This is proportional to absorbed radiation dose independent of scan length. CTDIvolume (CTDIvol) is the dose variation in the Z plane related to spatial distance between adjacent scans and table speed, i.e., pitch, where pitch is the travel distance of the CT scanner table during a 360° rotation of the x-ray tube divided by x-ray beam collimation (equivalent to slice thickness). CTDIvol = CTDIw/pitch and is described in milligray (mGy) units. Therefore, when the pitch equals 1, then CTDIvol equals the CTDIw. Dose-length product (DLP) describes the length of the object being radiated and is proportional to the effective radiation dose. DLP = CTDIvol × length of radiated object and is described in mGy-cm units.
Multidetector CT (MDCT) Imaging
Multidetector CT (MDCT) imaging has been one of the most important recent advances in pediatric GU imaging [4]. Its short scan times have led to reductions in motion artifact and the avoidance of sedation. MDCT imaging also allows for the overlap of images from a single exposure, the reconstruction of images in different planes with creation of 3D projections, and the ability for precise timing of peak vascular and organ phase enhancement, which have led to major improvements in CT imaging for pediatric GU evaluation. As a result, MDCT imaging has greatly reduced the need for pediatric GU angiography. In addition, MDCT imaging provides subcentimeter resolution and therefore renders it more useful for pediatric GU tract imaging than MR imaging in this respect. Furthermore, bundled infants and children above 3 years of age can usually tolerate the short scans without the need for sedation, while children who may not be initially tolerant can often proceed through the short scan times with the help of parental coaching and avoid the need for sedation.
MDCT Technical Aspects
For MDCT imaging, the CT parameters should be set at ALARA (As Low As Reasonably Achievable) settings using weight or body mass index (BMI) criteria. The www.pedrad.org website can give up-to-date information on settings for a particular type of CT scanner. In general, patients less than 45 kg in weight need an 80 peak kilovoltage (kVp) dose setting, while larger patients need 100–120 kVp dose. The milliamperage (mAs) settings for abdominal CT imaging based on weight are as follows:
Weight <10 kg: 50 mAs
10–15 kg: 60 mAs
16–25 kg: 70 mAs
26–35 kg: 90 mAs
36–45 kg: 100 mAs
45 kg: >120 mAs
Since pitch is defined as the travel distance of the CT scanner table during a 360° rotation of the x-ray tube divided by x-ray beam collimation (equivalent to slice thickness), a patient’s typical radiation dose will be inversely related to the pitch. Pitches of 1–2, where the table feed is greater than the collimation, lead to decreases in radiation dosage by 50 % but with associated loss of resolution. For a 16-row MDCT scanner, the collimation is 0.75–1.5 mm with a pitch of 1–1.5. For a 64-row MDCT scanner, the collimation is 0.63 mm–1.25 mm with pitch of 1–1.5. CT scan times are usually set at 0.5 ms or less such that CT urography which includes the abdomen and the pelvis has scan times of less than a minute and often take only a few seconds. Although the axial slice thicknesses are often 0.63 mm or less, the images are often reconstructed at a wider thickness between 2.5 and 5 mm, which decreases noise artifact. Multiplanar reconstruction (MPR) in coronal and sagittal planes can provide additional information on the anatomy. Occasionally, maximum intensity projections (MIP) can be performed in the coronal plane and can provide intravenous pyelogram-like images. Three-dimensional (3D) thick slab reconstruction including 3D thick slab MIP imaging can also be performed if further anatomic detail is necessary.
Nonionic intravenous contrast is generally preferred over ionic contrast, since it is associated with less discomfort at the injection site and less risks for allergic reaction, nausea, vomiting, and flushing. Intravenous contrast can be given by hand injection or mechanical power injector, with an injection rate of 3–4 ml/s with 20-gauge intravenous access and 1–1.5 ml/s with 24-gauge intravenous access. The intravenous contrast dose in general is 2 ml/kg up to 125 ml maximum. Oral contrast can be a negative contrast agent (dark appearing) such as water or Pedialyte or a positive contrast agent (dense appearing) such as diluted Gastrografin or nonionic IV contrast material mixed with liquids such as water, juice, Gatorade, or soda. The positive contrast is mixed such that 15–30 ml of contrast is added to a total liquid volume of 1,000 ml and then prescribed to the patient for oral consumption with volumes based on age. The oral contrast volume is preferably given at least 1–2 h before the scan and additionally about 15 min prior to the scan as follows:
<1-month-old: 60–90 ml initially followed by 30–45 ml
1-month-old to 1-year-old: 120–240 ml initially followed by 60–120 ml
1–5-year-old: 240–480 ml initially followed by 120–180 ml
6–12-year-old: 480–1,000 ml initially followed by 180–500 ml
>12 years old: 1,000 ml initially followed by 500 ml
For optimal CT urography, the patient should void just prior to the scan or undergo bladder catheterization to eliminate functional effects on the renal parenchyma and collecting system due to transmitted bladder pressure effects.
MDCT Imaging Phases
Noncontrast CT imaging is often utilized to detect urinary tract stones and for characterization of a kidney lesion (calcification, simple cystic fluid, proteinaceous fluid, solid, etc.). If a lesion is less than 5 mm in diameter, the determination of some lesions can be less sensitive. In addition, noncontrast CT imaging can be used for suspected bladder perforation to separate out radiodense fluid such as blood and other radiodense material from extravasated contrast during a CT cystogram study.
When intravenous contrast is used, there are usually four phases of contrast CT urography: the arterial phase begins between 15 and 25 s after the injection with delineation of the arteries. This phase can be programmed as a timed bolus or as a “bolus trigger” where the CT scanner begins scanning once the attenuation readings of the aorta hit a threshold value of 120 Hounsfield units (HU). In this phase, there may be early renal cortex enhancement as well. The corticomedullary phase (cortical phase) begins approximately 30–40 s after the injection and corresponds with the late arterial phase with sharp cortical enhancement and visually nondetectable or minimal medullary enhancement (Fig. 3.1). This phase is used to assess veins, arteries, renal masses, cysts, infection, and trauma. However, it is not entirely reliable in visualizing some masses or infections, including fungal infections. The nephrogenic phase (medullary or tubular phase) begins approximately 75–120 s from the start of contrast injection and is the most reliable for the assessment of parenchymal lesions (Fig. 3.2). However, this phase may not allow detection of early enhancing lesions such as renal cell carcinoma foci or certain vascular malformations. In this phase, there is uniform parenchymal enhancement throughout the kidneys without excretion into the pelvicalyceal system. In addition, urothelial pathology can occasionally be appreciated during this phase as well as during the corticomedullary phase. The excretory phase occurs approximately 3–5 min after injection, but a longer scan time delay until 5–15 min after injection can be utilized to allow for improved visualization of the pelvicalyceal system and ureters. The parenchymal enhancement decreases during this phase, which is often helpful in assessing anatomic anomalies, obstructing lesions of the collecting system and ureters, noncalcified filling defects, and urothelial pathology.
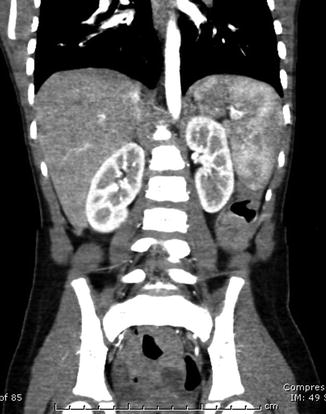

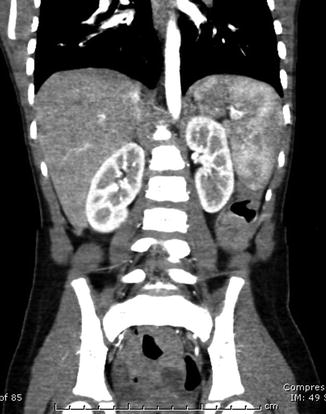
Fig. 3.1
Contrast CT image of the kidneys – early phase

Fig. 3.2
Contrast CT image of the kidneys – late phase
Anatomy/Variations
Examples of CT imaging in the genitourinary tract have been included below. Subsequent chapters will provide further imaging details by organ system.
CT imaging of the GU tract usually involves the recognition of normal relevant anatomy and its variations. The renal margins may be smooth or lobulated (fetal lobulations) in areas of renicular fusion, where fetal lobulations can be differentiated from renal scarring in that they maintain their overall cortical thickness. The perinephric fat is generally minimal in children. The renal capsule usually cannot be separately identified from the rest of the renal tissue by CT. The renal arteries branch from the aorta just below the superior mesenteric artery and split into its dorsal and ventral branches at the hilum. The renal veins are usually anterior to the arteries with the left renal vein coursing anterior to the aorta before reaching the inferior vena cava, although vascular anomalies are possible such as a retroaortic left renal vein anomaly or the “nutcracker” compression anomaly of the left renal vein between the superior mesenteric artery and the aorta which may be a source of hematuria. Prominent enhancing columns of Bertin that are identified as potential renal masses sonographically can be differentiated by CT as normal enhancing parenchyma. Though perinephric fat is usually minimal in children, it can become more prominent in children on steroid therapy, obese patients, immobile patients, patients with neuromuscular disorders, and patients with metabolic disorders. The perinephric fascia (Gerota’s fascia) surrounds the space containing kidney, adrenal gland, renal pelvis, and proximal ureter. The posterior pararenal space is marked by the posterior renal fascia, psoas, and quadratus muscle, while the anterior pararenal space is bordered by the posterior parietal peritoneum, lateral conal fascia, and anterior renal fascia. The ureters course anteromedial to the psoas muscle in the abdominal cavity. In the pelvis, at a level just below the iliac vessel bifurcation near the level of the iliac crest, the ureters drape over the iliac artery initially and then course medial to the iliac vessels, which are medial to the iliopsoas muscle, before entering the trigone area of the bladder posteriorly.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree