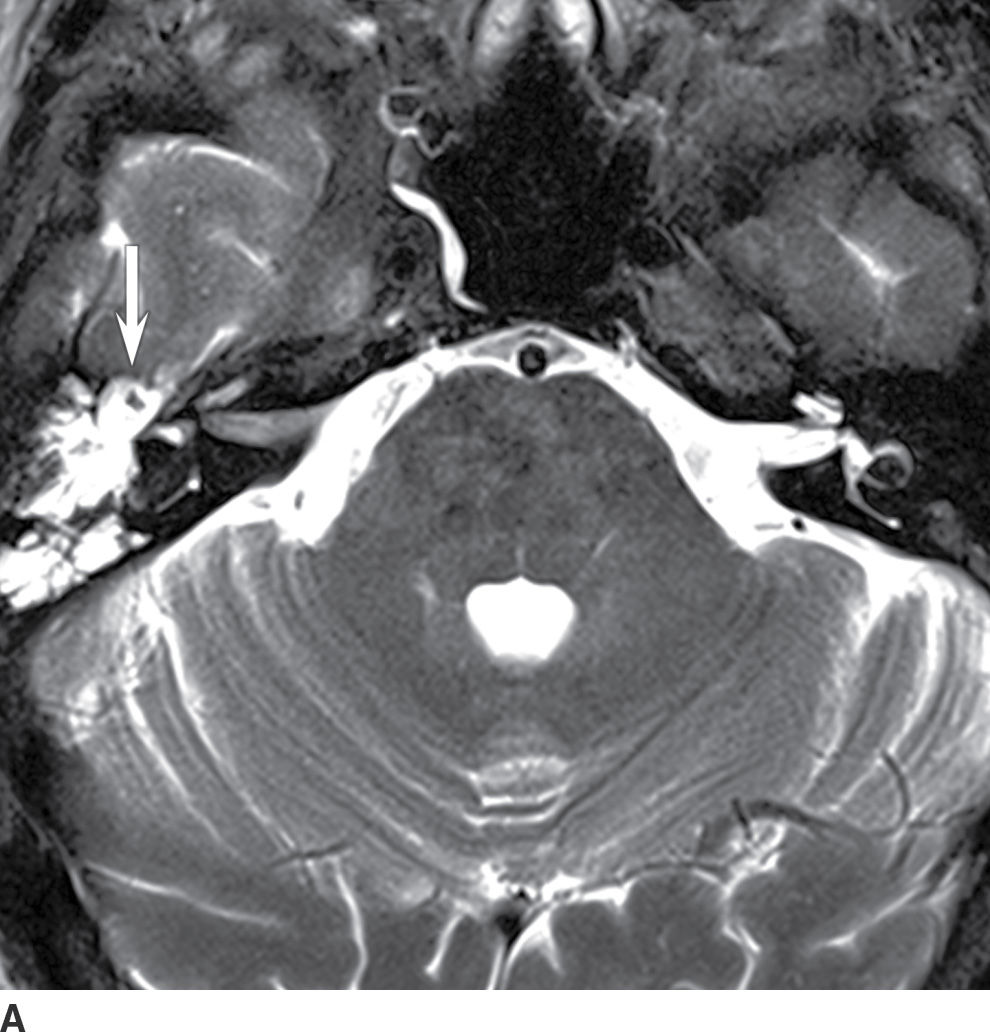

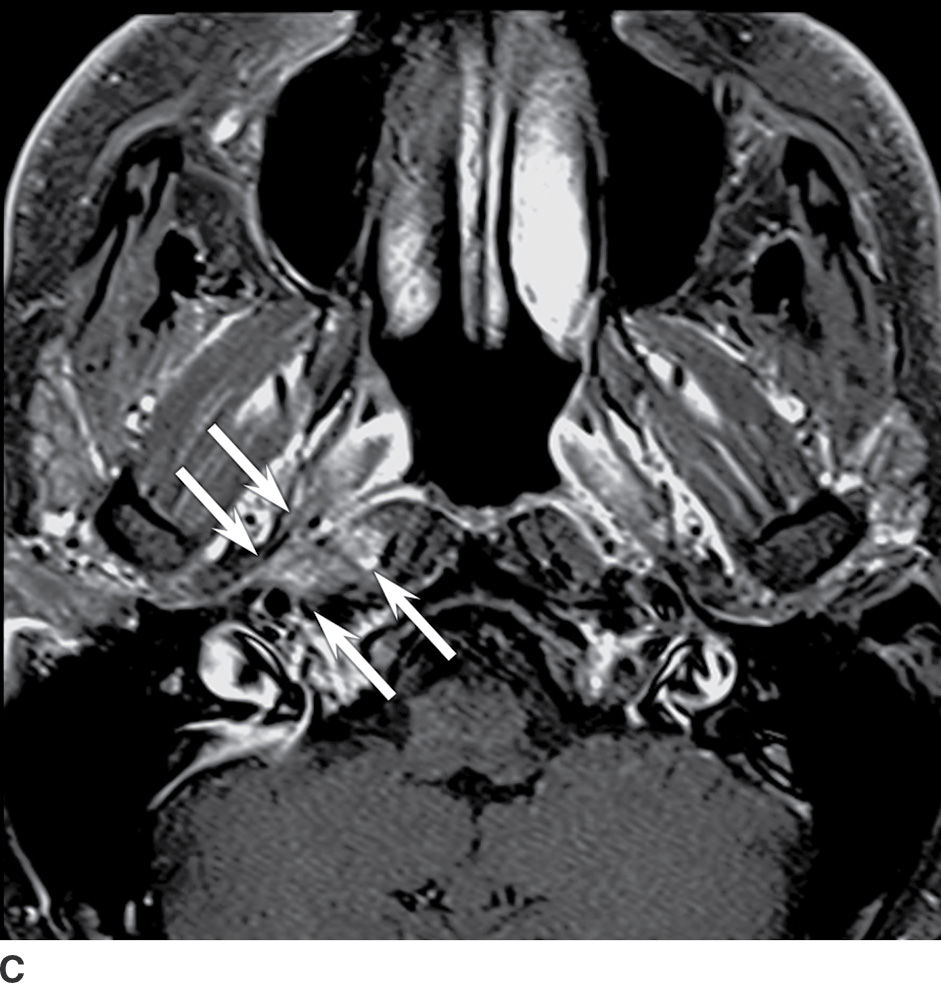
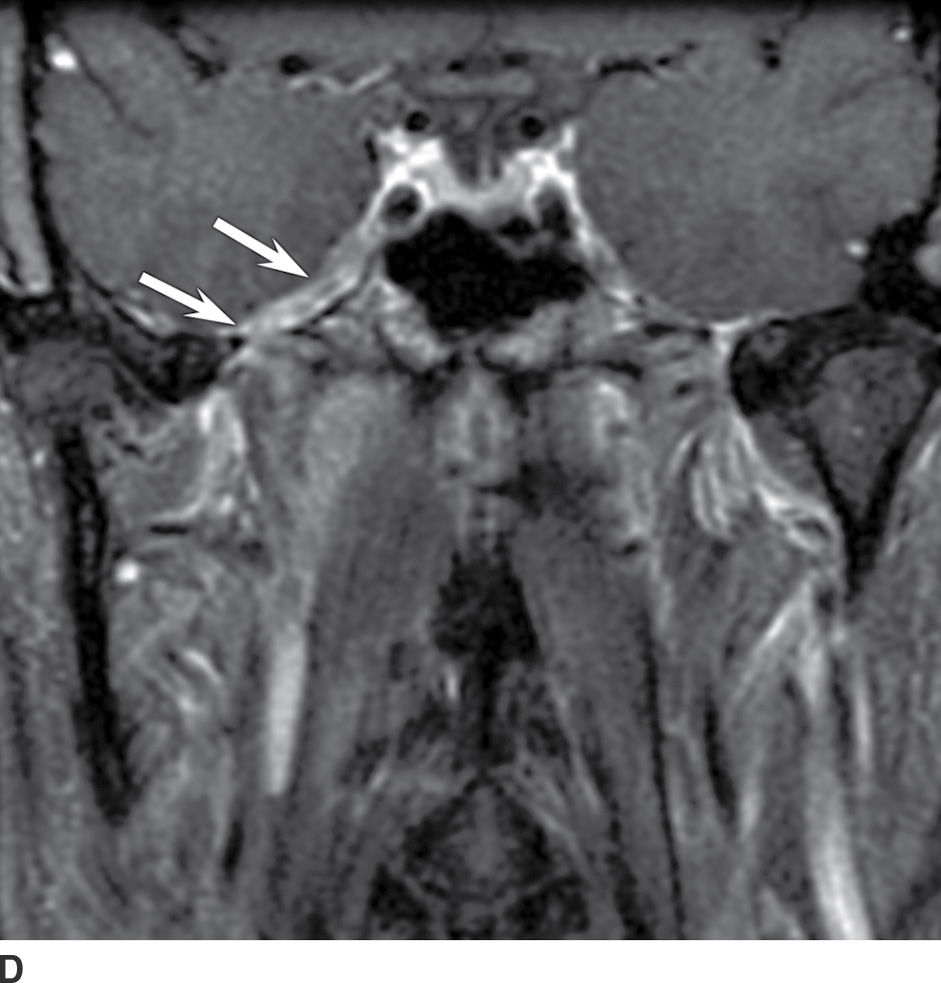
FIG. 24.13 Nasopharyngeal carcinoma. A 55-year-old man with right hearing loss and mandibular pain with perineural spread of tumor from small right nasopharyngeal carcinoma. A: Axial T2-weighted fat-suppressed MRI. A right mastoid and middle ear effusion (white arrow) indicate right eustachian tube dysfunction. B: Axial T1-weighted MRI. Asymmetric soft tissue fullness (arrowhead) is present in the right fossa of Rosenmuller, and there is adjacent abnormal infiltration of the soft tissue planes (arrows) just anterior to the right internal carotid artery when compared to the normal left side. C,D: Axial and coronal contrast-enhanced T1-weighted fat-suppressed MRIs, respectively. C: Contrast-enhanced MRI confirms an enhancing mass (arrows) extending deep to the right fossa of Rosenmuller. D: Perineural spread of tumor extends intracranially via the foramen ovale along the thickened third division of the trigeminal nerve (arrows).


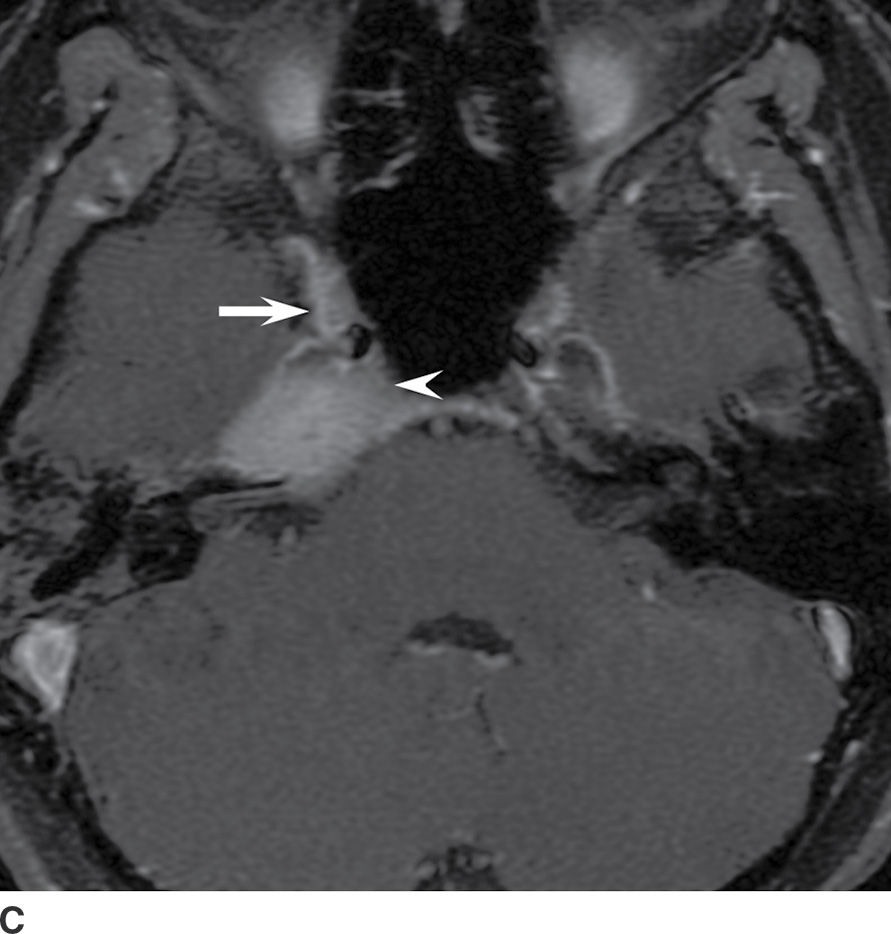
FIG. 24.14 Nasopharyngeal carcinoma. Axial T1- weighted MRI. A: Hypointense T1 signal in the right aspect of the clivus and right petrous apex (arrows) indicates tumor infiltration of the skull base bone marrow in this patient with biopsy-proven right nasopharyngeal carcinoma. B: Axial T1-weighted contrast-enhanced fat-suppressed MRI. The tumor invading the skull base avidly enhances (arrows) and surrounds the right internal carotid artery. C: Tumor extends into the inferior right cavernous sinus (arrow) and fills the right Meckel cave (arrowhead).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree