George M. Bridgeforth and Kris Alden
A 63-year-old man has redness, warmth, swelling, and severe pain affecting his wrists and his hands. He complains of pain, swelling, and redness in both knees as well.
CLINICAL POINTS
- Rheumatoid arthritis (RA) is a chronic inflammatory disease.
- Women are more likely than men to develop RA.
- Morning stiffness is a common complaint.
Clinical Presentation
More than 2 million Americans have the chronic inflammatory disease rheumatoid arthritis (RA). Women are affected more than men; the female-to-male ratio is approximately 3:1. Although individuals of any age can develop RA, most cases typically occur between the ages of 25 and 55 years. RA is an autoimmune arthritic condition, and its exact cause is unclear. Principally a joint disease, RA also has systemic manifestations, such as weight loss, low-grade fever, and malaise.
Affected joints are swollen, tender, and warm. Patients may complain of morning stiffness, with limited movement. A polyarthritis, RA usually involves the small joints of the hands, feet, and cervical spine but may also affect large joints such as the shoulders and knees. (Patients with RA may be prone to life-threatening cervical subluxations with minor cervical trauma. It is imperative to assume cervical instability until proven otherwise and to use a spine board and a hard cervical collar.) An important feature is the presence of a periarticular osteoporosis that not only involves the metacarpals and the proximal interphalangeal (PIP) joints, but there is some involvement of the distal interphalangeal (DIP) joints as well.
Clinicians use seven criteria to diagnose RA. At least four of the seven criteria must be met (Box 51.1).
Unlike gout and psoriatic arthritis, RA is usually a symmetrical arthritis. It can involve the upper cervical spine, hands, wrists, elbows, knees, ankles, and sacroiliac joints. Unlike osteoarthritis, which involves the DIP joints, RA has predilection for the carpal (wrist), metacarpals, and PIP joints. In the latter stages, there may be involvement of the DIP joints as well. Also, unlike osteoarthritis, RA is not characterized by prominent subchondral sclerosis or osteophyte formation at the joint margins. When these latter two findings are present (especially at the DIP joints of the hands), it indicates a concomitant osteoarthritis.
Radiographic Evaluation
Usually an examiner would like a minimum of three views of any affected area. Optional tests include a cervical computed tomography scan with contrast (for cervical trauma) to rule out atlantoaxial instability (Fig. 51.1).
Box 51.1 Diagnostic Criteria for Rheumatoid Arthritis (RA)*
Morning stiffness of the joints that lasts for at least 1 hour.
Arthritis in three or more joint areas. At least three joints demonstrate soft tissue swelling or fluid accumulation that has been verified by a physician. The possible areas of involvement are the proximal interphalangeal (PIP) joints, metacarpophalangeal (MCP) joints, wrist, elbow, knee, ankle, and metatarsophalangeal joints.
Arthritis affecting the joints of the hand, with at least one swollen area affecting the wrist, MCP, or PIP joint.
Symmetric arthritis. Bilateral arthritis affecting the same joints listed in item 2—the inflammatory changes do not have to be identical. (Although it is uncommon, there is an asymmetric form of RA.)
Rheumatoid nodules. The presence of subcutaneous nodules over bony prominences, extensor surfaces, or juxta-articular regions, verified by a physician.
Positive (serum) rheumatoid factor.
Radiographic changes secondary to RA identified on the posteroanterior hand and wrist radiographs.
* The first four criteria must be present for at least 6 weeks.

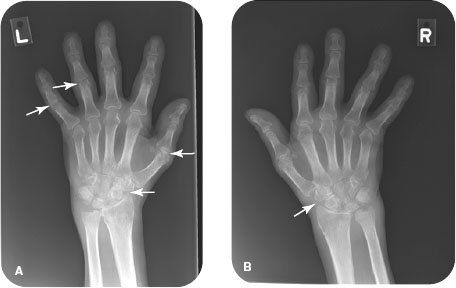
FIGURE 51.1 A 69-year-old man with rheumatoid arthritis on an (A) AP, (B) oblique, and (C) lateral projections. Notice the uniform loss of the PIP joint spaces from the right second through fifth digits (arrow). On the oblique projection there is erosion of the ulnar styloid (arrowhead).

FIGURE 51.2 A 66-year-old man with advanced rheumatoid arthritis. Anteroposterior radiographs of the (A) left and (B) right hands demonstrate diffuse osteopenia, proximal periarticular soft tissue swelling (arrows), marginal erosions (arrowheads), and ulnar deviation of the right fourth and fifth MCP joints. Also note widening of the scapholunate interval and proximal migration of the capitate in the left hand (circled) compatible with scapholunate advance collapse (SLAC).
PATIENT ASSESSMENT 
- Redness, warmth, and swelling of the wrists, metacarpals, PIP joints, knees, ankles, and elbows
- Moderate disease: ulnar deviation of the hands; hypertrophy of the metacarpals, PIP joints, and knees
- Advanced disease: joint erosions with permanent joint deformities (pannus formation), swan neck and boutonniere deformities
- Deformities of the hands
- Hypertrophy with severely impaired range of motion of the wrists, hands, and knees
NOT TO BE MISSED 
- Osteoarthritis
- Psoriatic arthritis
- Gout
- Fractures/contusions
- Septic joint
- Collagen vascular disease (systemic lupus erythematosus, scleroderma)
With early RA, there is an ulnar deviation of the wrists associated with a nonspecific soft tissue swelling (Fig. 51.2). With advanced RA, there is extensive erosive destruction of the carpal bones. Commonly associated findings include boutonniere and swan neck deformities of the fingers. Moreover, there is joint space narrowing with marginal erosions of the PIP joint. Hallmarks of early RA include soft tissue swelling with periarticular osteoporosis (Fig. 51.3). With joint space narrowing there are marginal erosions (i.e., erosions at the corners of the joints). More advanced involvement can lead subluxations of the metacarpals; these subluxations result in the ulnar deviation of the hand seen on clinical and radiological examinations. Boutonnière and swan neck deformities are classic findings in advanced RA. With a boutonnière deformity, there is prominent flexion at the PIP joint and extension of the DIP joint. Inflammation of the PIP joint results in a synovitis with elongation of the lateral bands. The resulting inflammation leads to attenuation and volar subluxation of the lateral bands (and triangular ligaments). The volar subluxation of the lateral bands exerts a downward force on the PIP joint; the end result is a characteristic flexion deformity of the PIP joint. With a swan neck deformity, the opposite configuration is characteristic. There is hyperextension of the PIP joint with flexion of the DIP joint. There is damage to the extensor mechanism at the DIP joint. Moreover, stretching and inflammatory damage to the volar plate (with an associated tendon imbalance) produces a hyperextension deformity at the PIP joint (Fig. 51.4).
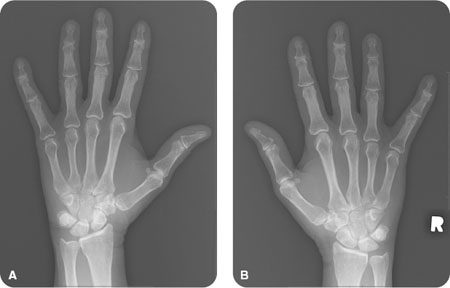
FIGURE 51.3 A 49-year-old female with rheumatoid arthritis demonstrating periarticular osteopenia, an early phase of the disease process.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








