George M. Bridgeforth, Shane J. Nho, Rachel M. Frank, and Brian J. Cole
AN 83-year-old woman who fell from a treadmill now complains of pain and soreness in both shoulders.

CLINICAL POINTS
- Most shoulder displacements occur in an anterior– inferior direction.
- Posterior dislocations are uncommon, and inferior dislocations (luxatio erecta) are rare.
- Gross dislocations may be associated with rotator cuff tears.
Clinical Presentation
A shoulder dislocation occurs at the glenohumeral joint when the humerus separates from the scapula (Fig. 30.1). The shoulder’s great range of motion makes it especially susceptible to dislocation, and it is the most commonly dislocated joint. Shoulder dislocations have a bimodal incidence; they occur more frequently in younger men and older women. The cause of most of these dislocations is generally a direct force applied to the arm; this force could result from a fall or a collision with another person or object.
Approximately 95% of all shoulder dislocations are anteroinferior. Posterior dislocations are uncommon, and pure inferior dislocations are rare. Most anteroinferior dislocations are characterized by displacement of the humeral head. Signs and symptoms include:
- Difficulty with arm movement together with impaired range of motion
- Marked pain
- Numbness of the arm
- Palpable gap in the subdeltoid region
Tears of the rotator cuff contribute to shoulder instability and may occur in shoulder dislocation. Patients with rotator cuff tears, with or without an associated dislocation, have impaired range of motion with a positive drop arm test—an inability to sustain abduction (in which the arm is raised laterally) against resistance. The ability to abduct the arm to 90 to 120 degrees with limited resistance may indicate a partial tear or strain of a rotator cuff. The presence of limited extension (i.e., in which the arm is placed behind the shoulder) and weak external rotation (in which the forearm is rotated away from the body against resistance) commonly signifies complete tears of the rotator cuff. Supraspinatus tendinopathy also results unimpaired abduction and marked pain with resistance.
It is always important to rule out cervical disc disease, because a C5 radiculopathy can mimic or be associated with a shoulder injury. Patients with a C5 radiculopathy have a positive Spurling’s test (cervical pain with axial compression), pain-limited cervical pain, and sensory loss along the lateral deltoid. In advanced cases, deltoid function may be pain limited and mimic a shoulder injury. Patients with C6 radiculopathies have numbness of the thumb and forefinger (Hoppenfeld’s “six shooter”). C7 radiculopathies present with numbness to the middle finger, and C8 radiculopathies are characterized by cervical pain and numbness that radiates to the little finger. More advanced cases (C8 radiculopathy) demonstrate triceps weakness (elbow extension) with an impaired triceps reflex.
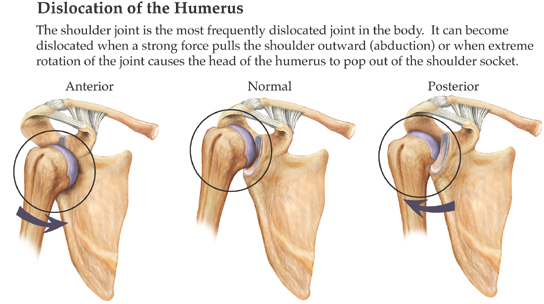
FIGURE 30.1 Anatomy and injuries of the shoulder. Instability. Dislocation of the humerus. Asset provided by Anatomical Chart Co.
Posterior dislocations account for less than 5% of all shoulder dislocations. Unlike anterior–inferior dislocations, they can be missed on the clinical examination. It is strongly recommended that clinicians obtain a “Y” view (see section, “Radiographic Evaluation”).
Radiographic Evaluation
An anteroposterior (AP) view, AP view with internal rotation, and “Y” (transscapular) view (used in acute trauma to determine whether there is an anterior or posterior dislocation of the humerus; Fig. 30.2) should be ordered. An axillary view is optional (some physicians prefer an axillary view to a “Y” view to rule out a shoulder dislocation).
PATIENT ASSESSMENT 
- Marked pain and tenderness
- Inability to abduct the affected arm (i.e., raise the arm away from the body)
- The arm is adducted at the shoulder and flexed at the elbow
Normally, the humeral head fits into the glenoid fossa like a golf ball on a tee. The golf ball analogy is very important. In a normal radiograph, a plumb line (a downward vertical line dropped at a 90 degree angle from a point on a horizontal plane) that goes directly below the coracoid process should lie medial to the humeral head. The head of the displaced humerus lies directly inferior to the coracoid process as the dislocated humeral head crosses the scapula. Note the anterior and inferior displacement of the humeral head. It lies medial to the glenoid rim and below the glenoid fossa as well.
The overwhelming majority of anterior dislocations are identified on the standard AP and AP view with internal rotation. If the head of the humerus lies inside and inferior to the glenoid fossa, the examiner should immediately suspect a shoulder dislocation. However, some shoulder dislocations, especially posterior dislocations, are best identified on the “Y” view. In this projection, the anterior arm of the “Y” is formed by the coracoid process, and the posterior arm of the “Y” is formed by the acromion. Normally, the long axis of the humerus should bisect the “Y” (Fig. 30.2). The long axis of the humerus clearly lies in front of the “Y”. Therefore, the “Y” view provides additional evidence of an anterior dislocation. On the other hand, with a posterior dislocation, the long axis of the humerus would lie behind the “Y”.
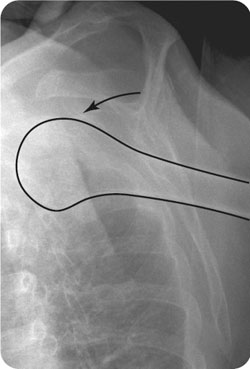
FIGURE 30.2 Scapular “Y” view of the left shoulder, demonstrating anterior shoulder dislocation from the patient in the introductory case. Note that on the anteroposterior view shown at the beginning of the chapter, the shoulder is inferiorly displaced and that the scapular “Y” view confirms and anterior dislocation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








